Abstract
Background
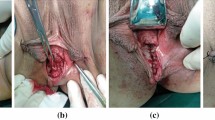
Rectovaginal fistulas (RVFs) are a rare surgical condition. Their treatment is extremely difficult, and no standard surgical technique is accepted worldwide. This report describes a new approach using transanal endoscopic microsurgery (TEM) to treat RVFs.
Methods
A retrospective review of 13 patients who underwent repair of rectovaginal fistula using TEM between 2001 and 2008 was undertaken. The surgical technique is widely described, and the advantages of the endorectal approach are noted.
Results
The median follow-up period was 25 months, and the median age of the patients was 44 years (range, 25–70 years). The mean operative time was 130 min (range, 90–150 min), and the hospital stay was 5 days (range, 3–8 days). One patient experienced recurrence. This patient underwent reoperation with TEM and experienced re-recurrence. Two patients had minor complications (hematoma of the septum and abscess of the septum), which were treated with medical therapy. For two patients, a moderate sphincter hypotonia was registered.
Conclusions
A new technique for treating RVFs using TEM is presented. The authors strongly recommend this approach that avoids any incision of the perineal area, which is very painful and can damage sphincter functions.



Similar content being viewed by others
References
Kosugi C, Saito N, Kimata Y, Ono M, Sugito M, Ito M, Sato K, Koda K, Miyazaki M (2005) Rectovaginal fistulas after rectal cancer surgery: incidence and operative repair by gluteal-fold flap repair. Surgery 137:329–336
Kumaran SS, Palanivelu C, Kavalakat AJ, Parthasarathi R, Neelayathatchi M (2005) Laparoscopic repair of high rectovaginal fistula: is it technically feasible? BMC Surg 5:20
Walfisch A, Zilberstein T, Walfisch S (2004) Rectovaginal septal repair: case presentations and introduction of a modified reconstruction technique. Tech Coloproctol 8:192–194
Chitrathara K, Namratha D, Francis V, Gangadharan VP (2001) Spontaneous rectovaginal fistula and repair using bulbocavernosus muscle flap. Tech Coloproctol 5:47–49
Oom DM, Gosselink MP, Van Dijl VR, Zimmerman DD, Schouten WR (2006) Puborectal sling interposition for the treatment of rectovaginal fistulas. Tech Coloproctol 10:125–130 (discussion 130, Epub 19 June 2006)
Sonoda T, Hull T, Piedmonte MR, Fazio VW (2002) Outcomes of primary repair of anorectal and rectovaginal fistulas using the endorectal advancement flap. Dis Colon Rectum 45:1622–1628
McCraw JB, Massey FM, Shankilin KD, Horton CE (1976) Vaginal reconstruction with gracilis myocutaneous flaps. Plast Reconstr Surg 58:176
Cardon A, Pattyn P, Monstrey S, Hesse U, de Hemptinne B (1999) Use of a unilateral pudendal thigh flap in the treatment of complex rectovaginal fistula. Br J Surg 86:645–646
Gurlek A, Gherardini G, Coban YK, Gorgu M, Erdogan B, Evans GR (1997) The repair of multiple rectovaginal fistulas with the neurovascular pudendal thigh flap (Singapore flap). Plast Reconstr Surg 99:2071–2073
Wee JT, Joseph VT (1989) A new technique of vaginal reconstruction using neurovascular pudendal thigh flaps: a preliminary report. Plast Reconstr Surg 83:701
Monstrey S, Blondeel P, Van Landuyt K, Verpaele A, Tonnard P, Matton G (2001) The versatility of the pudendal thigh fasciocutaneous flap used as an island flap. Plast Reconstr Surg 107:719–725
Hagerty RC, Vaughn TR, Lutz MH (1988) The perineal artery axial flap in reconstruction of the vagina. Plast Reconstr Surg 82:344–345
Gleeson NC, Baile W, Roberts WS, Hoffman MS, Fiorica JV, Finan MA et al (1994) Pudendal thigh fasciocutaneous flaps for vaginal reconstruction in gynecologic oncology. Gynecol Oncol 54:269–274
Woods JE, Alter G, Meland B, Podratz K (1992) Experience with vaginal reconstruction utilizing the modified Singapore flap. Plast Reconstr Surg 90:270
Soper JT, Larson D, Hunter VJ, Berchuck A, Clarke-Pearson DL (1989) Short gracilis myocutaneous flaps for vulvovaginal reconstruction after radical pelvic surgery. Obstet Gynecol 74:823
Tobin GR, Day TG (1988) Vaginal and pelvic reconstruction with distally based rectus abdominis myocutaneous flaps. Plast Reconstr Surg 81:62
Niazi ZB, Kogan SJ, Petro JA, Salzberg CA (1998) Abdominal composite flap for vaginal reconstruction. Plast Reconstr Surg 101:249
Cerna B, Rus J (1992) Repair of a vaginal defect with a musculocutaneous flap. Acta Chir Plast 34:38–43
Emirogiu M, Gultan SM, Adanali G, Apaydin I, Yormuk E (1996) Vaginal reconstruction with free jejunal flap. Ann Plast Surg 36:316–320
Pinedo G, Phillips R (1998) Labial fat pad grafts (modified Martius graft) in complex perianal fistulas. Ann R Coll Surg Engl 80:410–412
Wexner SD, Ruiz DE, Genua J, Nogueras JJ, Weiss EG, Zmora O (2008) Gracilis muscle interposition for the treatment of rectourethral, rectovaginal, and pouch-vaginal fistulas: results in 53 patients. Ann Surg 248:39–43
Ruiz D, Bashankaev B, Speranza J, Wexner SD (2008) Graciloplasty for rectourethral, rectovaginal, and rectovesical fistulas: technique overview, pitfalls, and complications. Tech Coloproctol 12:277–281 (discussion 281–282, Epub 5 August 2008)
Vávra P, Andel P, Dostalík J, Gunková P, Pelikán A, Gunka I, Martínek L, Vávrová M, Spurný P, Curík R, Koliba P (2006) The first case of management of the rectovaginal fistule using transanal endocsopic microsurgery. Rozhl Chir 85:82–85
Vàvra P, Dostalik J, Vavrova M, Gunkova P, Pai M, El-Gendi A, Habib N, Papaevangelou A (2009) Transanal endoscopic microsurgery: a novel technique for the repair of benign rectovaginal fistula. Surgeon 7:126–127
Darwood RJ, Borley NR (2008) TEMS: an alternative method for the repair of benign rectovaginal fistulae. Colorectal Dis 10:619–620 (Epub 21 February 2008)
Disclosures
Giancarlo D’Ambrosio, Alessandro Paganini, Mario Guerrieri, Luciana Barchetti, Giovanni Lezoche, Emanuele Lezoche, and Bernardina Fabiani have no conflicts of interests or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
D’Ambrosio, G., Paganini, A.M., Guerrieri, M. et al. Minimally invasive treatment of rectovaginal fistula. Surg Endosc 26, 546–550 (2012). https://doi.org/10.1007/s00464-011-1917-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1917-5