Abstract
Background
Different surgical procedures impose different physical demands on surgeons and high prevalence rates of neck and shoulder pain have been reported among general surgeons. Past research has examined electromyography in surgeons mainly during simulated conditions of laparoscopic and open surgery but not during real-time operations and not for long durations. The present study compares the neck-shoulder muscle activities in three types of surgery and between different surgeons. The relationships of postural muscle activities to musculoskeletal symptoms and personal factors also are examined.
Methods
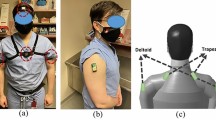
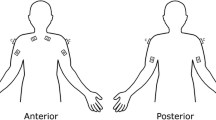
Twenty-five surgeons participated in the study (23 men). Surface electromyography (EMG) was recorded in the bilateral cervical erector spinae, upper trapezius, and anterior deltoid muscles during three types of surgical procedures: open, laparoscopic, and endovascular. In each procedure, EMG data were captured for 30 min to more than 1 h. The surgeons were asked to rate any musculoskeletal symptoms before and after surgery.
Results
The present study showed significantly higher muscle activities in the cervical erector spinae and upper trapezius muscles in open surgery compared with endovascular and laparoscopic procedures. Muscle activities were fairly similar between endovascular and laparoscopic surgery. The upper trapezius usually has an important role in stabilizing both the neck and upper limb posture, and this muscle also recorded higher activities in open compared with laparoscopic and endovascular surgeries. Surgeons reported similar degrees of musculoskeletal symptoms in open and laparoscopic surgeries, which were higher than endovascular surgery.
Conclusions
The present study showed that open surgery imposed significantly greater physical demands on the neck muscles compared with endovascular and laparoscopic surgeries. This may be due to the lighter manual task demands of these minimally invasive surgeries compared with open procedures, which generally required more dynamic movements and more forceful exertions.




Similar content being viewed by others
References
Wauben LSGL, van Veelen MA, Gossot D, Goossens RHM (2006) Application of ergonomic guidelines during minimally invasive surgery: a questionnaire survey of 284 surgeons. Surg Endosc 20:1268–1274
Liberman AS, Shrier I, Gordon PH (2005) Injuries sustained by colorectal surgeons performing colonoscopy. Surg Endosc 19:1606–1609
Szeto GPY, Ho P, Ting ACW, Poon JTC, Cheng SWK, Tsang RCC (2009) Work-related musculoskeletal symptoms in surgeons. J Occup Rehabil 19:175–184
van Det MJ, Meijerink WJHJ, Hoff C, Totte ER, Pierie JPEN (2009) Optimal ergonomics for laparoscopic surgery in minimally invasive surgery suites: a review and guidelines. Surg Endosc 23:1279–1285
Berguer R, Gerber S, Kilpatrick G, Beckley D (1998) An ergonomic comparison of in-line vs pistol-grip handle configuration in a laparoscopic grasper. Surg Endosc 12:805–808
Matern U, Kuttler G, Giebmeyer C, Waller P, Faist M (2004) Ergonomics aspects of five different types of laparoscopic instrument handles under dynamic conditions with respect to specific laparoscopic tasks: an electromyographic-based study. Surg Endosc 18:1231–1241
Berguer R, Rab GT, Abu-Ghaida H, Alarcon A, Chung JA (1997) A comparison of surgeons’ posture during laparoscopic and open surgical procedures. Surg Endosc 11:139–142
Matern U, Faist M, Kehl K, Giebmeyer C, Buess G (2005) Monitor position in laparoscopic surgery. Surg Endosc 19:436–440
Berguer R, Smith WD, Davis S (2002) An ergonomic study of the optimum operating table height for laparoscopic surgery. Surg Endosc 16:416–421
Manasnayakorn S, Cuschieri A, Hanna GB (2009) Ergonomic assessment of optimum operating table height for hand-assisted laparoscopic surgery. Surg Endosc 23:783–789
van Veelen MA, Kazemier G, Koopman J, Goossens RH, Meijer DW (2002) Assessment of the ergonomically optimal operating surface height for laparoscopic surgery. J Laparoendosc Adv Surg Tech 12:47–52
Albayrak A, van Veelen MA, Prins JF, Snijders CJ, de Ridder H, Kazemier G (2007) A newly designed ergonomic body support for surgeons. Surg Endosc 21:1835–1840
Nguyen NT, Ho HS, Smith WD, Phillips C, Lewis C, De Vera RM, Berguer R (2001) An ergonomic evaluation of surgeons’ axial and upper extremity movements during laparoscopic and open surgery. Am J Surg 182:720–724
