Abstract
Quantitative analysis of modified barium swallow (MBS) imaging is useful to determine the impact of various disease states on pharyngeal swallowing mechanics. In this retrospective proof of concept study, kinematic analysis and computational analysis of swallowing mechanics (CASM) were used to demonstrate how these methods differentiate swallowing dysfunction by dysphagia etiology. Ten subjects were randomly selected from four cohorts of dysphagic patients including COPD, head and neck cancer (HNC), motor neuron disease, and stroke. Each subject was age- and gender-matched with healthy, non-dysphagic controls. MBS videos of 5 ml thin and 5 ml thick bolus trials from each subject were used. A MATLAB tracker tool was adapted and updated to collect and compile data for each video (n = 160). For kinematic measurements, a MANOVA was performed with post-hoc analyses to determine group differences. For CASM measurements, a morphometric canonical variate analysis with post hoc analysis was performed to determine group differences. Kinematic analyses indicated statistically significant differences between HNC cohort and controls in distance measurements for hyolaryngeal approximation (p = .001), laryngeal elevation (p = 0.0001), pharyngeal shortening (p = 0.0002), and stage transition duration timing (p = 0.002). Timing differences were noted between the stroke cohort and controls for pharyngeal transit time (p = 0.007). Multivariate morphometric canonical variate analysis showed significant differences between etiology groups (p < 0.0001) with eigenvectors indicating differing patterns of swallowing mechanics. This study demonstrated that swallowing mechanics among cohorts of dysphagic patients can be differentiated using kinematics and CASM, providing different but complementary quantitative methods for investigating the impact of various disease states on swallowing function.





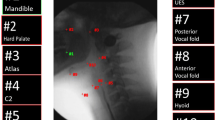
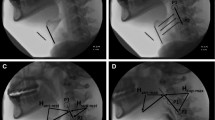
taken from a single video frame. Mathematical differences in geometric configuration, representing changes in swallowing mechanics, are calculated and plotted

Similar content being viewed by others
References
Seo HG, Oh B-M, Han TR. Swallowing kinematics and factors associated with laryngeal penetration and aspiration in stroke survivors with dysphagia. Dysphagia. 2016;31:160–8.
Starmer HM, Tippett D, Webster K, Quon H, Jones B, Hardy S, Gourin CG. Swallowing outcomes in patients with oropharyngeal cancer undergoing organ-preservation treatment. Head Neck. 2014;36:1392–7.
German RZ, Crompton A, Gould FD, Thexton AJ. Animal models for dysphagia studies: what have we learnt so far. Dysphagia. 2017;32:73–7.
Molfenter SM, Steele CM. Kinematic and temporal factors associated with penetration–aspiration in swallowing liquids. Dysphagia. 2014;29:269–76.
Kendall KA, McKenzie S, Leonard RJ, Gonçalves MI, Walker A. Timing of Events in Normal Swallowing: A Videofluoroscopic Study. Dysphagia. 2000;15:74–83.
Leonard RJ, Kendall KA, McKenzie S, Goncalves MI, Walker A. Structural displacements in normal swallowing: a videofluoroscopic study. Dysphagia. 2000;15:146–52.
Thompson TZ, Obeidin F, Davidoff AA, Hightower CL, Johnson CZ, Rice SL, Sokolove RL, Taylor BK, Tuck JM, Pearson WG Jr. Coordinate mapping of hyolaryngeal mechanics in swallowing. J Vis Exp. 2014;87:1–11.
Lee WH, Chun C, Seo HG, Lee SH, Oh B-M: STAMPS: development and verification of swallowing kinematic analysis software. Biomed Eng Online 16: no.120, 2017.
Kim Y, McCullough GH. Maximal hyoid excursion in poststroke patients. Dysphagia. 2010;25:20–5.
Pauloski BR, Logemann JA. Impact of tongue base and posterior pharyngeal wall biomechanics on pharyngeal clearance in irradiated postsurgical oral and oropharyngeal cancer patients. Head Neck. 2000;22:120–31.
Logemann JA, Pauloski BR, Rademaker AW, Colangelo LA, Kahrilas PJ, Smith CH. Temporal and Biomechanical Characteristics of Oropharyngeal Swallow in Younger and Older Men. J Speech Lang Hear Res. 2000;43:1264–74.
Steele CM, Bailey GL, Chau T, Molfenter SM, Oshalla M, Waito AA, Zoratto DCBH. The relationship between hyoid and laryngeal displacement and swallowing impairment. Clin Otolaryngol. 2011;36:30–6.
May NH, Pisegna JM, Marchina S, Langmore SE, Kumar S, Pearson WG Jr. Pharyngeal Swallowing Mechanics Secondary to Hemispheric Stroke. J Stroke Cerebrovasc Dis. 2017;26:952–61.
Garand KL, Schwertner R, Chen A, Pearson WG Jr. Computational Analysis of Pharyngeal Swallowing Mechanics in Patients with Motor Neuron Disease: A Pilot Investigation. Dysphagia. 2018;33:243–50.
