Abstract
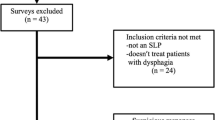
Growing patient numbers, within a context of finite resources, has placed increased demands on dysphagia services in acute settings. Delegating some aspects of dysphagia management to other trained professional groups, such as allied health assistants (AHA), may help speech-language pathology (SLP) service efficiencies. The primary aim of this study was to explore the feasibility and initial validity of using trained AHAs to complete structured mealtime observations of patients. The secondary aims were to explore costs and user perceptions. The study used a mixed methods design. All AHAs who participated worked in the adult acute inpatient setting and were agreeable to participate; they successfully completed training and were deemed competent to use the observation tool. To explore validity, trained AHAs (n = 7) and SLPs (n = 5) conducted independent, simultaneous mealtime observations of 50 adult inpatients, using a structured observation form. Costs of AHA versus SLP time per average assessment were compared. Consumer perceptions were examined in semi-structured interviews with the AHA (n = 5) and SLP participants (n = 3). Exact agreement between AHA and SLPs on the overall pass/fail criteria was high (94%). Where exact agreement was not achieved, the AHA had made a more conservative decision. Salary costs and time savings for the SLP were identified. Interviews identified that both SLPs and AHAs perceived multiple positive personal and service benefits. High levels of agreement in clinical decisions and positive staff perceptions support feasibility and initial clinical validity. This model may assist SP efficiencies in services with high patient demand.
Similar content being viewed by others
References
Altman KW, Yu G-P, Schaefer SD. Consequence of dysphagia in the hospitalized patient: impact on prognosis and hospital resources. Arch Otolaryngol-Head Neck Surg. 2010;136:784–9.
Bonilha HS, Simpson AN, Ellis C, Mauldin P, Martin-Harris B, Simpson K. The one-year attributable cost of post-stroke dysphagia. Dysphagia. 2014;29:545–52.
Davenport R, Dennis M, Wellwood I, Warlow CP. Complications after acute stroke. Stroke. 1996;27:415–20.
Guyomard V, Fulcher RA, Redmayne O, Metcalf AK, Potter JF, Myint PK. Effect of dysphasia and dysphagia on inpatient mortality and hospital length of stay: a database study. J Am Geriatr Soc. 2009;57:2101–6.
Katzan I, Cebul R, Husak S, Dawson N, Baker D. The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology. 2003;60:620–5.
Patel D, Krishnaswami S, Steger E, Conover E, Vaezi M, Ciucci M, Francis D. Economic and survival burden of dysphagia among inpatients in the United States. Diseases of the Esophagus, 2017.
Hammond CAS, Goldstein LB. Cough and aspiration of food and liquids due to oral-pharyngeal dysphagia: ACCP evidence-based clinical practice guidelines. Chest. 2006;129:154S–68S.
Australia SP. Dysphagia: general position paper. Melbourne: The Speech Pathology Association of Australia Limited; 2004.
Association AS-L-H. SLP health care survey: caseload characteristics. Rockville: Association AS-L-H; 2011.
Armstrong E. Communication culture in acute speech pathology settings: Current issues. Adv Speech Lang Pathol. 2003;5:137–43.
Code C, Heron C. Services for aphasia, other acquired adult neurogenic communication and swallowing disorders in the United Kingdom, 2000. Disabil Rehabil. 2003;25:1231–7.
Enderby P, Petheram B. Has aphasia therapy been swallowed up? Clin Rehabil. 2002;16:604–8.
Foster A, O’Halloran R, Rose M, Worrall L. “Communication is taking a back seat”: speech pathologists’ perceptions of aphasia management in acute hospital settings. Aphasiology. 2016;30:585–608.
Kamal RM, Ward E, Cornwell P. Dysphagia management practices among speech-language pathologists in Malaysia. Asia Pac J Speech Lang Hear. 2012;15:111–28.
Clavé P, Arreola V, Romea M, Medina L, Palomera E, Serra-Prat M. Accuracy of the volume-viscosity swallow test for clinical screening of oropharyngeal dysphagia and aspiration. Clin Nutr. 2008;27:806–15.
Morishima Y, Chida K, Watanabe H. Estimation of the dose of radiation received by patient and physician during a videofluoroscopic swallowing study. Dysphagia. 2016;31:574–8.