Patil PV, Hanna GB, Frank TG, Cuschieri A (2005) Effect of fixation of shoulder and elbow joint movement on the precision of laparoscopic instrument manipulations. Surg Endosc 19:366–368
Uhrich ML, Underwood RA, Standeven JW, Soper NJ, Engsberg JR (2002) Assessment of fatigue, monitor placement, and surgical experience during simulated laparoscopic surgery. Surg Endosc 16:635–639
Szeto GPY, Straker LM, O’Sullivan PB (2005) A comparison of symptomatic and asymptomatic office workers performing monotonous keyboard work—1. Neck and shoulder muscle recruitment patterns. Man Ther 10:270–280
Hägg GM, Astrom A (1997) Load pattern and pressure pain threshold in the upper trapezius muscle and psychosocial factors in medical secretaries with and without shoulder/neck disorders. Int Arch Occup Environ Health 69:423–432
Madeleine P, Lundager B, Voigt M, Arendt-Nielsen L (1999) Shoulder muscle co-ordination during chronic and acute experimental neck-shoulder pain. Eur J Appl Physiol 79:127–140
Falla D, Bilenkij G, Jull G (2004) Patients with chronic neck pain demonstrate altered patterns of muscle activation during performance of a functional upper limb task. Spine 29:1436–1440
Cram JR, Kasman GS, Holtz J (1998) Introduction to surface electromyography, 1st edn. Aspen Publisher Incorporation, Gaithersburg, pp 15–20
Hermen HJ, Freriks B, Merletti R et al (1999) European recommendations for surface electromyography: results of the SENIAM project, 2nd edn. Roessingh Research and Development, The Netherlands, pp 101–110
Kuorinka I, Jonsson B, Kilbom Å, Vinterberg H, Biering-Sörenson F, Andersson A, Jorgensen K (1987) Standardised Nordic Questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon 18(3):233–237
Jonsson B (1982) Measurement and evaluation of local muscular strain in the shoulder during constrained work. J Hum Ergol 11:73–88
Berguer R, Forkey DL, Smoth WD (1999) Ergonomic problems associated with laparoscopic surgery. Surg Endosc 13:466–468
Quick NE, Gillete JC, Shapiro R, Adrales GL, Gerlach D, Park AE (2003) The effect of using laparoscopic instruments on muscle activation patterns during minimally invasive surgical training procedures. Surg Endosc 17:462–465
Sandsjo L, Melin B, Rissen D, Dohns L, Lundberg U (2000) Trapezius muscle activity, neck and shoulder pain, and subjective experiences during monotonous work in women. Eur J Appl Physiol 83:235–238
Westgaard RH, Vasseljen O, Holte KA (2001) Trapezius muscle activity as a risk indicator for shoulder and neck pain in female service workers with low biomechanical exposure. Ergonomics 44:339–353
Szeto GPY, Straker LM, O’Sullivan PB (2009) Examining the low, high and range measures of muscle activity amplitudes in symptomatic and asymptomatic computer users performing typing and mousing tasks. Eur J Appl Physiol 106:243–251
Madeleine P, Mathiassen SE, Arendt-Nielsen L (2008) Changes in the degree of motor variability associated with experimental and chronic neck-shoulder pain during a standardized repetitive arm movement. Exp Brain Res 185:689–698
Hansson GA, Stromberg U, Larsson B, Ohlsson K, Balogh I, Moritz U (1992) Electromyographic fatigue in neck/shoulder muscles and endurance in women with repetitive work. Ergonomics 35:1341–1352
Acknowledgments
The authors express their sincere appreciation to the Bupa Foundation for funding this research project, and thank all of the surgeons who participated in the study. The authors thank the research assistants, Silvana Lau, Y. Y. Wong, Winnie Leung, and Ted Wong; without their help, this project would not be run so smoothly. The authors acknowledge Mr. Raymond Chung from the Hong Kong Polytechnic University for providing expert advice on statistical analysis, and Mr. Man Cheung for the technical advice on EMG data collection and analysis.
Disclosures
The current project has been funded by Bupa Foundation Medical Research Grants. G. P. Y. Szeto, P. Ho, A. C. W. Ting, J. T. C. Poon, R. C. C. Tsang, and S. W. K. Cheng have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Szeto, G.P.Y., Ho, P., Ting, A.C.W. et al. A study of surgeons’ postural muscle activity during open, laparoscopic, and endovascular surgery. Surg Endosc 24, 1712–1721 (2010). https://doi.org/10.1007/s00464-009-0834-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-009-0834-3