Abstract
Background
The face of surgery has changed over the past two decades with the introduction of laparoscopic techniques. The majority of surgical specialties now perform minimally invasive procedures hence decreasing the scarring, pain, and infection historically associated with open surgery. To further reduce the invasiveness of surgery, new surgical techniques like Natural Orifice Transluminal Endoscopic Surgery (NOTES) and Single-Port Surgery (SPS) are under development. Despite investment from the medical device industry and enthusiasm from medical professionals, we must analyse patient preferences and expectations of these novel techniques. This analysis will help us establish the demand for such techniques and guide future resource allocation.
Methods
A questionnaire-based study was derived to identify whether the concepts of innovative techniques are acceptable to the general population. Their preferences between different available surgical options were recorded along with their choices for new innovative techniques. This study was carried out face-to-face and by using an online survey. It comprised four questions based upon a hypothetical scenario of an acute appendicitis. All the data were captured in a prospective database and analysed using statistical software.
Results
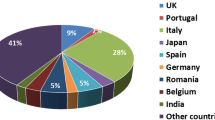
A total of 750 participants from variable backgrounds took part in the study. NOTES or SPS without an established safety profile was accepted by 34.3% of patients. SPS was the most popular method followed by conventional laparoscopy. Open surgery and NOTES were the least preferred (ranked 1.78, 1.98, 2.94, and 3.27, respectively). Choosing between SPS and NOTES only, 80.6% opted for SPS, 11.8% NOTES, and 5.6% declined surgery. The most popular route of access for NOTES is oral (37.7%).
Conclusion
Single-port surgery was the most preferred method and NOTES was the least preferred technique. This shows general acceptance of the concept of virtually scarless surgery but without using the natural orifices.









Similar content being viewed by others
References
Litynski GS (1999) Profiles in laparoscopy: Mouret, Dubois, and Perissat: the laparoscopic breakthrough in Europe (1987–1988). J Soc Laparoendosc Surg 3(2):163–167
Finkelberg DL, Wassef W (2008) Natural orifice translumenal surgery: from scales to symphonies. Curr Opin Gastroenterol 24(6):674–681
Horgan S, Cullen JP, Talamini MA, Mintz Y, Ferreres A, Jacobsen GR, Sandler B, Bosia J, Savides T, Easter DW, Savu MK, Ramamoorthy SL, Whitcomb E, Agarwal S, Lukacz E, Dominguez G, Ferraina P (2009) Natural orifice surgery: initial clinical experience. Surg Endosc 23(7):1512–1518
Horgan S, Mintz Y, Jacobsen GR, Sandler BJ, Cullen JP, Spivack A, Easter DW, Chock A, Savu MK, Ramamoorthy S, Bosia J, Agarwal S, Lukacz E, Whitcomb E, Savides T, Talamini MA (2009) Video. NOTES: transvaginal cholecystectomy with assisting articulating instruments. Surg Endosc 23(8):1900
Colvin SB, Grossi EA, Galloway AC (2000) Regarding ethics of rapid surgical technological advancement. Ann Thorac Surg 70(5):1758
Voermans RP, Worm AM, van Berge Henegouwen MI, Breedveld P, Bemelman WA, Fockens P (2008) In vitro comparison and evaluation of seven gastric closure modalities for natural orifice transluminal endoscopic surgery (NOTES). Endoscopy 40(7):595–601
von Delius S, Gillen S, Doundoulakis E, Schneider A, Wilhelm D, Fiolka A, Wagenpfeil S, Schmid RM, Feussner H, Meining A (2008) Comparison of transgastric access techniques for natural orifice transluminal endoscopic surgery. Gastrointest Endosc 68(5):940–947
ASGE/SAGES (2006) ASGE/SAGES Working Group on Natural Orifice Translumenal Endoscopic Surgery White Paper October 2005. Gastrointest Endosc 63(2):199–203
