Abstract
Background
The aim of this prospective study was to compare the outcome of laparoscopic colorectal surgery in obese and nonobese patients.
Methods
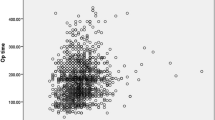
All patients who underwent laparoscopic surgery for both benign and malignant disease within the past 5 years were entered into the prospective database registry. Body mass index (BMI; kg/m2) was used as the objective measure to indicate morbid obesity. Patients with a BMI >30 were defined as obese, and patients with a BMI <30 were defined as nonobese. The parameters analyzed included age, gender, comorbid conditions, diagnosis, procedure, duration of surgery, transfusion requirements, conversion rate, overall morbidity rate including major complications (requiring reoperation), minor complications (conservative treatment) and late-onset complications (postdischarge), stay on intensive case unit, hospitalization, and mortality. For objective evaluation, only laparoscopically completed procedures were analyzed. Statistics included Student’s t test and chi-square analysis. Statistical significance was assessed at the 5% level (p < 0. 05 statistically significant).
Results
A total of 589 patients were evaluated, including 95 patients in the obese group and 494 patients in the nonobese group. There was no significant difference in conversion rate (7.3% in the obese group vs 9.5% in the nonobese group, p > 0.05) so that the laparoscopic completion rate was 90.5% (n = 86) in the obese and 92.7% (n = 458) in the nonobese group. The rate of females was significantly lower among obese patients (55.8% in the obese group vs 74.2% in the nonobese group, p = 0.001). No significant differences were observed with respect to age, diagnosis, procedure, duration of surgery, and transfusion requirements (p > 0.05). In terms of morbidity, there were no significant differences related to overall complication rates with respect to BMI (23.3% in the obese group vs 24.5% in the nonobese group, p > 0.05). Major complications were more common in the obese group without showing statistical significance (12.8% in the obese group vs 6.6% in the nonobese group, p = 0.078). Conversely, minor complications were more frequently documented in the nonobese group (8.1% in the obese group vs 15.5% in the nonobese group, p = 0.080). In the postoperative course, no differences were documented in terms of return of bowel function, duration of analgesics required, oral feeding, and length of hospitalization (p > 0.05).
Conclusion
These data indicate that laparoscopic colorectal surgery is feasible and effective in both obese and nonobese patients. Obese patients who are thought to be at increased risk of postoperative morbidity have the similar benefit of laparoscopic surgery as nonobese patients with colorectal disease.
Similar content being viewed by others
References
S Benoist Y Panis A Alves P Valleur (2000) ArticleTitleImpact of obesity on surgical outcomes after colorectal resection Am J Surg 179 275–281 Occurrence Handle10.1016/S0002-9610(00)00337-8 Occurrence Handle1:STN:280:DC%2BD3czjs1eqtA%3D%3D Occurrence Handle10875985
HP Bruch A Herold T Schiedeck O Schwandner (1999) ArticleTitleLaparoscopic surgery for rectal prolapse and outlet obstruction Dis Colon Rectum 42 1189–1194 Occurrence Handle1:STN:280:DyaK1MvisVykuw%3D%3D Occurrence Handle10496560
HP Bruch THK Schiedeck O Schwandner (1999) ArticleTitleLaparoscopic colorectal surgery: a five-year experience Dig Surg 16 45–54 Occurrence Handle10.1159/000018693 Occurrence Handle1:STN:280:DyaK1M7js1Wnsg%3D%3D Occurrence Handle9949267
PS Choban L Flancbaum (1997) ArticleTitleImpact of obesity on surgical outcomes: a review J Am Coll Surg 185 593–603 Occurrence Handle10.1016/S1072-7515(97)00109-9 Occurrence Handle1:STN:280:DyaK1c%2Fmsleqsg%3D%3D Occurrence Handle9404886
D Dindo MK Mueller M Weber PA Clavien (2003) ArticleTitleObesity in general elective surgery Lancet 361 2032–2035 Occurrence Handle10.1016/S0140-6736(03)13640-9 Occurrence Handle12814714
J Doublet G Belair (2000) ArticleTitleRetroperitoneal laparoscopic nephrectomy is safe and effective in obese patients: a comparative study of 55 procedures Urology 56 63–66 Occurrence Handle10.1016/S0090-4295(00)00533-1 Occurrence Handle1:STN:280:DC%2BD3czovFyhtg%3D%3D Occurrence Handle10869625
