Abstract
Background
This prospective study aimed to evaluate the impact of transabdominal preperitoneal patch plasty (TAPP) with implantation of a lightweight mesh (<50 g/m²) fixed by fibrin glue on the occurrence of chronic pain and sexual dysfunction in hernia patients.
Methods
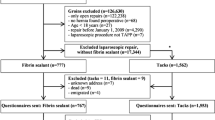
Patients were examined before TAPP, early and late postoperatively. The primary end point of the study was pain-related functional impairment 6 months after the operation as assessed by the validated assessment scale (AAS). For the first time, patients without any pain before surgery were compared with patients experiencing preoperative pain. Furthermore, the patients were asked about the frequency and extent of impairment in their sexual activities. A secondary end point was chronic pain in relation to the type of mesh fixation (glue vs clip).
Results
The study criteria was met by 276 patients. The dropout rate after 6 months was 2.9%. Mesh fixation was performed with glue for 212 patients and with clip for 64 patients. Chronic pain with significant impairment of daily activities was experienced by 42% of patients before the operation, which decreased to 8.3% after TAPP. The mean level of impairment, assessed by AAS, decreased from 11.2 preoperatively to 2 postoperatively (p < 0.001). The clip patients had more pain on days 4 and 7 postoperatively (p < 0.05) but not later. A majority of the patients (78%) experiencing pain before the operation were pain free 6 months after TAPP. New pain was seen in 7.4% of the patients but was only mild (numeric analog scale [NAS], 1–3; 78% of patients) or moderate (NAS, 4–6; 11% of patients). The only patient with severe pain (NAS, 8) had a clip fixation. Frequency of sexual dysfunction decreased after TAPP (p < 0.05).
Conclusion
The TAPP procedure with implantation of a lightweight mesh fixed by glue is a highly effective option for preventing chronic pain in inguinal hernia repair. Fibrin fixation seems superior to clip fixation during the early postoperative period. However, for confirmation of results, a randomized study is recommended.
Similar content being viewed by others
References
Van Veen RN, Wijsmuller AR, Vrijland WW, Hop WC, Lange JF, Jeekel J (2007) Long-term follow-up of a randomized clinical trial of non-mesh versus mesh repair of primary inguinal hernia. Br J Surg 94:506–510
Bay-Nielsen M, Nielsen E, Nordin P, Kehlet H (2007) Chronic pain after open mesh and sutured repair of indirect inguinal hernia in young males. Br J Surg 91:1372–1376
Nienhuijs S, Staal E, Stobbe L, Rosman C, Groenewoud H, Bleichrodt R (2007) Chronic pain after mesh repair of inguinal hernia: a systematic review. Am J Surg 194:394–400
Aasvang EK, Brandsborg B, Christensen B, Jensen TS, Kehlet H (2008) Neurophysiological characterization of postherniotomy pain. Pain 137:173–181
Bittner R, Schmedt CG, Schwarz J, Kraft K, Leibl BJ (2002) Laparoscopic transperitoneal procedure for routine repair of groin hernia. Br J Surg 89:1062–1066
Bittner R (2003) Transabdominal preperitoneal approach. In: LeBlanc KA (ed) Laparoscopic hernia surgery. Arnold, London
Bittner R (2006) Standardtechnik der transabdominellen präperitonealen Patchplastik (TAPP). In: Bittner R, Leibl BJ, Ulrich M (eds) Chirurgie der Leistenhernie. Karger, Freiburg
Amid PK, Hiatt JR (2007) New understanding of the causes and surgical treatment of postherniorrhaphy inguinodynia and orchalgia. J Am Coll Surg 205:381–385
Bay-Nielsen M, Perkins FM, Kehlet H (2001) Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg 233:1–7
International Association for the Study of Pain (1986) Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl 3:1–226
McCarthy M Jr, Jonasson O, Chang CH, Pickard SA, Giobbie-Hurder A, Gibbs J et al (2005) Assessment of patient functional status after surgery. J Am Coll Surg 201:171–178
Fujita F, Lahmann B, Otsuka K, Lyass S, Hiatt JR, Phillips EH (2004) Quantification of pain and satisfaction following laparoscopic and open hernia repair. Arch Surg 139:596–602
Junge K, Rosch R, Klinge U, Schwab R, Peiper C, Binnebösel M et al (2006) Risk factors related to recurrence in inguinal hernia repair: a retrospective analysis. Hernia 10:309–315
Cunningham J, Temple WJ, Mitchell P, Nixon JA, Preshaw RM, Hagen NA (1996) Cooperative hernia study: pain in the postrepair patient. Ann Surg 224:598–602
Poobalan AS, Bruce J, King PM, Chambers WA, Krukowski ZH, Smith WCS (2001) Chronic pain and quality of life following open inguinal hernia repair. Br J Surg 88:1122–1126
