Abstract
Background
Previous experimental research has reported minimal differences in pressure maintenance between different versions of standard insufflators (SI). However, a recent report identified potential clinical benefits with a valveless pressure barrier insufflator (PBI). We sought to perform a benchtop objective evaluation of SI and PBI systems.
Methods
A rigid box system with continuous pressure manometry was used to evaluate a PBI (Surgiquest Airseal) and two SIs (SI1 = Stryker PneumoSure High Flow Insufflator and SI2 = Storz SCB Thermoflator). Pressure maintenance of 15 mmHg was evaluated during experimental conditions of leakage from a 5 mm port site, leakage from a 12 mm port site, and continuous suction.
Results
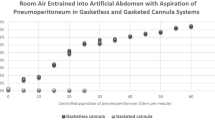
With leakage from the 5 mm port site, the PBI maintained pressure of >13 mmHg whereas the pressures dropped moderately with the SI1 (7–13 mmHg) and SI2 insufflators (3–7 mmHg) and did not regain goal pressure until leakage was stopped. With leakage from 12 mm port site, the PBI pressure decreased to 9–11 mmHg, whereas the SI1 and SI2 lost insufflation pressures completely. The PBI maintained pressure of >11 mmHg during continuous suction while the SI1 and SI2 lost pressure entirely, and actually showed negative pressure from air suction into the rigid box system. When evaluated statistically with the mixed model repeated measures ANOVA, the SI1 and SI2 performed similarly while the PBI maintained increased pressure.
Conclusions
In the experimental rigid box system, the PBI more successfully maintained pressure in response to leakage and suction than SIs.





Similar content being viewed by others
References
Barbash GI, Glied SA (2010) New technology and health care costs—the case of robot-assisted surgery. N Engl J Med 363:701–704
Miller DC, Wei JT, Dunn RL, Hollenbeck BK (2006) Trends in the diffusion of laparoscopic nephrectomy. JAMA 295:2480–2482
Jacobs VR, Morrison JE Jr, Kiechle M (2004) Twenty-five simple ways to increase insufflation performance and patient safety in laparoscopy. J Am Assoc Gynecol Laparosc 11:410–423
Jacobs VR, Kiechle M, Morrison JE Jr (2005) Carbon dioxide gas heating inside laparoscopic insufflators has no effect. JSLS 9:208–212
Birch DW, Manouchehri N, Shi X, Hadi G, Karmali S (2011) Heated CO(2) with or without humidification for minimally invasive abdominal surgery. Cochrane Database Syst Rev 19(1):CD007821
Lawrentschuk N, Fleshner NE, Bolton DM (2010) Laparoscopic lens fogging: a review of etiology and methods to maintain a clear visual field. J Endourol 24:905–913
Jacobs VR, Morrison JE Jr, Paepke S, Fischer T, Kiechle M (2006) Three-dimensional model for gas flow, resistance, and leakage-dependent nominal pressure maintenance of different laparoscopic insufflators. J Minim Invasive Gynecol 13:225–230
Jacobs VR, Morrison JE Jr (2007) The real intraabdominal pressure during laparoscopy: comparison of different insufflators. J Minim Invasive Gynecol 14:103–107
Herati AS, Atalla MA, Rais-Bahrami S, Andonian S, Vira MA, Kavoussi LR (2009) A new valve-less trocar for urologic laparoscopy: initial evaluation. J Endourol 23:1535–1539
Herati AS, Andonian S, Rais-Bahrami S, Atalla MA, Srinivasan AK, Richstone L, Kavoussi LR (2011) Use of the valveless trocar system reduces carbon dioxide absorption during laparoscopy when compared with standard trocars. Urology 77:1126–1132
Jacobs VR, Morrison JE Jr, Mundhenke C, Golombeck K, Jonat W, Harder D (2000) Model to determine resistance and leakage-dependent flow on flow performance of laparoscopic insufflators to predict gas flow rate of cannulas. J Am Assoc Gynecol Laparosc 7:331–337
Shafer DM, Khajanchee Y, Wong J, Swanstrom LL (2006) Comparison of five different abdominal access trocar systems: analysis of insertion force, removal force, and defect size. Surg Innov 13:183–189
Verdaasdonk EG, Stassen LP, van der Elst M, Karsten TM, Dankelman J (2007) Problems with technical equipment during laparoscopic surgery. An observational study. Surg Endosc 21:275–279
Disclosures
The authors Kenneth G. Nepple, Dorina Kallogjeri and Sam B. Bhayani have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nepple, K.G., Kallogjeri, D. & Bhayani, S.B. Benchtop evaluation of pressure barrier insufflator and standard insufflator systems. Surg Endosc 27, 333–338 (2013). https://doi.org/10.1007/s00464-012-2434-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2434-x