Abstract
In 2017, it was 200 years since James Parkinson published ‘An Essay on the Shaking Palsy’ and 20 years since α-synuclein aggregation came to the fore. In 1998, multiple system atrophy joined Parkinson’s disease and dementia with Lewy bodies as the third major synucleinopathy. Here, we describe the work that led to the identification of α-synuclein in Lewy bodies, Lewy neurites and Papp–Lantos bodies. We also review some of the findings reported since 1997.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 1817, James Parkinson (1755–1824) of Hoxton Square, East London, described the ‘Shaking Palsy’ (Parkinson 1817), a disease that was subsequently named after him (Sanders 1865; Charcot 1875). At the time, the involvement of the substantia nigra and the presence there of Lewy pathology were not known.
Paul Blocq (1860–1896) and Georges Marinesco (1863–1938) of the Salpêtrière Hospital in Paris reported a patient with left-sided parkinsonian tremor who, at autopsy, had an enucleated tuberculoma the size of a hazelnut in the right substantia nigra (Blocq and Marinesco 1893). They also alluded to a case from Jean-Martin Charcot (1825–1893) with hemiparkinsonism caused by a tumour that compressed the cerebral peduncle. This led Edouard Brissaud (1852–1909), Charcot’s successor at the Salpêtrière, to propose, in 1894, that a lesion of the substantia nigra was the anatomical substrate of Parkinson’s disease (PD) (Brissaud and Meige 1895).
In 1919, at the Salpêtrière, Constantin Trétiakoff (1892–1956) reported pathological inclusions that he named ‘corps de Lewy’ in the substantia nigra in PD (Trétiakoff 1919) [similar inclusions had been identified in other brain areas of PD by Fritz Jakob Heinrich Lewy (1885–1950) (Lewy 1912; Goedert et al. 2013)]. Trétiakoff also showed degeneration of the substantia nigra and postulated a link between nerve cell loss, rigidity and tremor. Rolf Hassler (1914–1984) confirmed Trétiakoff’s findings and showed that the ventrolateral tier was the most severely affected part of the substantia nigra (Hassler 1938). He did most of this work at the Kaiser Wilhelm Institute for Brain Research in Berlin, which was directed by Oskar Vogt. Following their dismissal in 1936, Vogt and his wife Cécile built up a new Institute in Neustadt in the Black Forest, where Hassler worked for a number of years. Science is often a young person’s game. Lewy, Marinesco, Trétiakoff and Hassler were 30 years old or less when they made these discoveries.
In 1997, the ordered assembly of α-synuclein came to the fore (Polymeropoulos et al. 1997; Spillantini et al. 1997). Polymeropoulos et al. described a causative mutation (A53T) in SNCA, the α-synuclein gene, in the Contursi kindred and three smaller Greek families with PD, whereas Spillantini et al. reported the presence of α-synuclein in Lewy bodies and Lewy neurites of idiopathic PD and dementia with Lewy bodies (DLB). These findings linked the genetic cause of a rare form of PD with the inclusions in all cases of the disease. They were conceptually similar to those previously obtained in Alzheimer’s disease (AD) (Glenner and Wong 1984; Goate et al. 1991) and some human tauopathies (Pollock et al. 1986; Poorkaj et al. 1998; Hutton et al. 1998; Spillantini et al. 1998a) and helped to underscore the view expressed by William Harvey (1578–1657) and reiterated by Archibald Garrod (1857–1936), that the study of rare forms of disease can inform the more common cases (Garrod 1928). In his letter of April 24, 1657, to John Vlackveld, Harvey wrote: “Nature is nowhere accustomed more openly to display her secret mysteries than in cases where she shows traces of her workings apart from the beaten path; nor is there any better way to advance the proper practice of medicine than to give our minds to the discovery of the usual law of nature, by the careful investigation of cases of rarer forms of disease.” (Harvey and Willis 1847).