Romanelli JR, Mark L, Omotosho PA (2008) Single port laparoscopic cholecystectomy with the TriPort system: a case report. Surg Innov 15(3):223–228
Piskun G, Rajpal S (1999) Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech A 9(4):361–364
Kosumi T, Kubota A, Usui N, Yamauchi K, Yamasaki M, Oyanagi H (2001) Laparoscopic ovarian cystectomy using a single umbilical puncture method. Surg Laparosc Endosc Percutan Tech 11(1):63–65
Kaouk JH, Palmer JS (2008) Single-port laparoscopic surgery: initial experience in children for varicocelectomy. BJU Int 102(1):97–99
Gill IS, Canes D, Aron M, Haber GP, Goldfarb DA, Flechner S, Desai MR, Kaouk JH, Desai MM (2008) Single port transumbilical (E-NOTES) donor nephrectomy. J Urol 180(2):637–641 discussion 641
Desai MM, Rao PP, Aron M, Pascal-Haber G, Desai MR, Mishra S, Kaouk JH, Gill IS (2008) Scarless single port transumbilical nephrectomy and pyeloplasty: first clinical report. BJU Int 101(1):83–88
Canes D, Desai MM, Aron M, Haber GP, Goel RK, Stein RJ, Kaouk JH, Gill IS (2008) Transumbilical single-port surgery: evolution and current status [see comment]. Eur Urol 54(5):1020–1029
Leroy J, Cahill RA, Asakuma M, Dallemagne B, Marescaux J (2009) Single-access laparoscopic sigmoidectomy as definitive surgical management of prior diverticulitis in a human patient. Arch Surg 144(2):173–179 discussion 179
Vander Velpen GC, Shimi SM, Cuschieri A (1993) Outcome after cholecystectomy for symptomatic gall stone disease and effect of surgical access: laparoscopic vs. open approach. Gut 34(10):1448–1451
Bass EB, Pitt HA, Lillemoe KD (1993) Cost-effectiveness of laparoscopic cholecystectomy versus open cholecystectomy. Am J Surg 165(4):466–471
Lam CM, Murray FE, Cuschieri A (1996) Increased cholecystectomy rate after the introduction of laparoscopic cholecystectomy in Scotland. Gut 38(2):282–284
Varadarajulu S, Tamhane A, Drelichman ER (2008) Patient perception of natural orifice transluminal endoscopic surgery as a technique for cholecystectomy. Gastrointest Endosc 67(6):854–860
Peterson CY, Ramamoorthy S, Andrews B, Horgan S, Talamini M, Chock A (2009) Women’s positive perception of transvaginal NOTES surgery. Surg Endosc 23(8):1770–1774
Swanstrom LL, Volckmann E, Hungness E, Soper NJ (2009) Patient attitudes and expectations regarding natural orifice translumenal endoscopic surgery. Surg Endosc 23(7):1519–1525
Disclosures
Drs. Ahsan Rao and James Kynaston, Mr. Euan Macdonald, and Mr. Irfan Ahmed have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1: Information sheet
Dear Participant:
Thank you for sparing time to answer four simple questions about your preference between different approaches available for appendicectomy.
There are various options available for removal of appendix.
-
1.
OPEN surgery (traditional old styled approach).
Using an incision/scar big enough to do surgery under direct vision.
-
2.
LAPAROSCOPIC surgery (key hole surgery—multiple incisions).
Multiple (3–4) small incisions usually 5–10 mm each to perform the operation.
-
3.
SINGLE PORT surgery (key hole surgery—single incision).
Virtually scarless, through a single hidden incision (12 mm) through the umbilicus.
-
4.
NOTES (Natural Orifice Transluminal Endoscopic Surgery)
Totally scarless, using natural openings of the body (e.g., mouth, vagina, rectum, etc.) to reach inside the abdomen to perform surgery.
The first two options are well established. Both options carry <1% risk of significant complications or death. Options 3 and 4 are new developments and safety profile is yet to be established.
Appendix 2: Questionnaire


Rights and permissions
About this article
Cite this article
Rao, A., Kynaston, J., MacDonald, E.R. et al. Patient preferences for surgical techniques: should we invest in new approaches?. Surg Endosc 24, 3016–3025 (2010). https://doi.org/10.1007/s00464-010-1078-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1078-y