Dietsch AM, Rowley CB, Solomon NP, Pearson WG Jr. Swallowing Mechanics Associated With Artificial Airways, Bolus Properties, and Penetration-Aspiration Status in Trauma Patients. J Speech Lang Hear Res. 2017;60:2442–511.
Pearson WG Jr, Davidoff AA, Smith ZM, Adams DE, Langmore SE. Impaired swallowing mechanics of post radiation therapy head and neck cancer patients: A retrospective videofluoroscopic study. World J Radiol. 2016;8:192–9.
Pearson WG, Zumwalt AC. Visualising Hyolaryngeal Mechanics in Swallowing Using Dynamic MRI. Comput Methods Biomech Biomed Eng Imaging Vis. 2014;2:208–16.
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756–63.
Rosenthal DI, Lewin JS, Eisbruch A. Prevention and treatment of dysphagia and aspiration after chemoradiation for head and neck cancer. J Clin Oncol. 2006;24:2636–43.
Heffernan C, Jenkinson C, Holmes T, Feder G, Kupfer R, Leigh PN, McGowan S, Rio A, Sidhu P. Nutritional management in MND/ALS patients: an evidence based review. Amyotroph Lateral Scler Other Motor Neuron Disord. 2004;5:72–83.
Steidl E, Ribeiro CS, Gonçalves BF, Fernandes N, Antunes V, Mancopes R. Relationship between dysphagia and exacerbations in chronic obstructive pulmonary disease: a literature review. Int Arch Otorhinolaryngol. 2015;19:74–9.
Martin-Harris B, Brodsky MB, Michel Y, Castell DO, Schleicher M, Sandidge J, Maxwell R, Blair J. MBS measurement tool for swallow impairment–MBSImp: establishing a standard. Dysphagia. 2008;23:392–405.
Cichero JA, Lam P, Steele CM, Hanson B, Chen J, Dantas RO, Duivestein J, Kayashita J, Lecko C, Murray J, Pillay M. Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: the IDDSI framework. Dysphagia. 2017;32:293–314.
Popa Nita S, Murith M, Chisholm H, Engmann J. Matching the rheological properties of videofluoroscopic contrast agents and thickened liquid prescriptions. Dysphagia. 2013;28:245–52.
Natarajan R, Stavness I, Pearson W. Semi-automatic tracking of hyolaryngeal coordinates in videofluoroscopic swallowing studies. Comput Methods Biomech Biomed Eng Imaging Vis. 2015;5:379–89.
Pearson WG Jr, Molfenter SM, Smith ZM, Steele CM. Image-based measurement of post-swallow residue: the normalized residue ratio scale. Dysphagia. 2013;28:167–77.
Leonard R, Rees CJ, Belafsky P, Allen J. Fluoroscopic surrogate for pharyngeal strength: the pharyngeal constriction ratio (PCR). Dysphagia. 2011;26:13–7.
Molfenter SM, Steele CM. Use of an anatomical scalar to control for sex-based size differences in measures of hyoid excursion during swallowing. Journal of speech, language, and hearing research : J Speech Lang Hear Res. 2014;57:768–78.
Klingenberg CP. MorphoJ: an integrated software package for geometric morphometrics. Mol Ecol Resour. 2011;11:353–7.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
Tran TTA, Martin Harris B, Pearson WG. Improvements resulting from respiratory-swallow phase training visualized in patient-specific computational analysis of swallowing mechanics. Comput Methods Biomech Biomed Eng Imaging Vis. 2016;6:532–8.
Mundry R, Sommer C. Discriminant function analysis with nonindependent data: consequences and an alternative. Anim Behav. 2007;74:965–76.
Schwertner RW, Garand KL, Pearson WG Jr. A Novel Imaging Analysis Method for Capturing Pharyngeal Constriction During Swallowing. J Imaging Sci. 2016;1:1–6.
Acknowledgements
Medical Scholars Program at the Medical College of Georgia provided funding to medical student authors. The following data sets were funded in part by various grants as indicated: Stroke, National Institute On Deafness And Other Communication Disorders of the National Institutes of Health under Award Number R01DC012584 (Kumar); COPD, Entera Health, Inc. (EH5220) (PI: Paoletti); HNC, National Institute on Deafness and Other Communication Disorders of the National Institutes of Health under award number R21DC010480 (PI: Martin-Harris); Normals, Veterans Affairs RR&D under award number CDA-1 1IK1RX001628-01A1 (PI: Garand), the National Institute on Deafness and Other Communication Disorders of the National Institutes of Health under award number K24DC12801 (PI: Martin-Harris), and the South Carolina Clinical & Translational Research (SCTR) Institute, with an academic home at the Medical University of South Carolina, NIH/NCATS Grant number TL1 TR000061 (PI: Brady; Project PI: Garand), and the American Speech-Language-Hearing Foundation (PI: Garand). The content is solely the responsibility of the authors and does not necessarily represent the official views the funding agencies listed above.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tadavarthi, Y., Hosseini, P., Reyes, S.E. et al. Pilot Study of Quantitative Methods for Differentiating Pharyngeal Swallowing Mechanics by Dysphagia Etiology. Dysphagia 36, 231–241 (2021). https://doi.org/10.1007/s00455-020-10123-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-020-10123-0