Abstract
Background
Sexual and urinary dysfunction is an established risk after pelvic surgery. Studies examining sexual and urinary function following laparoscopic and open rectal surgery give conflicting evidence for outcomes. The purpose of this study was to analyse the impact of the surgical technique on functional outcomes following laparoscopic or open resection for rectal cancer patients in a high-volume laparoscopic unit.
Methods
All patients who underwent elective laparoscopic or open surgery for rectal cancer between September 2006 and September 2009 were identified from a prospectively collated database. Validated standardized postal questionnaires were sent to surviving patients to assess their postoperative sexual and urinary function. The functional data were then quantified using previously validated indices of function.
Results
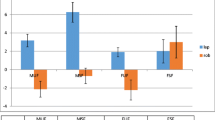
A total of 173 patients were identified from the database, of whom 144 (83 %) responded to the questionnaire-based study. Seventy-eight respondents had undergone laparoscopic rectal resection (49 men and 29 women), and 65 had an open procedure (41 men and 24 women). Both open surgery and laparoscopic surgery were associated with deterioration in urinary and sexual function. With regard to urinary function, there was no difference in the deterioration in open and laparoscopic groups in either gender. With regard to sexual function, in males one component of sexual function, namely, the incidence of successful penetration, showed less deterioration in the laparoscopic group (p = 0.04). However, in females, laparoscopic surgery was associated with significantly better outcomes in all aspects of sexual activity, specifically sexual arousal (p = 0.005), lubrication (p = 0.001), orgasm (p = 0.04), and the incidence of dyspareunia (p = 0.02).
Conclusion
Laparoscopic total mesorectal excision for rectal cancer is associated with significantly less deterioration in sexual function compared with open surgery. This effect is particularly pronounced in women.
Similar content being viewed by others
References
Marescaux J, Rubino F, Leroy J (2005) Laparoscopic total mesorectal excision for rectal cancer surgery. Dig Dis 23:135–141
McCourt M, Armitage J, Monson JR (2009) Rectal cancer. Surgeon 7:162–169
Aziz O, Constantinides V, Tekkis P, Athanasiou T, Purkayastha S, Paraskeva P, Darzi AW, Heriot AG (2006) Laparoscopic versus open surgery for rectal cancer: a meta-analysis. Ann Surg Oncol 13:413–424
Maas CP, Moriya Y, Steup WH, Kiebert GM, Kranenbarg WM, van de Velde CJ (1998) Radical and nerve-preserving surgery for rectal cancer in The Netherlands: a prospective study on morbidity and functional outcome. Br J Surg 85:92–97
Mundy AR (1982) An anatomical explanation for bladder dysfunction following rectal and uterine surgery. Br J Urol 54:501–504
Lindsey I, Mortensen NJ (2002) Iatrogenic impotence and rectal dissection. Br J Surg 89:1493–1494
Morino M, Parini U, Allaix ME, Monasterolo G, Brachet Contul R, Garrone C (2009) Male sexual and urinary function after laparoscopic total mesorectal excision. Surg Endosc 23:1233–1240
Quah HM, Jayne DG, Eu KW, Seow-Choen F (2002) Bladder and sexual dysfunction following laparoscopically assisted and conventional open mesorectal resection for cancer. Br J Surg 89:1551–1556
Jayne DG, Brown JM, Thorpe H, Walker J, Quirke P, Guillou PJ (2005) Bladder and sexual function following resection for rectal cancer in a randomized clinical trial of laparoscopic versus open technique. Br J Surg 92:1124–1132
Heald RJ (1979) A new approach to rectal cancer. Br J Hosp Med 22:277–281
Heald RJ, Husband EM, Ryall RD (1982) The mesorectum in rectal cancer surgery: the clue to pelvic recurrence? Br J Surg 69:613–616
Kehlet H, Wilmore DW (2002) Multimodal strategies to improve surgical outcome. Am J Surg 183:630–641
Denis L, Griffiths K, Khoury S (1998) Measuring the symptom and health impact of benign prostatic hyperplasia and its treatment. In: Denis L, Griffiths K, Khoury S et al (eds) 4th international consultation on benign prostatic hyperplasia. World Health Organization, Health Publication Ltd, Paris, p 265–280
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A (1997) The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 49:822–830
Kelleher CJ, Cardozo LD, Khullar V, Salvatore S (1997) A new questionnaire to assess the quality of life of urinary incontinent women. BJOG 104:1374–1379
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D’Agostino R Jr (2000) The female sexual function index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 26:191–208
Hemandas AK, Abdelrahman T, Flashman KG, Skull AJ, Senapati A, O’Leary DP, Parvaiz A (2010) Laparoscopic colorectal surgery produces better outcomes for high risk cancer patients compared to open surgery. Ann Surg 252:84–89
Frasson M, Braga M, Vignali A, Zuliani W, Di Carlo V (2008) Benefits of laparoscopic colorectal resection are more pronounced in elderly patients. Dis Colon Rectum 51:296–300
Böhm G, Kirschner-Hermanns R, Decius A, Heussen N, Schumpelick V, Willis S (2008) Anorectal, bladder, and sexual function in females following colorectal surgery for carcinoma. Int J Colorectal Dis 23:893–900
Disclosures
Ms. E. R. McGlone, Mr. O. Khan, Ms. K. Flashman, Mr. J. Khan, and Professor A. Parvaiz have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McGlone, E.R., Khan, O., Flashman, K. et al. Urogenital function following laparoscopic and open rectal cancer resection: a comparative study. Surg Endosc 26, 2559–2565 (2012). https://doi.org/10.1007/s00464-012-2232-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2232-5