GH Eltabbakh MS Piver RE Hempling FO Recio (1999) ArticleTitleLaparoscopic surgery in obese women Obstet Gynecol 94 704–708 Occurrence Handle10.1016/S0029-7844(99)00406-8 Occurrence Handle1:STN:280:DC%2BD3c%2Fht1ajtw%3D%3D Occurrence Handle10546714
N Gatsoulis S Koulas G Kiparos N Tzafestas K Pangratis K Pandis G Mavrakis (1999) ArticleTitleLaparoscopic cholecystectomy in obese and nonobese patients Obes Surg 9 459–461 Occurrence Handle10.1381/096089299765552756 Occurrence Handle1:STN:280:DC%2BD3c%2FntF2hsg%3D%3D Occurrence Handle10605904
P Gervaz A Pikarsky M Utech M Secic J Efron B Belin A Jain SD Wexner (2001) ArticleTitleConverted laparoscopic colorectal surgery Surg Endosc 15 827–832 Occurrence Handle10.1007/s004640080062 Occurrence Handle1:STN:280:DC%2BD3MrksFSitg%3D%3D Occurrence Handle11443444
Z Holub A Jabor L Kliment D Fischlova M Wagnerova (2001) ArticleTitleLaparoscopic hysterectomy in obese women: a clinical prospective study Eur J Obstet Gynecol Repord Biol 98 77–78 Occurrence Handle10.1016/S0301-2115(00)00565-0 Occurrence Handle1:STN:280:DC%2BD3MvntF2jtg%3D%3D
F Marusch I Gastinger C Schneider H Scheidbach J Konradt HP Bruch L Koehler E Baerlehner InstitutionalAuthorNameKoeckerling F—Laparoscopic Colorectal Surgery Study Group (2001) ArticleTitleImportance of conversion for results obtained with laparoscopic colorectal surgery Dis Colon Rectum 44 207–214 Occurrence Handle1:STN:280:DC%2BD3M7ot1Sluw%3D%3D Occurrence Handle11227937
AJ Pikarsky Y Saida T Yamaguchi S Martinez W Chen EG Weiss JJ Nogueras SD Wexner (2002) ArticleTitleIs obesity a high-risk factor for laparoscopic colorectal surgery? Surg Endosc 16 855–858 Occurrence Handle10.1007/s004640080069 Occurrence Handle1:STN:280:DC%2BD383lvVagsA%3D%3D Occurrence Handle11997837
TH Schiedeck O Schwandner HP Bruch (1998) ArticleTitleLaparoscopic sigmoid resection in diverticulitis [in German] Chirurg 69 846–853 Occurrence Handle10.1007/s001040050499 Occurrence Handle1:STN:280:DyaK1cvlsFOhsw%3D%3D Occurrence Handle9782401
THK Schiedeck O Schwandner HP Bruch (1999) ArticleTitleLaparoscopic therapy of chronic constipation [In German] Zentralbl Chir 124 818–824 Occurrence Handle1:STN:280:DC%2BD3c%2FhtFOhsQ%3D%3D Occurrence Handle10544488
O Schwandner THK Schiedeck HP Bruch (1999) ArticleTitleThe role of conversion in laparoscopic colorectal surgery: do predictive factors exist? Surg Endosc 13 151–156 Occurrence Handle10.1007/s004649900927 Occurrence Handle1:STN:280:DyaK1M7hslCrsQ%3D%3D Occurrence Handle9918619
O Schwandner THK Schiedeck C Killaitis HP Bruch (1999) ArticleTitleA case-control study comparing laparoscopic versus open surgery for rectosigmoidal and rectal cancer Int J Colorectal Dis 14 158–163
AJ Senagore CP Delaney K Madboulay KM Brady CV Fazio (2003) ArticleTitleLaparoscopic colectomy in obese and nonobese patients J Gastrointest Surg 7 558–561 Occurrence Handle10.1016/S1091-255X(02)00124-5 Occurrence Handle12763416
P Sperlongano D Pisaniello D Parmeggiani M Falco ParticleDe M Agresti U Parmeggiani (2002) ArticleTitleLaparoscopic cholecystectomy in the morbidly obese [in Italian] Chir Ital 54 363–366 Occurrence Handle12192933
JJ Tuech N Regenet S Hennekinne P Pessaux R Bergamaschi JP Arnaud (2001) ArticleTitleLaparoscopic colectomy for sigmoid diverticulitis in obese and nonobese patients: a prospective comparative study Surg Endosc 15 1427–1430 Occurrence Handle1:STN:280:DC%2BD383ivVSktw%3D%3D Occurrence Handle11965459
H Zeller H Hauner (1999) ArticleTitleObesity—what is the significance for the organism? [in German] Minimal Invasive Chirurgie 8 170–176
Acknowledgments
Preparation of the manuscript was performed during a clinical observership by O. Schwandner the author at the Department of Surgery at Cleveland Clinic Florida supported by a grant from the Stiftung Coloplast, Hamburg, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schwandner, O., Farke, S., Schiedeck, T.H.K. et al. Laparoscopic colorectal surgery in obese and nonobese patients: Do differences in body mass indices lead to different outcomes?. Surg Endosc 18, 1452–1456 (2004). https://doi.org/10.1007/s00464-003-9259-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-003-9259-6