α-Synuclein and Lewy pathology
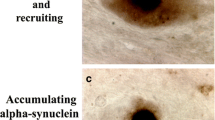
Our findings on α-synuclein (Jakes et al. 1994) grew out of work on tau, which we found to be an integral component of the paired helical and straight filaments of AD in 1988 (Goedert et al. 1988; Wischik et al. 1988a, b). In August 1997, together with Ross Jakes, Marie-Luise Schmidt, Virginia Lee and John Trojanowski, we showed that the Lewy pathology from the substantia nigra of six patients with idiopathic PD and four patients with DLB was strongly immunoreactive for α-synuclein (Fig. 1a–c) (Spillantini et al. 1997). The same was true of the Lewy pathology from the cingulate cortex of DLB. Antibodies specific for the amino- and carboxy-termini of α-synuclein stained the inclusions, consistent with the presence of the whole molecule. An antibody specific for β-synuclein failed to label the inclusions of PD and DLB.
The α-synuclein pathology of Parkinson’s disease. Lewy pathology in the substantia nigra and several other brain regions defines Parkinson’s disease at the neuropathological level. This is shown by light microscopy, labelled by α-synuclein antibodies (a–c). Using immunoelectron microscopy, filaments extracted from the Lewy pathology were decorated by α-synuclein antibodies (d–g). a Two pigmented nerve cells, each containing an α-synuclein-positive Lewy body (red arrows); Lewy neurites (black arrows) are also immunopositive. Scale bar 20 μm. b Pigmented nerve cell with two α-synuclein-positive Lewy bodies. Scale bar 8 μm. c α-Synuclein-positive extracellular Lewy body. Scale bar 4 μm. d–g Isolated filaments from the substantia nigra of patients with Parkinson’s disease are decorated by an antibody directed against the carboxy-terminal (d, e) or the amino-terminal (f, g) region of α-synuclein. The gold particles conjugated to the second antibody appear as black dots. Note the uniform decoration (d, e) and the labelling of only one filament end (f, g). Scale bar 100 nm. From Goedert (2001)
In May 1998, we reported that Lewy neurites were more abundant in PD and DLB than hitherto believed (Spillantini et al. 1998b). The staining of intraneuritic Lewy bodies helped to reinforce the view that the Lewy pathology is not benign. Prior to this work, ubiquitin staining had been the most sensitive means of detecting Lewy pathology but it lacked in specificity, because inclusions made of other proteins can also be ubiquitinated. We showed that staining for α-synuclein was more extensive than staining for ubiquitin, indicating that the assembly of α-synuclein precedes ubiquitination. Similar findings were subsequently reported by others (Hasegawa et al. 2002; Sampathu et al. 2003).
We confirmed that β-synuclein did not accumulate in the Lewy pathology and showed that γ-synuclein was not present either. Of the three mammalian synucleins, only α-synuclein is found in the Lewy pathology. We then studied sarkosyl-insoluble filaments extracted from the cingulate cortex of patients with DLB by immunoelectron microscopy. An antibody specific for the carboxy-terminal region of α-synuclein labelled filaments with a diameter of 5–10 nm and a length of 200–600 nm. An antibody specific for the amino-terminal region only labelled one end of each filament, suggesting that α-synuclein filaments are polar structures. We subsequently reported similar findings on filaments from the substantia nigra of PD patients (Fig. 1d–g) (Crowther et al. 2000).
α-Synuclein and Papp-Lantos bodies
Multiple system atrophy (MSA) is a neurodegenerative disease characterised by a combination of autonomic, cerebellar, parkinsonian, pyramidal and cognitive symptoms (Goedert 2015). It is divided into parkinsonian (MSA-P) and cerebellar (MSA-C) variants. A rarer cortical variant (MSA-FTLD) has also been described. In most countries, MSA-P is the most common form. MSA comprises what used to be called olivopontocerebellar atrophy, striatonigral degeneration and Shy–Drager syndrome.
Inclusions in the cytoplasm of oligodendrocytes (Papp–Lantos bodies) are the major histological hallmark of MSA (Papp et al. 1989). Less often, nuclear inclusions are present, as are neuronal cytoplasmic and nuclear inclusions. Together with Nigel Cairns and Peter Lantos at the Institute of Psychiatry of King’s College London, we showed that glial and neuronal inclusions of MSA contain α-synuclein (Fig. 2a–c) (Spillantini et al. 1998c). The inclusions were stained by antibodies recognising the amino- and carboxy-termini of α-synuclein. By double-labelling, staining for α-synuclein was more extensive than staining for ubiquitin, indicating that the aggregation of α-synuclein preceded ubiquitination. Antibodies against β- and γ-synuclein failed to stain the inclusions. Similar results were reported by others at about the same time (Wakabayashi et al. 1998; Tu et al. 1998).
