Abstract
Background
Laparoscopic cholecystectomy is considered nowadays as the standard management of acute cholecystitis (AC). However, results from multicentric studies in the general surgical community are still lacking.
Methods
A prospective multicenter survey of surgical management of AC patients was conducted over a 2-year period in Belgium. Operative features and patients’ clinical outcome were recorded. The impact of independent predictive factors on the choice of surgical approach, the risk of conversion, and the occurrence of postoperative complications was studied by multivariate logistic regression analysis.
Results
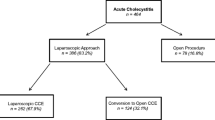
Fifty-three surgeons consecutively and anonymously included 1,089 patients in this prospective study. A primary open approach was chosen in 74 patients (6.8%), whereas a laparoscopic approach was the first option in 1,015 patients (93.2%). Independent predictive factors for a primary open approach were previous history of upper abdominal surgery [odds ratio (OR) 4.13, p < 0.001], patient age greater than 70 years (OR 2.41, p < 0.05), surgeon with more than 10 years’ experience (OR 2.08, p = 0.005), and gangrenous cholecystitis (OR 1.71, p < 0.05). In the laparoscopy group, 116 patients (11.4%) required conversion to laparotomy. Overall, 38 patients (3.5%) presented biliary complications and 49 had other local complications (4.5%). Incidence of bile duct injury was 1.2% in the whole series, 2.7% in the open group, and 1.1% in the laparoscopy group. Sixty patients had general complications (5.5%). The overall mortality rate was 0.8%. All patients who died were in poor general condition [American Society of Anesthesiologists (ASA) III or IV].
Conclusions
Although laparoscopic cholecystectomy is currently considered as the standard treatment for acute cholecystitis, an open approach is still a valid option in more advanced disease. However, overall mortality and incidence of bile duct injury remain high.
Similar content being viewed by others
References
Sauerland S, Agresta F, Bergamachi R, Borzellino G, Budzynski A, Champault G, Fingerhut A, Isla A, Johansson M, Lundorff P, Navez B, Saad S, Neugebauer EA (2006) Laparoscopy for abdominal emergencies: evidence-based guidelines of the European Association for Endoscopic Surgery. Surg Endosc 20(1):14–29
Gurusamy K, Samraj K, Gluud C, Wilson E, Davidson BR (2010) Meta-analysis of randomized controlled trials on the safety and effectiveness of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg 97(2):141–150
David GG, Al-Sarira AA, Willmott S, Deakin M, Corless DJ, Slavin JP (2008) Management of acute gallbladder disease in England. Br J Surg 95(4):472–476
Navez B, Mutter D, Russier Y, Vix M, Jamali F, Lipski D, Cambier E, Guiot P, Leroy J, Marescaux J (2001) Safety of laparoscopic approach for acute cholecystitis: retrospective study of 609 cases. World J Surg 25(10):1352–1356
Pessaux P, Tuech JJ, Rouge C, Duplessis R, Cervi C, Arnaud JP (2000) Laparoscopic cholecystectomy in acute cholecystitis. A prospective comparative study in patients with acute vs. chronic cholecystitis. Surg Endosc 14(4):358–361
Martin M, Abrams M, Arkin R, Ballen P, Blievernicht S, Bowman W, Davis T, Farley R, Hoxworth B, Ingram H, Lindsey A, Leone M, Newman D, Price T, Streck C, Weatherly W, Young P (1993) Safe laparoscopic cholecystectomy in a community setting, N = 762. Surg Endosc 7(4):300–303
Kolla SB, Aggarwal S, Kumar A, Kumar R, Chumber S, Parshad R, Seenu V (2004) Early vs delayed laparoscopic cholecystectomy for acute cholecystitis: a prospective randomized trial. Surg Endosc 18(9):1323–1327
Glavic Z, Begic L, Simlesa D, Rukavina A (2001) Treatment of acute cholecystitis. A comparison of open vs laparoscopic cholecystectomy. Surg Endosc 15(4):398–401
Gigot J, Etienne J, Aerts R, Wibin E, Dallemagne B, Deweer F, Fortunati D, Legrand M, Vereecken L, Doumont J, Van Reepinghen P, Beguin C (1997) The dramatic reality of biliary tract injury during laparoscopic cholecystectomy. An anonymous multicenter Belgian survey of 65 patients. Surg Endosc 11(12):1171–1178
Fitzgibbons RJ Jr, Tseng A, Wang H, Ryberg A, Nguyen N, Sims KL (1996) Acute cholecystitis. Does the clinical diagnosis correlate with the pathological diagnosis? Surg Endosc 10(12):1180–1184
Schrenk P, Woisetschläger R, Rieger R, Wayand WU (1998) A diagnostic score to predict the difficulty of a laparoscopic cholecystectomy from preoperative variables. Surg Endosc 12(2):148–150
Giger UF, Michel JM, Opitz I, Th Inderbitzin D, Kocher T, Krähenbühl L (2006) Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy: analysis of 22,953 consecutive cases from the Swiss Association of Laparoscopic and Thoracoscopic Surgery database. J Am Coll Surg 203(5):723–728
