Abstract
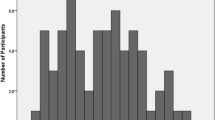
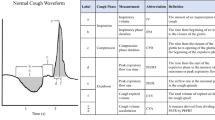
Aspiration pneumonia is a leading cause of death in Parkinson’s disease (PD), occurring as a result of impaired cough and swallowing function. However, portable diagnostic tools for cough assessment and dysphagia screening are limited. Therefore, the aims of this study were to determine if: (1) ‘Handheld Cough Testing’ (HCT), a novel tool developed for cough assessments, could detect differences in cough airflow and sensation during reflex and voluntary cough tasks; and (2) HCT could screen for dysphagia in PD with high sensitivity. Twenty-two people with PD underwent HCT and swallowing assessments. Cough airflow (‘PEFR’) and sensation (‘UTC’) was recorded during reflex and voluntary cough tasks. Flexible endoscopy was used to identify people with and without dysphagia. Within-subject statistical analyses were used to detect differences in PEFR and UTC across cough tasks and between-subject statistical analyses were used to detect differences in cough function between people with and without dysphagia. Results revealed significant differences in PEFR (p < 0.0005) and UTC (p < 0.0005) across cough tasks using HCT. Additionally, reflex cough PEFR was significantly different between people with and without dysphagia (p < 0.05). A cut-off of 42.5 L/min exhibited an excellent ability to predict dysphagia in people with PD (90.9% sensitivity; 80.0% specificity). This study revealed that HCT was a valid tool for cough assessment and dysphagia screening. It identified differences in cough airflow and sensation during reflex and voluntary cough tasks and screened for people with dysphagia in PD with high sensitivity.



Similar content being viewed by others
References
Fall PA, Saleh A, Fredrickson M, Olsson JE, Granérus AK. Survival time, mortality, and cause of death in elderly patients with Parkinson’s disease: a 9-year follow-up. Mov Disord. 2003;18(11):1312–6. https://doi.org/10.1002/mds.10537.
Beyer MK, Herlofson K, Arsland D, Larsen JP. Causes of death in a community-based study of Parkinson’s disease. Acta Neurol Scand. 2001;103(1):7–11. https://doi.org/10.1034/j.1600-0404.2001.00191.x.
Wirdefeldt K, Adami HO, Cole P, Trichopoulos D, Mandel J. Epidemiology and etiology of Parkinson’s disease: a review of the evidence. Eur J Epidemiol. 2011;26(s1):S1–S58. https://doi.org/10.1007/s10654-011-9581-6.
Pinter B, Diem-Zangerl A, Karl Wenning G, et al. Mortality in Parkinson’s disease: a 38-year follow-up study. Mov Disord. 2015;30(2):266–9. https://doi.org/10.1111/cge.12355.
Troche MS, Brandimore AE, Okun MS, Davenport PW, Hegland KW. Decreased cough sensitivity and aspiration in Parkinson disease. Chest. 2014;146(5):106. https://doi.org/10.1378/chest.14-0066.
Troche MS, Schumann B, Brandimore AE, Okun MS, Hegland KW. Reflex cough and disease duration as predictors of swallowing dysfunction in Parkinson’s disease. Dysphagia. 2016;31:757–64. https://doi.org/10.1007/s00455-016-9734-6.
Leow LP, Beckert L, Anderson T, Huckabee ML. Changes in chemosensitivity and mechanosensitivity in aging and Parkinson’s disease. Dysphagia. 2012;27:106–14. https://doi.org/10.1007/s00455-011-9347-z.
Nienstedt JC, Bihler M, Niessen A, et al. Predictive clinical factors for penetration and aspiration in Parkinson’s disease. Neurogastroenterol Motil. 2018. https://doi.org/10.1111/nmo.13524.
Hegland KW, Troche MS, Brandimore A. Relationship between respiratory sensory perception, speech, and swallow in Parkinson’s disease. Mov Disord Clin Pract. 2019;6(3):243–9. https://doi.org/10.1002/mdc3.12732.