Aasvang EK, Kehlet H (2005) Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth 95:69–76
Post S, Weiss B, Willer M, Neufang T, Lorenz D (2004) Randomized clinical trial of lightweight composite mesh for Lichtenstein inguinal hernia repair. Br J Surg 91:44–48
O’Dwyer PJ, Kingsnorth AN, Molloy RG, Small PK, Lammers B, Horeyseck G (2005) Randomized clinical trial assessing impact of a lightweight or heavyweight mesh on chronic pain after inguinal hernia repair. Br J Surg 92:166–170
Bringman S, Wollert S, Österberg J, Smedberg S, Granlund H, Heikkinen TJ (2006) Three-year results of a randomized clinical trial of lightweight or standard polypropylene mesh in Lichtenstein repair of primary inguinal hernia. Br J Surg 93:1056–1059
Heikkinen TJ, Wollert S, Österberg J, Smedberg S, Bringman S (2006) Early results of a randomised trial comparing Prolene and Vyproll mesh in endoscopic extraperitoneal inguinal hernia repair (TEP) of recurrent unilateral hernias. Hernia 10:34–40
Langenbach MR, Schmidt J, Zirngibl H (2006) Comparison of biomaterials: three meshes and TAPP for inguinal hernia. Surg Endosc 20:1511–1517
Champault G, Bernard C, Rizk N, Polliand C (2007) Inguinal hernia repair: the choice of prosthesis outweighs that of technique. Hernia 11:125–128
Hernia The EU, Collaboration Trialists (2002) Repair of groin hernia with synthetic mesh: metaanalysis of randomized controlled trials. Ann Surg 235:322–332
Schmedt CG, Sauerland S, Bittner R (2005) Comparison of endoscopic procedures vs Lichtenstein and other open mesh techniques for inguinal hernia repair: a metaanalysis of randomized controlled trials. Surg Endosc 19:188–199
Aasvang EK, Mohl B, Bay-Nielsen M, Kehlet H (2006) Pain related sexual dysfunction after inguinal herniorraphy. Pain 122:258–263
Broin EO, Horner C, Mealy K, Kerin MJ, Gillen P, O’Brien M et al (1995) Meralgia paraesthetica following laparoscopic inguinal hernia repair: an anatomical analysis. Surg Endosc 9:76–78
Rosenberger RJ, Loeweneck H, Meyer G (2000) The cutaneous nerves encountered during laparoscopic repair of inguinal hernia. Surg Endosc 14:731–735
Taylor C, Layani L, Liew V, Ghusn M, Crampton N, White S (2008) Laparoscopic inguinal hernia repair without mesh fixation: early results of a large randomised clinical trial. Surg Endosc 22:757–762
Lowham AS, Filipi JC, Fitzgibbons RJ, Stoppa R, Wantz GE, Felix EL et al (1997) Mechanisms of hernia recurrence after preperitoneal mesh repair. Ann Surg 225:422–431
Katkhouda N, Mavor E, Friedlander MH, Mason RJ, Kiyabu M, Grant SW et al (2001) Use of fibrin sealant for prosthetic mesh fixation in laparoscopic extraperitoneal inguinal hernia repair. Ann Surg 233:18–25
Lau H (2005) Fibrin sealant versus mechanical stapling for mesh fixation during endoscopic extraperitneal inguinal hernioplasty: a randomized prospective trial. Ann Surg 242:670–675
Lovisetto F, Zonta S, Rota E, Mazzilli M, Bardone M, Bottero L et al (2007) Use of human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty. Ann Surg 245:222–231
Olmi S, Scaini A, Erba L, Guaglio M, Croce E (2007) Quantification of pain in laparoscopic transabdominal preperitoneal (TAPP) inguinal hernioplasty identifies marked differences between prosthesis fixation systems. Surgery 152:40–46
Schug-Pass C, Lippert H, Köckerling F (2009) Mesh fixation with fibrin glue (Tissucol/Tisseel) in hernia repair dependent on mesh structure: is there an optimum fibrin–mesh combination? Investigations on a biomechanical model. Langenbecks Arch Surg (Epub ahead of print 31 January)
Acknowledgments
The biometrics was done in cooperation with the Institut for Biometrics, University of Tübingen (uni-tübingen.de\biometrie). The study was funded by a grant from Aesculap AG (Tuttlingen, Germany), Baxter Deutschland GmbH (Unterschleißheim, Germany), and the Lundback Foundation (Denmark) to cover the cost (room, materials, psychologists). Neither physician fees or royalties nor patient reimbursements were provided. In addition, none of the authors has any direct or indirect financial interest in the products.
Disclosures
Reinhard Bittner, Eliza Gmähle, Björn Gmähle, Jochen Schwarz, Eske Aasvang, and Henrik Kehlet have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bittner, R., Gmähle, E., Gmähle, B. et al. Lightweight mesh and noninvasive fixation: an effective concept for prevention of chronic pain with laparoscopic hernia repair (TAPP). Surg Endosc 24, 2958–2964 (2010). https://doi.org/10.1007/s00464-010-1140-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1140-9