Kanaan SA, Murayama KM, Merriam LT, Dawes LG, Prystowsky JB, Rege RV, Joehl RJ (2002) Risk factors for conversion of laparoscopic to open cholecystectomy. J Surg Res 106(1):20–24
Borzellino G, Sauerland S, Minicozzi AM, Verlato G, Di Pietrantonj C, de Manzoni G, Cordiano C (2008) Laparoscopic cholecystectomy for severe acute cholecystitis. A meta-analysis of results. Surg Endosc 22(1):8–15
Yol S, Kartal A, Vatansev C, Aksoy F, Toy H (2006) Sex as a factor in conversion from laparoscopic cholecystectomy to open surgery. JSLS 10(3):359–363
Brodsky A, Matter I, Sabo E, Cohen A, Abrahamson J, Eldar S (2000) Laparoscopic cholecystectomy for acute cholecystitis: can the need for conversion and the probability of complications be predicted?. A prospective study. Surg Endosc 14(8):755–760
Lau H, Lo Y, Patil NG, Yuen WK (2006) Early versus delayed-interval laparoscopic cholecystectomy for acute cholecystitis. A meta-analysis. Surg Endosc 20(1):82–87
Siddiqui T, MacDonald A, Chong PS, Jenkins JT (2008) Early versus delayed laparoscopic cholecystectomy for acute cholecystitis : a meta-analysis of randomized clinical trials. Am J Surg 195(1):40–47
Nuzzo G, Giuliante F, Giovannini I, Ardito F, D’Acapito F, Vellone M, Murazio M, Capelli G (2005) Bile duct injury during laparoscopic cholecystectomy: results of an Italian national survey on 56 591 cholecystectomies. Arch Surg 140(10):986–992
Regöly-Mérei J, Ihász M, Szeberin Z, Sándor J, Máté M (1998) Biliary tract complications in laparoscopic cholecystectomy. A multicenter study of 148 biliary tract injuries in 26,440 operations. Surg Endosc 12(4):294–300
Flum DR, Koepsell T, Heagerty P, Sinanan M, Dellinger EP (2001) Common bile duct injury during laparoscopic cholecystectomy and the use of intraoperative cholangiography: adverse outcome or preventable error? Arch Surg 136(11):1287–1292
Suter M, Meyer A (2001) A 10-year experience with the use of laparoscopic cholecystectomy for acute cholecystitis: is it safe ? Surg Endosc 15(10):1187–1192
Nakajima J, Sasaki A, Obuchi T, Baba S, Nitta H, Wakabayashi G (2009) Laparoscopic subtotal cholecystectomy for severe cholecystitis. Surg Today 39(10):870–875
Tian Y, Wu SD, Su Y, Kong J, Yu H, Fan Y (2009) Laparoscopic subtotal cholecystectomy as an alternative procedure designed to prevent bile duct injury: experience of a hospital in northern China. Surg Today 39(6):510–513
Horiuchi A, Watanabe Y, Doi T, Sato K, Yukumi S, Yoshida M, Yamamoto Y, Sugishita H, Kawachi K (2008) Delayed laparoscopic subtotal cholecystectomy in acute cholecystitis with severe fibrotic adhesions. Surg Endosc 22(12):2720–2723
Hubert C, Annet L, van Beers BE, Gigot JF (2010) The “inside approach of the gallbladder” is an alternative to the classic Calot’s triangle dissection for a safe operation in severe cholecystitis. Surg Endosc 24(10):2626–2632
Beldi G, Glättli A (2003) Laparoscopic subtotal cholecystectomy for severe cholecystitis. Surg Endosc 17(9):1437–1439
Johansson M, Thune A, Nelvin L, Stiernstam M, Westman B, Lundell L (2005) Randomized clinical trial of open versus laparoscopic cholecystectomy in the treatment of acute cholecystitis. Br J Surg 92(1):44–49
Kim JH, Kim JW, Jeong IH, Choi TY, Yoo BM, Kim JH, Kim MW, Kim WH (2008) Surgical outcomes of laparoscopic cholecystectomy for severe acute cholecystitis. J Gastrointest Surg 12(5):829–835
Acknowledgments
The following members of BGES are gratefully acknowledged for their substantial contributions to the present study: Drs. Jacques Baillieux (Hornu), Jean Beaurang (Willebroek), Michel Bourdon (Libramont), Emmanuel Cambier (Gilly), Bernard Dallemagne (Liège), Georges Decker (Luxembourg), Robert De Keulenner (Auvelais), Didier Deltour (Gosselies), Olivier Dockx (Marche), Raphael Droissart (Brussels), Mary-Lou Druart (deceased) (Brussels), Pierre Guiot (Gilly), Dominique Herman (Libramont), Jean-Luc Jourdan (Liège), Fadi Maassarani (Auvelais), Bernard Majerus (Ottignies), Baudouin Mansvelt (Jolimont), Pierre Mendes Da Costa (Brussels), Benoit Monami (Liège), Karel Mulier (Leuven), Christian Ngongang (Marche), Jacques Peeters (Waremme), Pascal Remy (Hornu), Casper Sommeling (Waregem), Pierre Taziaux (Malmedy), Musa Tugilimana (Ath), and Etienne Veys (Gosselies). The authors also wish to thank Prof C. de Burbure for revising the manuscript.
Disclosures
Authors Benoit Navez, Felicia Ungureanu, Martens Michiels, Julie Navez, Donald Claeys, Filip Muysoms, Catherine Hubert, Marc Vanderveken, Olivier Detry, Bernard Detroz, Jean Closset, Bart Devos, Marc Kint, Francis Zech, and Jean-François Gigot have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Navez, B., Ungureanu, F., Michiels, M. et al. Surgical management of acute cholecystitis: results of a 2-year prospective multicenter survey in Belgium. Surg Endosc 26, 2436–2445 (2012). https://doi.org/10.1007/s00464-012-2206-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2206-7