Suttrup I, Warnecke T. Dysphagia in Parkinson’s disease. Dysphagia. 2016;31:24–322. https://doi.org/10.1007/s00455-015-9671-9.
Smith Hammond C, Goldstein L, Zajac D, Davenport P, Bolser D. Assessment of aspiration risk in stroke patients with quantification of voluntary cough. Neurology. 2001;56:502–6.
Hammond CAS, Goldstein LB, Horner RD, et al. Predicting aspiration in patients with ischemic stroke. Chest. 2009. https://doi.org/10.1378/chest.08-1122.
Plowman EK, Watts SA, Robison R, et al. Voluntary cough airflow differentiates safe versus unsafe swallowing in amyotrophic lateral sclerosis. Dysphagia. 2016;31:383–90. https://doi.org/10.1007/s00455-015-9687-1.
Silverman EP, Carnaby G, Singletary F, Hoffman-Ruddy B, Yeager J, Sapienza C. Measurement of voluntary cough production and airway protection in parkinson disease. Arch Phys Med Rehabil. 2016;97(3):413–20. https://doi.org/10.1016/j.apmr.2015.10.098.
Ebihara S, Saito H, Kanda A, et al. Impaired efficacy of cough in patients with Parkinson disease. Chest. 2003;124(3):1009–155. https://doi.org/10.1378/chest.124.3.1009.
Pitts T, Troche M, Mann G, Rosenbek J, Okun MS, Sapienza C. Using voluntary cough to detect penetration and aspiration during oropharyngeal swallowing in patients with Parkinson disease. Chest. 2010;138(6):1426–31. https://doi.org/10.1378/chest.10-0342.
Fontana GA, Pantaleo T, Lavorini F, Benvenuti F, Gangem S, Gangemi S. Defective motor control of coughing in Parkinson’s disease. Am J Respir Crit Care Med. 1998;158:458–64.
Wheeler Hegland K, Troche MS, Brandimore AE, Davenport PW, Okun MS. Comparison of voluntary and reflex cough effectiveness in Parkinson’s disease. Park Relat Disord. 2014;20:1226–300. https://doi.org/10.1016/j.parkreldis.2014.09.010.
Yamanda S, Ebihara S, Ebihara T, et al. Impaired urge-to-cough in elderly patients with aspiration pneumonia. Cough. 2008. https://doi.org/10.1186/1745-9974-4-11.
Hegland KW, Troche MS, Brandimore A, Okun MS, Davenport PW. Comparison of two methods for inducing reflex cough in patients with Parkinson’s disease with and without dysphagia. Dysphagia. 2016;31:66–73. https://doi.org/10.1007/s00455-015-9659-5.
Lee JY, Kim DK, Seo KM, Kang SH. Usefulness of the simplified cough test in evaluating cough reflex sensitivity as a screening test for silent aspiration. Ann Rehabil Med. 2014;38(4):476. https://doi.org/10.5535/arm.2014.38.4.476.
Wakasugi Y, Tohara H, Nakane A, et al. Usefulness of a handheld nebulizer in cough test to screen for silent aspiration. Odontology. 2014. https://doi.org/10.1007/s10266-012-0085-y.
Miles A, Moore S, McFarlane M, Lee F, Allen J, Huckabee ML. Comparison of cough reflex test against instrumental assessment of aspiration. Physiol Behav. 2013;118:25–31. https://doi.org/10.1016/j.physbeh.2013.05.004.
Imoto Y, Kojima A, Osawa Y, Sunaga H, Fujieda S. Cough reflex induced by capsaicin inhalation in patients with dysphagia. Acta Otolaryngol. 2010;131(1):96–100. https://doi.org/10.3109/00016489.2010.516013.
Addington WR, Stephens RE, Gilliland K, Rodriguez M. Assessing the laryngeal cough reflex and the risk of developing pneumonia after stroke. Arch Phys Med Rehabil. 1999. https://doi.org/10.1016/S0003-9993(99)90112-0.
