Abstract
Background
Intraoperative endoscopy (IOE) is a useful adjunct during laparoscopic gastrointestinal (GI) surgery. However, one potential hazard of IOE is a prolonged bowel distension due to insufflated air, which may cause obstructed surgical exposure and increased postoperative abdominal pain. Recently, carbon dioxide (CO2), with its rapid absorptive nature, has been proven effective to minimize prolonged bowel distension in ambulatory/intraoperative colonoscopy. The objectives were to assess the feasibility, safety, and efficacy of CO2-insufflating upper GI IOE during laparoscopic surgery.
Methods
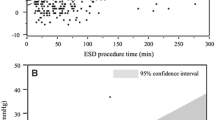
A historical comparison study was performed on the initial ten consecutive patients who underwent CO2-insufflating upper GI IOE (CO2-IOE) during laparoscopic surgery. The control group consisted of the past 12 consecutive patients who underwent conventional air-insufflating upper GI IOE (air-IOE) during laparoscopic surgery. The following parameters were compared between the two groups: (1) patient demographics; (2) feasibility (% completion of IOE); (3) safety (complications related to IOE, impacts on cardiopulmonary status, including systemic blood pressure, heart rate, and end-tidal CO2); (4) efficacy (postoperative residual intestinal gas, time to resume oral intake, and bowel movement). The amounts of post-IOE residual intestinal gas were evaluated and classified on the immediate postoperative abdominal radiographs in a blinded manner.
Results
Patient demographics were comparable between the two groups. IOE was completed in both groups without complications. Adverse effects on cardiopulmonary status were not observed during simultaneous intraperitoneal and intraluminal CO2 insufflation. In the air-IOE group, one patient was converted to open surgery because of inadequate surgical exposure from prolonged distension of the downstream bowel. The patients in the CO2-IOE group had significantly lower grade of postoperative bowel distension than the control group. Postoperative oral intake was resumed earlier in the CO2-IOE group.
Conclusion
CO2-insufflating upper GI IOE during laparoscopic surgery is feasible, safe, and has a practical advantage in minimizing post-IOE bowel distension compared with conventional air-insufflating upper GI IOE.


Similar content being viewed by others
References
Kim SH, Milsom JW, Church JM, Ludwig KA, Garcia-Ruiz A, Okuda J, Fazio VW (1997) Perioperative tumor localization for laparoscopic colorectal surgery. Surg Endosc 11:1013–1016
Brandt LJ, Boley SJ, Sammartano R (1986) Carbon dioxide and room air insufflation of the colon: effects on colonic blood flow and intraluminal pressure in the dog. Gastrointest Endosc 32:324–329
Silva A, Ho HS, Mathiesen KA, Wolfe BM (1997) Gastrointestinal endoscopy combined with laparoscopy or laparotomy. Surg Endosc 11:214
Saltzman HA, Sieker HO (1968) Intestinal response to changing gaseous environments: normobaric and hyperbaric observations. Ann NY Acad Sci 150:31–39
Bretthauer M, Thiis-Evenson E, Huppertz-Hauss G, Gisselsson L, Grotmol T, Skovlund E, Hoff G (2002) NORCCAP (Norwegian colorectal cancer prevention): a randomized trial to assess the safety and efficacy of carbon dioxide versus air insufflation in colonoscopy. Gut 50:604–607
Church J, Delaney C (2003) Randomized, controlled trial of carbon dioxide insufflation during colonoscopy. Dis Colon Rectum 46:322–326
Hussein AM, Bartram CI, Williams CB (1984) Carbon dioxide insufflation for more comfortable colonoscopy. Gastrointest Endosc 30:68–70
Phaosawasdi K, Cooley W, Wheeler J, Rice P (1986) Carbon dioxide-insufflated colonoscopy: an ignored superior technique. Gastrointest Endosc 32:330–333
Stevenson GW, Wilson JA, Wilkinson J, Norman G, Goodacre RL (1992) Pain following colonoscopy: elimination with carbon dioxide. Gastrointest Endosc 38:564–567
Sumanac K, Zealley I, Fox BM, Rawlinson J, Salena B, Marshall JK, Stevenson GW, Hunt RH (2002) Minimizing postcolonoscopy abdominal pain by using CO2 insufflation: a prospective, randomized, double-blind, controlled trial evaluating a new commercially available CO2 delivery system. Gastrointest Endosc 56:190–194
Williams CB (1986) Who’s for CO2? Gastrointest Endosc 32:365–367
Yasumasa K, Nakajima K, Endo S, Ito T, Matsuda H, Nishida T (2006) Carbon dioxide insufflation attenuates parietal blood flow obstruction in distended colon. Surg Endosc 20:587–594
Nakajima K, Lee SW, Sonoda T, Milson JW (2005) Intraoperative carbon dioxide colonoscopy: a safe insufflation alternative for locating colonic lesions during laparoscopic surgery. Surg Endosc 19:321–325
Nomura S, Kaminishi M (2007) Surgical treatment of early gastric cancer. Dig Surg 24:96–100
Cappell MS, Friedel D (2002) The role of sigmoidoscopy and colonoscopy in the diagnosis and management of lower gastrointestinal disorders: endoscopic findings, therapy, and complications. Med Clin North Am 86:1253–1288
Huang EH, Marks JM (2001) The diagnosis and therapeutic roles of colonoscopy: a review. Surg Endosc 15:1373–1380
Waye JD (1992) Colonoscopy. CA Cancer J Clin 42:350–365
Katzgraber F, Glenewinkel F, Fischler S, Rittner C (1998) Mechanism of fatal air embolism after gastrointestinal endoscopy. Int J Legal Med 111:154–156
Rogers BH (1974) The safety of carbon dioxide insufflation during colonoscopic electrosurgical polypectomy. Gastrointest Endosc 20:115–117
Rattner D, Kalloo A (2006) ASGE/SAGES working group on natural orifice translumenal endoscopic surgery. Surg Endosc 20:329–333
Hochberger J, Lamadé W (2005) Transgastric surgery in the abdomen: the dawn of a new era? Gastrointest Endosc 62:293–296
Kantsevoy SV, Hu B, Jagannath SB, Vaughn CA, Beitler DM, Chung SS, Cotton PB, Gostout CJ, Hawes RH, Paricha PJ, Magee CA, Pipitone LJ, Talamini MA, Kalloo AN (2006) Transgastric endoscopic splenectomy: is it possible? Surg Endosc 20:522–525
Acknowledgments
Part of this study was presented at the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) at Pennsylvania Convention Center, Philadelphia, Pennsylvania, April 2008. The authors thank Kenji Noda and Masakazu Gotanda (Olympus Medical Systems, Tokyo, Japan) for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Souma, Y., Nakajima, K., Takahashi, T. et al. The role of intraoperative carbon dioxide insufflating upper gastrointestinal endoscopy during laparoscopic surgery. Surg Endosc 23, 2279–2285 (2009). https://doi.org/10.1007/s00464-008-0309-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-0309-y