Abstract
Objective
This article was designed to systematically analyze the prospective, randomized, controlled trials on the effectiveness of staple-line reinforcement (SLR) in patients undergoing laparoscopic gastric bypass (LGBP) surgery.
Methods
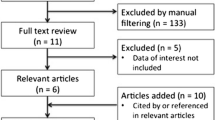
Trials on the effectiveness of SLR in patients undergoing LGBP surgery were selected electronic data bases and analyzed to generate summative data by using the principles of meta-analysis on statistical software package RevMan 5.0.2 provided by Cochrane Collaboration. Combined outcome of the binary variables was expressed as odds ratio (OR) and continuous variables were expressed as standardized mean difference (SMD).
Results
Three randomized, controlled trails on 180 patients qualified for inclusion. There were 91 patients in SLR group and 89 patients in non-staple-line reinforcement (NSLR) group. There was no heterogeneity among trials. In the fixed-effects model, SLR is equivalent to NSLR in terms of controlling bleeding (odds ratio (OR), 0.32; 95% confidence interval (CI), 0.03, 3.18; z = 0.98; P < 0.33) from the staple-line and total number of staples used (standardized mean difference (SMD), −21.01; 95% CI, −56.46, 14.44; z = 1.16; P < 0.25) for anastomosis. SLR significantly reduces operative time (SMD, −0.76; 95% CI, −1.36, −0.16; z = 2.47; P < 0.01), perioperative complications (OR, 0.19; 95% CI, 0.05, 0.68; z = 2.55; P < 0.01), anastomotic leak (OR, 0.1; 95% CI, 0.01, 0.78; z = 2.2; P < 0.03), and hemostatic clips (SMD, −21.01; 95% CI, −56.46, 14.44; z = 1.16; P < 0.25) usage.
Conclusions
SLR seems to reduce the operative time in LGBP. In addition, SLR is associated with fewer postoperative complications, reduced incidence of anastomotic leak, and reduced requirement of hemostatic clips to control hemorrhage at the staple line. However, SLR does not have any superiority in terms of controlling staple-line bleeding and does not influence the number of staples used in LGBP.







Similar content being viewed by others
References
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292:1724–1737
Saber AA, Scharf KR, Turk AZ, Elgamal MH, Martinez RL (2008) Early experience with intraluminal reinforcement of stapled gastrojejunostomy during laparoscopic Roux-en-Y gastric bypass. Obes Surg 18:525–529
Gagner M, Garcia-Ruiz A, Arca MJ (1999) Laparoscopic isolated gastric bypass for morbid obesity. Surg Endosc S19:6
Higa KD, Boone KB, Ho T (2000) Complications of the laparoscopic Roux-en-Y gastric bypass: 1, 040 patients–what have we learned? Obes Surg 10:509–513
Schauer PR, Ikramuddin S, Gourash W, Ramanathan R, Luketich J (2000) Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Ann Surg 232:515–529
Wittgrove AC, Clark GW (2000) Laparoscopic gastric bypass, Roux-en-Y 500 patients: technique and results, with 3–60 month follow-up. Obes Surg 10:233–239
MacLean LD, Rhode BM, Nohr C, Katz S, McLean AP (1997) Stomal ulcer after gastric bypass. J Am Coll Surg 185:1–7
Mehran A, Szomstein S, Zundel N, Rosenthal R (2003) Management of acute bleeding after laparoscopic Roux-en-Y gastric bypass. Obes Surg 13:842–847
Nguyen NT, Rivers R, Wolfe BM (2003) Early gastrointestinal hemorrhage after laparoscopic gastric bypass. Obes Surg 13:62–65
Luján JA, Frutos MD, Hernández Q, Liron R, Cuenca JR, Valero G, Parrilla P (2004) Laparoscopic versus open gastric bypass in the treatment of morbid obesity: a randomized prospective study. Ann Surg 239:433–437
Madan AK, Martinez JM, Lo Menzo E, Khan KA, Tichansky DS (2009) Omental reinforcement for intraoperative leak repairs during laparoscopic Roux-en-Y gastric bypass. Am Surg 75:839–842
Basu NN, Leschinskey D, Heath DI (2008) The use of Seamguard to buttress the suture repair of a staple line leak following laparoscopic gastric bypass for obesity. Obes Surg 8:896–897
Angrisani L, Lorenzo M, Borrelli V, Ciannella M, Bassi UA, Scarano P (2004) The use of bovine pericardial strips on linear stapler to reduce extraluminal bleeding during laparoscopic gastric bypass: prospective randomized clinical trial. Obes Surg 14:1198–1202