The α-synuclein pathology of multiple system atrophy. Glial cytoplasmic inclusions in several brain regions define multiple system atrophy. Similar inclusions are also present in the nuclei of some glial cells, as well as in the cytoplasm and nuclei of some nerve cells and in nerve cell processes. Inclusions labelled by α-synuclein antibodies are shown by light microscopy (a–c). Using immunoelectron microscopy, filaments extracted from the inclusions were decorated by α-synuclein antibodies (d–g). a α-Synuclein-immunoreactive cytoplasmic oligodendrocyte inclusions (red arrows) in pontine fibre tracts. b α-Synuclein-immunoreactive nuclear oligodendrocyte inclusion (red arrow) and cytoplasmic nerve cell inclusion (black arrow) in grey matter of frontal cortex. c α-Synuclein-immunoreactive nuclear nerve cell inclusion (black arrow) in grey matter of pons. Scale bars (a) 5 μm, (b) 50 μm, (c) 30 μm. d–g Isolated filaments from the frontal cortex and cerebellum of patients with multiple system atrophy are decorated by antibodies specific for the carboxy-terminal (d, e) and amino-terminal (f, g) regions of α-synuclein. The gold particles conjugated to the second antibody appear as black dots. Note the uniform decoration in (d, e) and the labelling of only one filament end in (f, g). A twisted filament is shown in (d), whereas (e) shows a straight filament. Scale bar 100 nm. Adapted from Goedert (2001)
Filaments from MSA brains had a diameter of 5–18 nm and were strongly labelled by an antibody specific for the carboxy-terminus of α-synuclein (Fig. 2d, e) (Spillantini et al. 1998c). An amino-terminal antibody only labelled one filament end, as was the case in PD and DLB (Fig. 2f, g). This work revealed a molecular link between MSA and Lewy pathology disorders. However, unlike PD and DLB, where α-synuclein filaments are mostly present in the cytoplasm of nerve cells in the form of Lewy bodies and Lewy neurites, in MSA, they are found in the cytoplasm and nuclei of both nerve cells and glial cells. Since 1998, PD, DLB and MSA have frequently been called ‘synucleinopathies’ (Goedert and Spillantini 1998). Filaments assembled from bacterially expressed human α-synuclein are structurally and antigenically similar to those extracted from DLB and MSA brains (Fig. 3) (Crowther et al. 1998; Conway et al. 1998). However, higher-resolution techniques, such as cryogenic electron microscopy, may reveal structural differences between these filaments in the future.
Filaments extracted from the brains of patients with dementia with Lewy bodies (a), multiple system atrophy (b) or assembled from bacterially expressed human α-synuclein (c) were decorated by an anti-α-synuclein antibody. The gold particles conjugated to the second antibody appear as black dots. From Goedert and Spillantini (2012)
Twenty years of synucleinopathies
Lewy pathology is also the defining feature of several rarer diseases, including pure autonomic failure, in which α-synuclein aggregates in the peripheral sympathetic nervous system are the major neuropathological hallmark (Arai et al. 2000). In PD, abundant Lewy pathology is present in the enteric, peripheral and central nervous systems. Some patients presenting clinically with pure autonomic failure go on to develop PD or DLB (Kaufmann et al. 2004). In incidental Lewy body disease, which may be a preclinical form of PD, Lewy pathology is present in the absence of clinical motor symptoms (Iwanaga et al. 1999; Del Tredici et al. 2002; Dickson et al. 2008; Beach et al. 2008). Similarly, cases with oligodendroglial α-synuclein inclusions in the absence of clinical symptoms, akin to preclinical MSA, have been described (Parkkinen et al. 2007; Fujishiro et al. 2008).
The clinical Parkinson’s syndrome is defined as bradykinesia that worsens over time, in conjunction with at least one of three additional features: rigidity, resting tremor or gait disturbance (Jenner et al. 2013; Postuma et al. 2015). At the time of diagnosis, around 30% of dopaminergic neurons in the substantia nigra and 50–60% of their axon terminals have been lost (Cheng et al. 2010), consistent with a centripetal mechanism of aggregate formation and neurodegeneration.
