Abstract
Background
Fundus-first dissection (FFD) is an established technique to deal with difficult open cholecystectomies. Although the indications for such an approach are similar for laparoscopic cholecystectomy (LC), FFD is not widely practiced because of difficulties that arise with liver retraction, the dissection of dense adhesions, or obscured cystic pedicles, often necessitating conversion to an open procedure.
Methods
The aim of this study was to evaluate the indications for FFD and the technical aspects of the procedure in cases with a difficult cystic pedicle. Prospectively collected data and video recordings of cases of fundus-first laparoscopic cholecystectomy (FFLC) were analyzed. The great majority were difficult cases, so we also reviewed the safety aspects of this approach and assessed its effect on the conversion rate.
Results
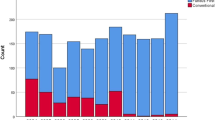
FFLC was resorted to in 35 cases (5%) of 710 consecutive LCs with difficulty grade II (two cases), III (13 cases), or IV (20 cases). There were 16 male patients (46% vs 9% males in the whole), and the mean age was 56 years (ranges, 28–87). The reasons for FFD were dense adhesions preventing the exposure of the cystic pedicle in 14 cases, large Hartmann’s pouch stones in 10 cases, short dilated cystic ducts in six cases, and Mirizzi syndrome in three cases. Two cases had contracted “burnout” gallbladders. Intraoperative cholangiography (IOC) was possible in 24 patients, failed in 10 (29%), and was not attempted in one. Seven patients had bile duct stones and required bile duct exploration. FFLC was completed in 31 patients, 28 of whom were seriously considered for conversion prior to commencing FFD. Conversion was still necessary after trial FFD in four cases (11%) two with Mirizzi abnormalities, one with bile duct stones, and one with dense adhesions. The mean operative time was 125 min, (range, 50–230). There were no operative or technique-related complications.
Conclusion
FFLC is feasible and is a safe option for cases with a difficult cystic pedicle. Its use reduced the conversion rate of the series from a potential 5.2% to 1.2%, However, subtotal cholecystectomy or conversion must not be delayed if, after the neck of the gallbladder is reached the anatomy is still unclear.
Similar content being viewed by others
References
Araujo-Teixeira JP, Rocha-Reis J, Costa-Cabral A, Barros H, Saraiva AC, Araujo-Teixeira AM (1999) Laparoscopy or laparotomy in acute cholecystitis (200 cases): comparison of the results and factors predictive of conversion. Chirurgie 124: 529–535
Bickel A, Rappaport A, Hazani E, Eitan A (1998) Laparoscopic cholecystectomy for acute cholecystitis performed by residents in surgery: a risk factor for conversion to open laparotomy? J Laparoendosc Adv Surg Tech A 8: 137–141
Bickel A, Rappaport A, Kanievski V, Vaksman I, Haj M, Geron N, Eitan A (1996) Laparoscopic management of acute cholecystitis, prognostic factors for success. Surg Endosc 10: 1045–1049
Fried GM, Barkun JS, Sigman HH, Joseph L, Clas D, Garzon J, Hincher EJ, Meakin S (1994) Factors determining conversion to laparotomy in patients undergoing laparoscopic cholecystectomy. Am J Surg 167: 35–39
Hauer-Jensen M, Karesen R, Nygaard K, Solheim K, Amlie E, Havig O, Viddal KO (1985) Predictive ability of choledocholithiasis indicators—a prospective evaluation. Ann Surg 202: 64–68
Hermann RE (1976) A plea for a safe technique of cholecystectomy. Surgery 79: 609–611
Koperna T, Kisser M, Schulz F (1999) Laparoscopic versus open treatment of patients with acute cholecystitis. Hepatogastroenterology 46: 753–757
Lo CM, Fan ST, Liu CL, Lai EC, Wong J (1997) Early decision for conversion of laparoscopic to open cholecystectomy for treatment of acute cholecystitis. Am J Surg 173: 513–517
Mahmud S, Hamza Y, Nassar AHM (2001) The significance of cystic duct stones encountered during laparoscopic cholecystectomy. Surg Endosc 15: 460–462
Martin IG, Dexter SP, Marton J, Gibson J, Asker J, Firullo A, McMahan MJ (1995) Fundus-first laparoscopic cholecystectomy. Surg Endosc 9: 203–206
Mattioli FP, Cagnazzo A, Razzetta F, Biaanchi C, Varaldo E, Campagna A, Percivale A (1999) Laparoscopic cholecystectomy: an analysis of reasons for a conversion to conventional surgery in an elective surgery department. Minerva Chir 54: 471–476
Moossa AR, Mayer AD, Stabile B (1990) Iatrogenic injury to the bile duct. Arch Surg 119: 92–107
Nassar AHM, Ashkar KA, Mohamed AY, Hafiz AA (1995) Is laparoscopic cholecystectomy possible without video technology? Min Invas Ther 4: 63–65
Parra Blanco JA, Bueno Lopez J, Madrazo Leal C, Farinas Alvarez C, Torre Carrasco F, Farinas MC (1999) Laparoscopic cholecystectomy: analysis of risk factors for predicting conversion to open cholecystectomy. Rev Esp Enferm Dig 91: 359–364
Sanabria JR, Gallinger S, Croxford R, Strasberg SM (1994) Risk factors in elective laparoscopic cholecystectomy for conversion to open cholecystectomy. J Am Coll Surg 176: 696–704
Tamij Marane A, Campbell DF, Nassar AHM (2000) Intracorporeal ligation of the cystic duct and artery during laparoscopic cholecystectomy: do we need the endoclips? Min Invas Ther All Technol 9: 13–14
Uyama I, Lida S, Ogiwara H, Takahara T, Kato Y, Furuta T, Kikuchi K (1995) Laparoscopic retrograde cholecystectomy (from fundus downwards) facilitated by lifting the liver bed up to the diaphragm for inflammatory gallbladder. Surg Laparosc Endosc 5: 431–436
Wongworawat MD, Aitken DR, Robles AE, Garberoglio C (1994) The impact of prior intra-abdominal surgery on laparoscopic cholecystectomy. Am Surg 60: 763–766
Yu CS, Chen SC, Wang SM, Wei TC (1994) Is previous abdominal surgery a contraindication to laparoscopic cholecystectomy? J Laparoendosc Surg 4: 31–35
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Mahmud, S., Masaud, M., Canna, K. et al. Fundus-first laparoscopic cholecystectomy. Surg Endosc 16, 581–584 (2002). https://doi.org/10.1007/s00464-001-9094-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-001-9094-6