Perry SE, Miles A, Fink JN, Huckabee ML. The dysphagia in stroke protocol reduces aspiration pneumonia in patients with dysphagia following acute stroke: a clinical audit. Transl Stroke Res. 2019;10(1):36–433. https://doi.org/10.1007/s12975-018-0625-z.
Pitts T, Bolser D, Rosenbek J, Troche M, Sapienza C. Voluntary cough production and swallow dysfunction in Parkinson’s disease. Dysphagia. 2008;23:297–301. https://doi.org/10.1007/s00455-007-9144-x.
Guillen-Sola A, Chiarella SC, Martinez-Orfila J, et al. Usefulness of citric cough test for screening of silent aspiration in subacute stroke patients: a prospective study. Arch Phys Med Rehabil. 2015;96:1277–83. https://doi.org/10.1016/j.apmr.2015.02.028.
Curtis J, Perry S, Troche MS. Detection of airway invasion during flexible endoscopic evaluations of swallowing: comparing barium, blue dye, and green dye. Am J Speech Lang Pathol. 2019. https://doi.org/10.1044/2018_AJSLP-18-0119.
Jordan Hazelwood R, Hill EG, Bonilha HS, Armeson KE, Martin-Harris B. Identification of swallowing tasks from a modified barium swallow study that optimize the detection of physiological impairment. J Speech Lang Hear Res. 2017;60:1855–63. https://doi.org/10.1044/2017_jslhr-s-16-0117.
Rosenbek JC, Robbins J, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
Hosmer DWJ, Lemeshow S, Sturdivant RX. Applied logistic regression. 3rd ed. Hoboken: Wiley; 2013.
Hammond CAS, Goldstein LB. Cough and aspiration of food and liquids due to oral-pharyngeal dysphagia: ACCP evidence-based clinical practice guidelines. Dysphagia. 2006;129(1):154S–68S.
Troche MS, Brandimore AE, Godoy J, Hegland KW. A framework for understanding shared substrates of airway protection. J Appl Oral Sci. 2014;22(4):251–60. https://doi.org/10.1590/1678-775720140132.
Hammond CAS, Goldstein LB, Horner RD, et al. Predicting aspiration in patients with ischemic stroke: comparison of clinical signs and aerodynamic measures of voluntary cough. Chest. 2009;135:769–77.
Davenport PW. Clinical cough I: the urge-to-cough: a respiratory sensation. In: Chung KF, Widdicombe J, editors. Handbook of experimental pharmacology. Berlin: Springer; 2009. p. 263–276.
Davenport PW, Bolser DC, Vickroy T, et al. The effect of codeine on the urge-to-cough response to inhaled capsaicin. Pulm Pharmacol Ther. 2007;20:338–46. https://doi.org/10.1016/j.pupt.2006.10.012.
Smith JA, Aliverti A, Quaranta M, et al. Chest wall dynamics during voluntary and induced cough in healthy volunteers. J Physiol. 2012;590(3):563–74. https://doi.org/10.1113/jphysiol.2011.213157.
Acknowledgements
The authors would like to acknowledge Jordanna Sevitz, M.S., CCC-SLP for her contribution to data collection.
Funding
This work was supported in part by Grant funds to Dr. Michelle Troche from the Michael J. Fox Foundation.
Author information
Authors and Affiliations
Contributions
JC takes full responsibility for the content of the manuscript, including the accuracy of the data and analysis. JC proposed the study concept and design, collected all data, performed the statistical analyses, and prepared the manuscript for publication. MT contributed to study design, had access to all the data, and assisted in data analysis and manuscript preparation.
Corresponding author
Ethics declarations
Conflict of interest
J.C. has no disclosures to endorse; M.T. receives employee salary from Teachers College, Columbia employee, and Grant funding from the Michael J. Fox Foundation and the CurePSP Foundation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Curtis, J.A., Troche, M.S. Handheld Cough Testing: A Novel Tool for Cough Assessment and Dysphagia Screening. Dysphagia 35, 993–1000 (2020). https://doi.org/10.1007/s00455-020-10097-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-020-10097-z