Physiological function of α-synuclein
The physiological function of α-synuclein is incompletely understood. It binds to acidic phospholipids through its amino-terminal repeats (Davidson et al. 1998; Jensen et al. 1998), when it multimerizes and becomes α-helical (Chandra et al. 2003; Ulmer et al. 2005; Jao et al. 2008). About 3500 α-synuclein molecules co-exist with 300 synaptic vesicles in individual synaptic boutons from rat brain (Wilhelm et al. 2014). The presence of α-synuclein in nerve terminals has suggested a role in neurotransmitter release. It has been reported that it promotes dilation of the exocytic fusion pore (Logan et al. 2017). Mitochondria fragment upon α-synuclein expression (Kamp et al. 2010; Nakamura et al. 2011), despite the fact that in nerve cells α-synuclein is concentrated in nerve terminals, whereas most mitochondria localise to nerve cell bodies and dendrites (Bendor et al. 2013).
Loss of SNCA does not lead to a neurodegenerative phenotype (Abeliovich et al. 2000). The existence of three synucleins raised the possibility that redundancy might account for the relatively mild SNCA knockout phenotype. Mice lacking α-, β- and γ-synucleins were subsequently produced (Greten-Harrison et al. 2010; Anwar et al. 2011). They showed an increase in striatal dopamine release beyond that of single knockouts, probably because synaptic vesicles fused more with presynaptic membranes. However, the overall phenotype was relatively mild. No synuclein homologues are found in C. elegans or D. melanogaster.
α-Synuclein inclusions
The core of an α-synuclein filament, which is the sequence required for a filament from human brain to look like a filament by electron microscopy, extends over approximately 70 amino acids (residues 30–100) (Miake et al. 2002; Der-Sarkissian et al. 2003). The crystal structure of residues 68–78 of human α-synuclein showed paired β-sheets with parallel β-strands in each sheet and anti-parallel β-strands between the sheets. The zipper structure that marked the region between paired sheets was longer than in other peptide structures, and each pair of β-sheets contained two water molecules (Rodriguez et al. 2015). Upon assembly, full-length α-synuclein adopts structures rich in β-sheets (Serpell et al. 2000). Recombinant α-synuclein that had been aggregated using a seed from PD brain was studied by solid-state nuclear magnetic resonance, scanning transmission electron microscopy and X-ray diffraction (Tuttle et al. 2016). The core of the filament (residues 44–97) consisted of parallel in-register β-sheets with the topology of a Greek key.
Assembly of α-synuclein is nucleation-dependent. Deletion of residues 71–82 abolished the ability to assemble into filaments (Giasson et al. 2001); these residues are located in the innermost β-sheet of the core (Tuttle et al. 2016). Deletion of residues 66–74 also prevented assembly (Du et al. 2003), whereas the absence of the carboxy-terminal region promoted assembly (Crowther et al. 1998).
Genetics of SNCA
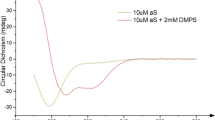
Seven dominantly inherited missense mutations in SNCA have been described as the cause of familial PD (Fig. 4). Besides A53T, they include A30P (Krüger et al. 1998), E46K (Zarranz et al. 2003), H50Q (Appel-Cresswell et al. 2013; Proukakis et al. 2013), G51D (Kiely et al. 2013; Lesage et al. 2013), A53E (Pasanen et al. 2014; Martikainen et al. 2015) and A53V (Yoshino et al. 2017). The age of disease onset can be variable, even within families but mutations G51D, A53E and A53T give rise to the earliest onset. Experimentally, mutations E46K, H50Q and A53T increase α-synuclein inclusion formation (Serpell et al. 2000; Choi et al. 2004; Ghosh et al. 2013), whereas mutations A30P, G51D and A53E (Narhi et al. 1999; Bilal-Fares et al. 2014; Ghosh et al. 2014; Rutherford et al. 2014) reduce aggregation rates. Mutations A30P, G51D and A53E also lead to a reduced ability of mutant α-synuclein to interact with acidic phospholipids (Chandra et al. 2003; Bilal-Fares et al. 2014; Ghosh et al. 2014; Ysselstein et al. 2015). These findings are consistent with work that has suggested an antagonistic relationship between lipid binding of α-synuclein and aggregation into cytotoxic species (Burré et al. 2015; Iljina et al. 2016; Cremades et al. 2012).
