Abstract
Background
Laparoscopic Heller myotomy has been proven effective. Reliable predictive factors for outcome and the true benefit of the da Vinci robotic system, however, remain unknown.
Methods
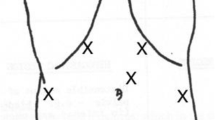
Seventy patients underwent laparoscopic Heller myotomy. The number of intraoperative perforations and the symptom-predictive value of postoperative esophagogram width measurement at the gastroesophageal junction were analyzed.
Results
The overall complication rate was 11%. Four patients experienced intraoperative perforation during the laparoscopic technique. No perforations were experienced with the da Vinci robotic system (n = 19). Of the total, 82% of patients had resolution of dysphagia, 91% of regurgitation, 91% of heartburn and 82% of chest pain. Immediate postoperative esophagogram gastroesophageal junction width demonstrated a positive predictive trend from 0 to 10 mm for dysphagia.
Conclusion
Laparoscopic Heller myotomy is an effective treatment for achalasia. Immediate postoperative esophagogram gastroesophageal junction width measurement as a predictor for symptom resolution requires further study.



Similar content being viewed by others
References
Arain MA, Peters JH, Tamhankar AP, Portale G, Almogy G, DeMeester SR, Crookes PF, Hagen JA, Bremner CG, DeMeester TR (2004) Preoperative lower esophageal sphincter pressure affects outcome of laparoscopic esophageal myotomy for achalasia. J Gastrointest Surg 8(3): 328–334
Beckingham IJ, Callanan M, Louw JA, Bornman PC (1999) Laparoscopic cardiomyotomy for achalasia after failed balloon dilatation. Surg Endosc 13(5): 493–496
Bloomston M, Serafini F, Rosemurgy AS (2001) Videoscopic heller myotomy as first-line therapy for severe achalasia. Am Surg 67(11): 1105–1109
Howard PJ, Maher L, Pryde A, Cameron EW, Heading RC (1992) Five-year prospective study of the incidence, clinical features and diagnosis of achalasia in Edinburgh. Gut 33: 1011–1015
Morino M, Rebecchi F, Festa V, Garrone C (1997) Preoperative pneumatic dilatation represents a risk factor for laparoscopic Heller myotomy. Surg Endosc 11: 359–361
Patti MG, Feo CV, Arcerito M, De Pinto M, Tamburini A, Diener U, Gantert W, Way LW (1999) Effects of previous treatment on results of laparoscopic Heller myotomy for achalasia. Dig Dis Sci 44(11): 2270–2276
Patti MG, Pellegrini CA, Horgan S, Arcerito M, Omelanczuk P, Tamburini A, Diener U, Eubanks TR, Way LW (1999) Minimally invasive surgery for achalasia: an 8-year experience with 168 patients. Ann Surg 230(4): 587–594
Payne WS (1989) Heller’s contribution to the surgical treatment of achalasia of the esophagus. Ann Thorac Surg 48: 876–881
Pechlivanides G, Chrysos E, Athanasakis E, Tsiaoussis J, Vassilakis JS, Xynos E (2001) Laparoscopic Heller cardiomyotomy and Dor fundoplication for esophageal achalasia: possible factors predicting outcome. Arch Surg 136(11): 1240–1243
Pellegrini CA, Leichter R, Patti M, Somberg K, Ostroff JW, Way L (1993) Thoracoscopic esophageal myotomy in the treatment if achalasia. Ann Thoracic Surg 56: 680–682
Richter JE (1989) Surgery or pneumatic dilatation for achalasia a head to head comparison. Now are all the questions answered? Gastroenterology 97: 1340–1341
Richter JE (2004) Achalasia. In: Castell DO, Richter JE (eds). The esophagus. Lipponcott Williams & Wilkins, Philadelphia, PA, pp 221–261
Stewart KC, Finley RJ, Clifton JC, Graham AJ, Storseth C, Inculet R (1999) Thoracoscopic versus laparoscopic modified Heller myotomy for achalasia: efficacy and safety in 87 patients. J Am Coll Surg 189: 164–169; discussion 169–170
Vogt D, Curet M, Pitcher D, Josloff R, Milne RL, Zucker K (1997) Successful treatment of esophageal achalasia with laparoscopic Heller myotomy and Toupet fundoplication. Am J Surg 174(6): 709–714
Wills VL, Hunt DR (2001) Functional outcome after Heller myotomy and fundoplication for achalasia. J Gastrointest Surg 5(4): 408–413
Yaghoobi M, Mikaeli J, Montazeri G, Nouri N, Sohrabi MR, Malekzadeh R (2003) Correlation between clinical severity score and the lower esophageal sphincter relaxation pressure in idiopathic achalasia. Am J Gastroenterol 98(2): 278–283
Yoo C, Levine MS, Redfern RO, Laufer I, Buyske J (2004) Laparoscopic Heller myotomy and fundoplication: findings and predictive value of early postoperative radiographic studies. Abdom Imaging 29(6): 643–647
Zaijer JH (1923) Cardiospasm in the aged. Ann Surg 77: 615–617
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iqbal, A., Haider, M., Desai, K. et al. Technique and follow-up of minimally invasive Heller myotomy for achalasia. Surg Endosc 20, 394–401 (2006). https://doi.org/10.1007/s00464-005-0069-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-005-0069-x