Fullum TM, Aluka KJ, Turner PL (2009) Decreasing anastomotic and staple line leaks after laparoscopic Roux-en-Y gastric bypass. Surg Endosc 23:1403–1408
Assalia A, Ueda K, Matteotti R, Cuenca-Abente F, Rogula T, Gagner M (2007) Staple-line reinforcement with bovine pericardium in laparoscopic sleeve gastrectomy: experimental comparative study in pigs. Obes Surg 17:222–228
Shikora SA, Kim JJ, Tarnoff ME (2008) Comparison of permanent and nonpermanent staple line buttressing materials for linear gastric staple lines during laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 4:729–734
Thomas P, Massard G, Porte H, Doddoli C, Ducrocq X, Conti M (2006) A new bioabsorbable sleeve for lung staple-line reinforcement (FOREseal): report of a three-center phase II clinical trial. Eur J Cardiothorac Surg 29:880–885
de la Portilla F, Zbar AP, Rada R, Vega J, Cisneros N, Maldonado VH, Utrera A, Espinosa E (2006) Bioabsorbable staple-line reinforcement to reduce staple-line bleeding in the transection of mesenteric vessels during laparoscopic colorectal resection: a pilot study. Tech Coloproctol 10:335–338
Cheragwandi A, Nieuwenhuis DH, Gagner M, Consten EC (2008) An update of available innovative staple line reinforcement materials in colorectal surgery. Surg Technol Int 17:131–137
Higgins JPT, Green S (eds) (2008) Cochrane handbook for systematic reviews of interventions, Version 5.0.0 (updated February 2008). The Cochrane Collaboration http://www.cochrane-handbook.org. Accessed 7 March 2010
Review Manager (RevMan) [computer program] (2008) Version 5.0. The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
DeMets DL (1987) Methods for combining randomized clinical trials: strengths and limitations. Stat Med 6:341–350
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Egger M, Smith GD, Altman DG (2006) Systematic reviews in healthcare. BMJ Publishing, London
Deeks JJ, Altman DG, Bradburn MJ (2001) Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. Systemic reviews in health care: meta-analysis in context, 2nd edn. BMJ Publishing, London
Miller KA, Pump A (2007) Use of bioabsorbable staple reinforcement material in gastric bypass: a prospective randomized clinical trial. Surg Obes Relat Dis 3:417–421
Nguyen NT, Longoria M, Welbourne S, Sabio A, Wilson SE (2005) Glycolide copolymer staple-line reinforcement reduces staple site bleeding during laparoscopic gastric bypass: a prospective randomized trial. Arch Surg 140:773–778
Baker RS, Foote J, Kemmeter P, Brady R, Vroegop T, Serveld M (2004) The science of stapling and leaks. Obes Surg 14:1290–1298
Liu CD, Glantz GJ, Livingston EH (2003) Fibrin glue as a sealant for high-risk anastomosis in surgery for morbid obesity. Obes Surg 13:45–48
Arnold W, Shikora SA (2005) A comparison of burst pressure between buttressed versus non-buttressed staple-lines in an animal model. Obes Surg 15:164–171
Pinheiro JS, Correa JL, Cohen RV, Novaes JA, Schiavon CA (2006) Staple line reinforcement with new biomaterial increased burst strength pressure: an animal study. Surg Obes Relat Dis 2:397–399
Downey DM, Harre JG, Dolan JP (2005) Increased burst pressure in gastrointestinal staple-lines using reinforcement with a bioprosthetic material. Obes Surg 15:1379–1383
Ibele A, Garren M, Gould J (2010) Effect of circular staple line buttressing material on gastrojejunostomy failure in laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 6:64–67
Callery CD, Filiciotto S, Neil KL (2010) Collagen matrix staple line reinforcement in gastric bypass. Surg Obes Relat Dis [Epub ahead of print]
Disclosures
M. S. Sajid, K. Khatri, K. Singh, M. Sayegh have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sajid, M.S., Khatri, K., Singh, K. et al. Use of staple-line reinforcement in laparoscopic gastric bypass surgery: a meta-analysis. Surg Endosc 25, 2884–2891 (2011). https://doi.org/10.1007/s00464-011-1637-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1637-x