Human α-synuclein and its disease-causing mutations. a Diagram of the 140 amino acid human α-synuclein. The seven amino-terminal repeats are shown as blue bars. b A dominantly inherited increase in gene dosage (duplication or triplication) of the chromosomal region containing SNCA gives rise to Parkinson’s disease and dementia with Lewy bodies. Homozygous duplications have also been described. In addition, missense mutations in SNCA cause dominantly inherited forms of Parkinson’s disease and dementia with Lewy bodies. c The repeats (residues 7–87) of human α-synuclein are shown, with disease-causing mutations (A30P, E46K, H50Q, G51D, A53E, A53T and A53V) given as blue letters. Amino acids that are identical in at least five of the seven repeats are shaded in blue
Dominantly inherited duplications and triplications of the chromosomal region that contains SNCA have also been found to cause PD (Fig. 4) (Singleton et al. 2003; Chartier-Harlin et al. 2004; Ibánez et al. 2004). A homozygous duplication of SNCA has been described (Ikeuchi et al. 2008). The sequence of α-synuclein was wild-type, showing that an increase in protein levels rather than a change in its properties is sufficient to cause PD. Heterozygous duplications of SNCA gave rise to a form of PD that was similar to the sporadic disorder in terms of age of onset and symptoms but triplication caused a more severe phenotype, with an earlier age of onset and prominent cognitive impairment.
Individuals with the A53T mutation in SNCA developed a severe form of PD that was often accompanied by dementia. A clinical picture resembling DLB was characteristic of a family with the E46K mutation, whereas individuals from the family with the A30P mutation developed late-onset PD and had only mild dementia. Neuropathologically, some individuals, in particular those with mutations G51D and A53E, had features of both PD and MSA. This overlap of clinical and neuropathological characteristics supports the view that the aetiologies of PD, DLB and MSA are closely related.
Heterozygous mutations in the gene encoding leucine-rich repeat kinase 2 (LRRK2) are the most common cause of dominantly inherited PD (Paisán-Ruiz et al. 2004; Zimprich et al. 2004). LRRK2 is a multidomain protein of 2527 amino acids with two enzymatic activities (guanosine triphosphatase and protein kinase) and multiple protein–protein interaction domains. G2019S, the most common mutation, increases LRRK2’s kinase activity 2- to 3-fold. Disease penetrance is incomplete. Some Rab GTPases are prominent LRRK2 targets (Steger et al. 2016) and their increased phosphorylation may result in disturbed vesicle trafficking. Moreover, mutations in the gene encoding TMEM230, a transmembrane protein of synaptic vesicles, give rise to inherited PD (Deng et al. 2016). The resulting impairment of vesicle trafficking may impair the degradation of α-synuclein, resulting in a net effect not unlike that of gene dosage mutations.
Genome-wide association studies (GWAS) of risk in idiopathic PD showed that SNCA makes the largest contribution. The implicated polymorphisms lie outside the coding region and thus probably affect mRNA expression, resulting in increased expression of α-synuclein (Satake et al. 2009; Simón-Sánchez et al. 2009; Nalls et al. 2014). Variability in LRRK2, GAK (cyclin G-associated kinase) and MAPT (microtubule-associated protein tau) has also been implicated. Variants in SNCA and MAPT have been reported as risk factors for MSA (Scholz et al. 2009; Al-Chalabi et al. 2009; Vilarino-Güell et al. 2011). However, a GWAS of risk in MSA failed to confirm these findings (Sailer et al. 2016). None of the studied variants were statistically significant. The estimated heritability of MSA is lower than that of PD (Federoff et al. 2016).