Chau KHT, Kung CMA. Patient dose during videofluoroscopy swallowing studies in a Hong Kong public hospital. Dysphagia. 2009;24:387.
Kim HM, Choi KH, Kim TW. Patients’ radiation dose during videofluoroscopic swallowing studies according to underlying characteristics. Dysphagia. 2013;28:153–8.
Steele CM, Greenwood C, Ens I, Robertson C, Seidman-Carlson R. Mealtime difficulties in a home for the aged: not just dysphagia. Dysphagia. 1997;12:43–50.
Miller N, Patterson J. Dysphagia: implications for older people. Rev Clin Gerontol. 2014;24:41–57.
Hines S, Kynoch K, Munday J. Nursing interventions for identifying and managing acute dysphagia are effective for improving patient outcomes: a systematic review update. J Neurosci Nurs. 2016;48:215–23.
Hines S, Wallace K, Crowe L, Finlayson K, Chang A, Pattie M. Identification and nursing management of dysphagia in individuals with acute neurological impairment (update). Int J Evid-Based Healthc. 2011;9:148–50.
Pelletier CA. What do certified nurse assistants actually know about dysphagia and feeding nursing home residents? Am J Speech-Lang Pathol. 2004;13:99–113.
Simmons SF, Keeler E, Zhuo X, Hickey KA, Sato HW, Schnelle JF. Prevention of unintentional weight loss in nursing home residents: a controlled trial of feeding assistance. J Am Geriatr Soc. 2008;56:1466–73.
Simmons SF, Schnelle JF. Feeding assistance needs of long-stay nursing home residents and staff time to provide care. J Am Geriatr Soc. 2006;54:919–24.
Lizarondo L, Kumar S, Hyde L, Skidmore D. Allied health assistants and what they do: a systematic review of the literature. J Multidiscip Healthc. 2010;3:143.
Stanmore E, Waterman H. Crossing professional and organizational boundaries: the implementation of generic rehabilitation assistants within three organizations in the northwest of England. Disabil Rehabil. 2007;29:751–9.
Davenport SJ, Arnold M, Hua C, Schenck A, Batten S, Taylor NF. Physical activity levels during acute inpatient admission after hip fracture are very low. Physiother Res Int. 2015;20:174–81.
Ward EC, Burns CL. Dysphagia management via telerehabilitation: a review of the current evidence. J Gastroenterol Hepatol Res 3, 2014.
Sharma S, Ward EC, Burns C, Theodoros D, Russell T. Training the allied health assistant for the telerehabilitation assessment of dysphagia. J Telemed Telecare. 2012;18:287–91.
Martino R, Pron G, Diamant NE. Oropharyngeal dysphagia: surveying practice patterns of the speech–language pathologist. Dysphagia. 2004;19:165–76.
Ramsey DJ, Smithard DG, Kalra L. Early assessments of dysphagia and aspiration risk in acute stroke patients. Stroke. 2003;34:1252–7.
Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval. 2006;27:237–46.
Creswell JW. Research design: qualitative, quantitative, and mixed methods approaches. London: Sage; 2013.
McHugh ML. Interrater reliability: the kappa statistic. Biochemia medica. 2012;22:276–82.
Munn Z, Tufanaru C, Aromataris E. Recognition of the health assistant as a delegated clinical role and their inclusion in models of care: a systematic review and meta-synthesis of qualitative evidence. Int J Evid-Based Healthc. 2013;11:3–19.
Nancarrow SA, Roots A, Grace S, Moran AM, Vanniekerk-Lyons K. Implementing large-scale workforce change: learning from 55 pilot sites of allied health workforce redesign in Queensland, Australia. Hum Resour Health. 2013;11:66.
Acknowledgements
The authors extend their thanks to the speech pathology and allied health assistant staff who helped to conduct training and participated in the data collection for this research.
Funding
The study was funded by the Queensland Health, Health Practitioners Research Grant (2015/2016).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schwarz, M., Ward, E.C., Cornwell, P. et al. Evaluating the Feasibility and Validity of Using Trained Allied Health Assistants to Assist in Mealtime Monitoring of Dysphagic Patients. Dysphagia 34, 350–359 (2019). https://doi.org/10.1007/s00455-018-9947-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-018-9947-y