Abstract
Introduction
Some stroke patients show oral phase dysphagia, characterized by a markedly prolonged oral transit time that hinders oral feeding. The aim of this study was to clarify the clinical characteristics and lesions responsible for delayed swallowing.
Methods
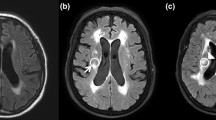
We reviewed 90 patients with stroke. The oral processing time plus the postfaucial aggregation time required to swallow semisolid food was assessed. The patients were divided into two groups according to oral transit time, and we analyzed the differences in characteristics such as demographic factors, lesion factors, and cognitive function. Logistic regression analyses were performed to examine the predictors of delayed oral transit time. Lesion location and volume were measured on brain magnetic resonance images. We generated statistic maps of lesions related to delayed oral phase in swallowing using voxel-based lesion symptom mapping (VLSM).
Results
The group of patients who showed delayed oral transit time had significantly low cognitive function. Also, in a regression model, delayed oral phase was predicted with low K-MMSE (Korean version of the Mini Mental Status Exam). Using VLSM, we found the lesion location to be associated with delayed oral phase after adjusting for K-MMSE score. Although these results did not reach statistical significance, they showed the lesion pattern with predominant distribution in the left frontal lobe.
Conclusion
Delayed oral phase in post-stroke patients was not negligible clinically. Patients’ cognitive impairments affect the oral transit time. When adjusting it, we found a trend that the lesion responsible for delayed oral phase was located in the left frontal lobe, though the association did not reach significance. The delay might be related to praxis function.


Similar content being viewed by others
References
Sturm JW, Dewey HM, Donnan GA, Macdonell RA, McNeil JJ, Thrift AG. Handicap after stroke: how does it relate to disability, perception of recovery, and stroke subtype?: the North East Melbourne Stroke Incidence Study (NEMESIS). Stroke. 2002;33(3):762–8.
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36(12):2756–63.
Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest. 2003;124(1):328–36.
Moon HI, Pyun SB, Kwon HK. Correlation between location of brain lesion and cognitive function and findings of videofluoroscopic swallowing study. Ann Rehabil Med. 2012;36(3):347–55.
Robbins J, Levine RL, Maser A, Rosenbek JC, Kempster GB. Swallowing after unilateral stroke of the cerebral cortex. Arch Phys Med Rehabil. 1993;74(12):1295–300.
Ikenaga Y, Nakayama S, Taniguchi H, Ohori I, Komatsu N, Nishimura H, et al. Factors predicting recovery of oral intake in stroke survivors with dysphagia in a convalescent rehabilitation ward. J Stroke Cerebrovasc Dis. 2017;26(5):1013–9.
Saito T, Hayashi K, Nakazawa H, Ota T. Clinical characteristics and lesions responsible for swallowing hesitation after acute cerebral infarction. Dysphagia. 2016;31(4):567–73.
Bates E, Wilson SM, Saygin AP, Dick F, Sereno MI, Knight RT, et al. Voxel-based lesion-symptom mapping. Nat Neurosci. 2003;6(5):448–50.
Logemann JA. Swallowing physiology and pathophysiology. Otolaryngol Clin North Am. 1988;21(4):613–23.
Palmer JB. Bolus aggregation in the oropharynx does not depend on gravity. Arch Phys Med Rehabil. 1998;79(6):691–6.
Hiiemae KM, Palmer JB. Food transport and bolus formation during complete feeding sequences on foods of different initial consistency. Dysphagia. 1999;14(1):31–42.
Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86(8):1516–20.
Barer DH. The natural history and functional consequences of dysphagia after hemispheric stroke. J Neurol Neurosurg Psychiatry. 1989;52(2):236–41.
Kojima A, Imoto Y, Osawa Y, Fujieda S. Predictor of rehabilitation outcome for dysphagia. Auris Nasus Larynx. 2014;41(3):294–8.
Secil Y, Arici S, Incesu TK, Gurgor N, Beckmann Y, Ertekin C. Dysphagia in Alzheimer’s disease. Neurophysiol Clin. 2016;46(3):171–8.
Boccardi V, Ruggiero C, Patriti A, Marano L. Diagnostic Assessment and Management of Dysphagia in Patients with Alzheimer’s Disease. J Alzheimers Dis. 2016;50(4):947–55.
Suntrup S, Kemmling A, Warnecke T, Hamacher C, Oelenberg S, Niederstadt T, et al. The impact of lesion location on dysphagia incidence, pattern and complications in acute stroke. Part 1: dysphagia incidence, severity and aspiration. Eur J Neurol. 2015;22(5):832–8.
Suntrup-Krueger S, Kemmling A, Warnecke T, Hamacher C, Oelenberg S, Niederstadt T, et al. The impact of lesion location on dysphagia incidence, pattern and complications in acute stroke. Part 2: Oropharyngeal residue, swallow and cough response, and pneumonia. Eur J Neurol. 2017;24(6):867–74.
Jernigan TL, Gamst AC, Fennema-Notestine C, Ostergaard AL. More “mapping” in brain mapping: statistical comparison of effects. Hum Brain Mapp. 2003;19(2):90–5.
Yang Y, Raine A. Prefrontal structural and functional brain imaging findings in antisocial, violent, and psychopathic individuals: a meta-analysis. Psychiatr Res. 2009;174(2):81–8.
Graff-Radford J, Jones DT, Strand EA, Rabinstein AA, Duffy JR, Josephs KA. The neuroanatomy of pure apraxia of speech in stroke. Brain Lang. 2014;129:43–6.
Hamdy S, Mikulis DJ, Crawley A, Xue S, Lau H, Henry S, et al. Cortical activation during human volitional swallowing: an event-related fMRI study. Am J Physiol. 1999;277(1 Pt 1):G219–25.
Hamdy S, Rothwell JC, Brooks DJ, Bailey D, Aziz Q, Thompson DG. Identification of the cerebral loci processing human swallowing with H2(15)O PET activation. J Neurophysiol. 1999;81(4):1917–26.
Suzuki M, Asada Y, Ito J, Hayashi K, Inoue H, Kitano H. Activation of cerebellum and basal ganglia on volitional swallowing detected by functional magnetic resonance imaging. Dysphagia. 2003;18(2):71–7.
Lowell SY, Reynolds RC, Chen G, Horwitz B, Ludlow CL. Functional connectivity and laterality of the motor and sensory components in the volitional swallowing network. Exp Brain Res. 2012;219(1):85–96.
Daniels SK, Foundas AL. The role of the insular cortex in dysphagia. Dysphagia. 1997;12(3):146–56.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Moon, H.I., Yoon, S.Y., Yi, T.I. et al. Lesions Responsible for Delayed Oral Transit Time in Post-stroke Dysphagia. Dysphagia 33, 321–328 (2018). https://doi.org/10.1007/s00455-017-9856-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-017-9856-5