The most common genetic risk factor for idiopathic PD and DLB, missense mutations in one or both alleles of GBA1, the glucocerebrosidase gene, was not discovered using GWAS but through clinical studies (Neudorfer et al. 1996; Aflaki et al. 2017). GBA1 encodes glucocerebrosidase, which degrades glucosylceramide into glucose and ceramide. Homozygous loss-of-function mutations in GBA1 cause Gaucher’s disease, a lysosomal storage disorder. Approximately 7% of patients with PD carry mutations in GBA1. Conversely, 5–7% of patients with Gaucher’s disease develop PD before the age of 70. The mechanistic links between glucocerebrosidase and α-synuclein are unclear but there appears to be an inverse correlation between the levels of glucocerebrosidase and α-synuclein (Mazzulli et al. 2011). Experimental evidence supports a direct interaction between α-synuclein and glucocerebrosidase (Yap et al. 2011). Mutations in GBA1 may also predispose to MSA (Mitsui et al. 2015).
Propagation of α-synuclein aggregates
Evidence for the existence of prion-like mechanisms in diseased human brain has come from the development of scattered Lewy pathology in foetal human midbrain neurons that were therapeutically implanted into the striata of patients with advanced PD (Li et al. 2008; Kordower et al. 2008). Lewy pathology was detected in 2–5% of grafted cells 10 or more years after transplantation, approximately the same percentage as that of neurons with Lewy pathology in the pars compacta of the substantia nigra in PD. After 24 years, 11–12% of grafted dopaminergic neurons exhibited α-synuclein- and ubiquitin-positive inclusions (Li et al. 2016).
Over the past 8 years, experimental studies have shown that the intracerebral injection of α-synuclein assemblies from diseased human brains or recombinant proteins induces nerve cells to form intracellular inclusions at the injection sites, from where they can spread to distant brain regions (Goedert 2015; Shimozawa et al. 2017). Moreover, the peripheral injection of α-synuclein aggregates assembled from recombinant protein caused α-synuclein pathology and neurodegeneration in the central nervous system of transgenic but not wild-type, mice (Breid et al. 2016; Ayers et al. 2017). Using long-term in vivo imaging, aggregated recombinant α-synuclein was shown to seed the ordered assembly of expressed α-synuclein in brain (Osterberg et al. 2015). Inclusion-bearing neurons degenerated, demonstrating that inclusion formation was linked to cellular toxicity. In the substantia nigra from PD patients, the proportion of Lewy body-containing neurons is approximately 4%. The inclusions are probably degraded when the neurons that bear them die. In a model in which neurons are killed by the Lewy pathology, it has been estimated that the mean survival time of an eosinophilic Lewy body is of the order of 6 months (Greffard et al. 2010).
Some morphological differences between disease-associated α-synuclein filaments have been described (Spillantini et al. 1998b). Lewy pathology was positive by Campbell–Switzer silver but not Gallyas–Braak silver (Uchihara et al. 2005a). The same has been shown to be the case of inclusions made of tau isoforms with 3 repeats (Uchihara et al. 2005b). By contrast, the glial cytoplasmic inclusions of MSA were positive by both Campbell–Switzer and Gallyas–Braak silver, like inclusions made of all 6 tau isoforms. Inclusions made of tau isoforms with 4 repeats are only positive with Gallyas–Braak silver. Brain extracts from MSA patients propagated in heterozygous mice transgenic for human A53T α-synuclein, in contrast to brain extracts from PD patients (Woerman et al. 2015; Prusiner et al. 2015). However, unlike in MSA, α-synuclein inclusions were exclusively neuronal.
Despite an increased understanding of the pathogenesis of MSA, the origin of glial α-synuclein aggregates is still unclear. Ordered assembly is concentration-dependent and, until recently, it was believed that mature oligodendrocytes did not express α-synuclein. However, a study based on single-cell capture and quantitative real-time PCR has challenged this view (Asi et al. 2014). It pointed to the possibility that α-synuclein aggregates characteristic of GCIs might be of oligodendroglial origin. Cell-to-cell transfer might also play a role, since oligodendrocytes have been shown to take up α-synuclein assemblies (Kisos et al. 2012; Reyes et al. 2014). It remains to be seen if MSA is a primary gliopathy with neurons involved secondarily, or if it is a primary neuronal problem with glial cells affected secondarily.
