Abstract
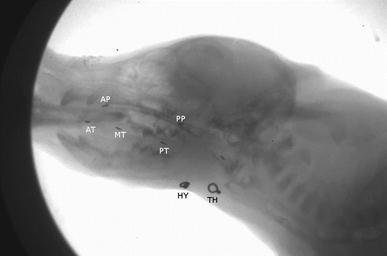
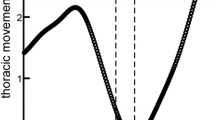
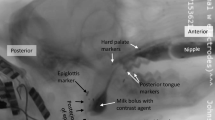
Aerodigestive coordination is critical for safe feeding in mammals, and failure to do so can result in aspiration. Using an infant pig model, we analyzed the impact of recurrent laryngeal nerve (RLN) lesion on aerodigestive coordination and swallow safety at two time points prior to weaning. We used high-speed videofluoroscopy to record 23 infant pigs longitudinally at two ages (7 days, 17 days) feeding on barium milk. We measured respiration with a plethysmograph and used the Infant Mammalian Penetration–Aspiration Scale (IMPAS) to identify unsafe swallows. We tested for changes in swallow safety longitudinally in control and lesion pigs, and whether there was any interaction between the four different groups. On postnatal day 7, lesioned pigs exhibited differences in the frequency distribution of IMPAS scores relative to control pigs on day 7, and 17 day old lesion and control pigs. There were longitudinal changes in performance following RLN lesion through time, suggesting that the impact of RLN lesion decreases with time, as older lesioned pigs performed similarly to older control pigs. We found minimal differences in the impact of aerodigestive coordination on swallow safety, with shorter delays of inspiration onset reflecting higher rates of penetration in young lesioned pigs. Healthy pigs aspirated at a similar rate to those with an RLN lesion indicating that the occasional occurrence of dysphagia in infants may be a normal behavior.


Similar content being viewed by others
References
Rofes L, Arreola V, Almirall J, Cabré M, Campins L, García-Peris P, et al. Diagnosis and management of oropharyngeal dysphagia and its nutritional and respiratory complications in the elderly. Gastroenterol Res Pract. 2011. https://doi.org/10.1155/2011/818979.
Holman SD, Campbell-Malone R, Ding P, Gierbolini-Norat EM, Griffioen AM, Inokuchi H, et al. Development, reliability, and validation of an infant mammalian penetration-aspiration scale. Dysphagia. 2013;28:178–87.
Jadcherla S. Dysphagia in the high-risk infant: potential factors and mechanisms. Am J Clin Nutr. 2016;103:622S–8S.
Gewolb IH, Vice FL. Maturational changes in the rhythms, patterning, and coordination of respiration and swallow during feeding in preterm and term infants. Dev Med Child Neurol. 2006;48:589–94.
Ballester A, Gould FDH, Bond L, Stricklen B, Ohlemacher J, Gross A, et al. Maturation of the coordination between respiration and deglutition with and without recurrent laryngeal nerve lesion in an animal model. Dysphagia. 2018;33:627–35. https://doi.org/10.1007/s00455-018-9881-z.
Horton KK, Segers LS, Nuding SC, O’Connor R, Alencar PA, Davenport PW, et al. Central respiration and mechanical ventilation in the gating of swallow with breathing. Front Physiol. 2018;9:1–17.
Martin-Harris B, McFarland D, Hill EG, Strange CB, Focht KL, Wan Z, Blair J, McGrattan K. Respiratory-swallow training in patients with head and neck cancer. Arch Phys Med Rehabilit. 2015;96:885–93.
Goldfield EC, Wolff PH, Schmidt RC. Dynamics of oralrespiratory coordination in full-term and preterm infants: 1. Comparisons at 38–40 weeks postconceptional age. Dev Sci. 1999;2:363–73.
Lau C, Smith EO, Schanler RJ. Coordination of suck-swallow and swallow respiration in preterm infants. Acta Paediatr. 2003;92:721–7.
Henderson M, Miles A, Holgate V, Peryman S, Allen J. Application and verification of quantitative objective videofluoroscopic swallowing measures in a pediatric population with dysphagia. J Pediatr. 2016;178:200–5. https://doi.org/10.1016/j.jpeds.2016.07.050.