Polymorphs of recombinant aggregated α-synuclein in the form of ribbons and fibrils have been described (Bousset et al. 2013). When injected into the rat substantia nigra, the ribbons gave rise to Lewy pathology, whereas the fibrils, which did not seed Lewy pathology, led to the loss of dopaminergic neurons (Peelaerts et al. 2015). It remains to be seen if ribbons and fibrils have their counterparts in human synucleinopathies. In a separate work, some α-synuclein filaments seeded both tau and α-synuclein aggregation, whereas others only seeded α-synuclein aggregation (Guo et al. 2013). These conformers of aggregated α-synuclein exhibited different properties after proteinase K digestion. They were similar to prion strains, in that they showed structural variations, differences in seeding properties and heritability of phenotypic traits.
Conclusion
The ordered assembly of α-synuclein has proved to be central to PD, DLB and MSA. Understanding disease aetiology and pathogenesis will probably be necessary for the development of safe and effective mechanism-based therapies that are superior to what is currently available. This is a tall order for PD, where L-DOPA has proved to be a good symptomatic therapy for the motor symptoms, at least for some time during the course of the disease. Perhaps future treatments aimed at slowing down or arresting the progression of PD will be complementary to L-DOPA. Although the diagnosis of PD relies on the motor effects of a deficient function of the substantia nigra, there are also non-motor symptoms, such as hyposmia (Ansari and Johnson 1975), REM sleep behaviour disorder (Schenck et al. 1986), depression and constipation, which can precede the motor symptoms by several years (Schapira and Tolosa 2010). The presence of early non-motor features has given rise to the concept of prodromal PD (Berg et al. 2015). The hope is that in the future it will become possible to identify those who are in the preclinical phase of PD, with some α-synuclein inclusions but no symptoms. If so, preventive strategies, when available, could be tried.
References
Abeliovich A, Schmitz Y, Farinas I, Choi-Lundberg D, Ho WH, Castillo PE, Hinsky N, Verdugo JM, Armanini M, Ryan A, Hynes M, Phillips H, Sulzer D, Rosenthal A (2000) Mice lacking α-synuclein display functional deficits in the nigrostriatal dopamine system. Neuron 25:239–252
Aflaki E, Westbroek W, Sidransky E (2017) The complicated relationship between Gaucher disease and parkinsonism: Insights from a rare disease. Neuron 93:737–746
Al-Chalabi A, Dürr A, Wood NW, Parkinson MH, Camuzat A, Hulot JS, Morrison KE, Renton A, Süssmuth SD, Landwehrmeyer BG, Ludolph A, Agid Y, Brice A, Leigh PN, Bensimon G (2009) Genetic variants of the α-synuclein gene SNCA are associated with multiple system atrophy. PLoS ONE 4:e7114
Ansari KA, Johnson AJ (1975) Olfactory function in Parkinson’s disease. J Chronic Dis 28:493–497
Anwar S, Peters O, Millership S, Ninkina NN, Doig N, Connor-Robson N, Threlfell S, Kooner G, Deacon RM, Bannerman DM, Bolam JP, Chandra SS, Cragg SJ, Wade-Martins R, Buchman VL (2011) Functional alterations to the nigrostriatal system in mice lacking all three members of the synuclein family. J Neurosci 31:7264–7274
Appel-Cresswell S, Vilarino-Guell C, Encamacion M, Sherman H, Yu I, Shah B, Weir D, Thompson C, Szu-Tu C, Trinh J, Aaslay JO, Rajput A, Rajput AH, Stoessl JA, Farrer MJ (2013) Alpha-synuclein p.H50Q, a novel pathogenic mutation for Parkinson’s disease. Mov Disord 28:811–813
Arai K, Kato K, Kashiwado K, Hattori T (2000) Pure autonomic failure in association with human α-synucleinopathy. Neurosci Lett 296:171–173