Sachdeva R, Hussain E, Moss MM, Schmitz ML, Ray RM, Imamura M, et al. Vocal cord dysfunction and feeding difficulties after pediatric cardiovascular surgery. J Pediatr. 2007;151:312–5–315.e1-2.
Pourmoghadam KK, DeCampli WM, Ruzmetov M, Kosko J, Kishawi S, O’Brien M, et al. Recurrent laryngeal nerve injury and swallowing dysfunction in neonatal aortic arch repair. Ann Thorac Surg. 2017;104:1611–8.
Knight MJ, McDonald SE, Birchall MA. Intrinsic muscles and distribution of the recurrent laryngeal nerve in the pig larynx. Eur Arch Otorhinolaryngol. 2005;262:281–5.
Tessema B, Roark RM, Pitman MJ, Weissbrod P, Sharma S, Schaefer SD. Observations of recurrent laryngeal nerve injury and recovery using a rat model. Laryngoscope. 2009;119:1644–51.
Paniello RC, Rich JT, Debnath NL. Laryngeal adductor function in experimental models of recurrent laryngeal nerve injury. Laryngoscope. 2015;125:E67–72.
Bautista TG, Xing T, Fong AY, Pilowsky PM. Recurrent laryngeal nerve activity exhibits a 5-HT-mediated long-term facilitation and enhanced response to hypoxia following acute intermittent hypoxia in rat. J Appl Physiol. 2012;112:1144–56.
Gould FDH, Lammers AR, Ohlemacher J, Ballester A, Fraley L, Gross A, et al. The physiologic impact of unilateral recurrent laryngeal nerve (RLN) lesion on infant oropharyngeal and esophageal performance. Dysphagia. 2015;30:714–22.
Gould FDH, Ohlemacher J, Lammers AR, Gross A, Ballester A, Fraley L, et al. Central nervous system integration of sensorimotor signals in oral and pharyngeal structures: oropharyngeal kinematics response to recurrent laryngeal nerve lesion. J Appl Physiol. 2016;120:495–502.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
DeLozier KR, Gould FDH, Ohlemacher J, Thexton AJ, German RZ. The impact of recurrent laryngeal nerve lesion on oropharyngeal muscle activity and sensorimotor integration in an infant pig model. J Appl Physiol. 2018;125:159–66.
Gould FDH, Yglesias B, Ohlemacher J, German RZ. Pre-pharyngeal swallow effects of recurrent laryngeal nerve lesion on bolus shape and airway protection in an infant pig model. Dysphagia. 2017;32:362–73.
German RZ, Crompton AW, Gould FDH, Thexton AJ. Animal models for dysphagia studies: what have we learnt so far. Dysphagia. 2017;32:73–7.
Cichero JAY, Lam P, Steele CM, Hanson B, Chen J, Dantas RO, et al. Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: the IDDSI framework. Dysphagia. 2017;32:293–314.
Ismail FY, Fatemi A, Johnston MV. Cerebral plasticity: windows of opportunity in the developing brain. Eur J Paediatr Neurol. 2017;21:23–48.
Gao W, Lin W, Grewen K, Gilmore JH. Functional connectivity of the infant human brain: plastic and modifiable. Neuroscience 2017;23:169–84.
Mayerl CJ, Gould FDH, Bond LE, Stricklen BM, Buddington RK, German RZ. Preterm birth disrupts the development of feeding and breathing coordination. J Appl Phys. 2019;126:1681–6.
Campbell-Malone R, Crompton AW, Thexton AJ, German RZ. Ontogenetic changes in mammalian feeding: insights from electromyographic data. Int Comp Biol. 2011;51:282–8.
Acknowledgements
We would like to thank Ashley Ballester and the CMU at NEOMED for their extensive support of this project, as well as two anonymous reviewers of the manuscript.
Funding
This project was funded by NIH R01 HD088561 to R.Z.G.
Author information
Authors and Affiliations
Contributions
Study design: BMS, RZG, FDHG and CJM. Performed data collection: All authors. Processed data: BMS. Analyzed data: BMS, RZG and CJM. Wrote manuscript: BMS and CJM. Provided comments on manuscript: All authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stricklen, B.M., Bond, L.E., Gould, F.D.H. et al. Swallow Safety in Infant Pigs With and Without Recurrent Laryngeal Nerve Lesion. Dysphagia 35, 978–984 (2020). https://doi.org/10.1007/s00455-020-10099-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-020-10099-x