Asi YT, Simpson JE, Heath PR, Wharton SB, Lees AJ, Revesz T, Houlden H, Holton JL (2014) Alpha-synuclein mRNA expression in oligodendrocytes in MSA. Glia 62:964–970
Ayers JI, Brooks MM, Rutherford NJ, Howard JK, Sorrentino ZA, Riffe CJ, Giasson BI (2017) Robust central nervous system pathology in transgenic mice following peripheral injection of α-synuclein fibrils. J Virol 91:e02095–e02016
Beach TG, Adler CH, Sue LI, Peirce JB, Bachalakuri J, Dalsing-Hernandez J, Lue LF, Caviness JN, Connor DJ, Sabbagh MN, Walker DG (2008) Reduced striatal tyrosine hydroxylase in incidental Lewy body disease. Acta Neuropathol 115:445–451
Bendor JT, Logan TP, Edwards RH (2013) The function of α-synuclein. Neuron 79:1044–1066
Berg D, Postuma RB, Adler CH, Bloem BR, Chan P, Dubois B, Gasser T, Goetz CG, Halliday G, Joseph L, Lang AE, Liepelt-Scarfone I, Litvan I, Marek K, Obeso J, Oertel W, Olanow CW, Poewe W, Stern M, Deuschl G (2015) MDS research criteria for prodromal Parkinson’s disease. Mov Disord 30:1600–1609
Bilal-Fares M, Alt-Bouziad N, Dikiy I, Mbefo MK, Jovicic A, Kiely A, Holton JL, Lee SJ, Gitler AD, Eliezer D, Lashuel HA (2014) The novel Parkinson’s disease linked mutation G51D attenuates in vitro aggregation and membrane binding of α-synuclein, and enhances its secretion and nuclear localization in cells. Hum Mol Genet 23:4491–4509
Blocq P, Marinesco G (1893) Sur un cas de tremblement parkinsonien hémiplégique symptomatique d’une tumeur du pédoncule cérébral. CR Soc Biol 5:105–111
Bousset L, Peri L, Ruiz-Arlandis G, Gath J, Jensen PH, Habenstein B, Madiona K, Olieric V, Böckmann A, Meier BH, Melki R (2013) Structural and functional characterization of two α-synuclein strains. Nat Commun 4:2575
Breid S, Bernis ME, Babilla JT, Garza MC, Wille H, Tamgüney G (2016) Neuroinvasion of α-synuclein prionoids after intraperitoneal and intraglossal inoculation. J Virol 90:9182–9193
Brissaud E, Meige H (1895) Leçons sur les maladies nerveuses (Salpêtrière, 1893–1894). Masson Editeur, Paris
Burré J, Sharma M, Südhof TC (2015) Definition of a molecular pathway mediating α-synuclein neurotoxicity. J Neurosci 35:5221–5232
Chandra S, Chen X, Rizo J, Jahn R, Südhof TC (2003) A broken alpha-helix in folded α-synuclein. J Biol Chem 278:15313–15318
Charcot JM (1875) Leçons sur les maladies du système nerveux, vol 1, 2nd edn. Delhaye, Paris
Chartier-Harlin MC, Kachergus J, Roumier C, Mouroux V, Douay X, Lincoln S, Levecque C, Larvor L, Andrieux J, Hulihan M, Waucquier N, Defebre L, Amouyel P, Farrer M, Destée A (2004) α-Synuclein locus duplication as a cause of familial Parkinson’s disease. Lancet 364:1167–1169
Cheng HC, Ulane CM, Burke RE (2010) Clinical progression in Parkinson disease and the neurobiology of axons. Ann Neurol 67:715–725
Choi W, Zibaee S, Jakes R, Serpell LC, Davletov B, Crowther RA, Goedert M (2004) Mutation E46K increases phospholipid binding and assembly into filaments of human α-synuclein. FEBS Lett 576:363–368
Conway KA, Harper JD, Lansbury PT (1998) Accelerated in vitro fibril formation by a mutant α-synuclein linked to early-onset Parkinson disease. Nat Med 4:1318–1320
Cremades N, Cohen SIA, Deas E, Abramov AY, Chen AY, Orte A, Sandal M, Clarke RW, Dunne P, Aprile FA, Bertoncini CW, Wood NW, Knowles TP, Dobson CM, Klenerman D (2012) Direct observation of the interconversion of normal and toxic forms of α-synuclein. Cell 149:1048–1059
Crowther RA, Jakes R, Spillantini MG, Goedert M (1998) Synthetic filaments assembled from C-terminally truncated α-synuclein. FEBS Lett 436:309–312
Crowther RA, Daniel SE, Goedert M (2000) Characterisation of isolated α-synuclein filaments from substantia nigra of Parkinson’s disease brain. Neurosci Lett 292:128–130
Davidson WS, Jonas A, Clayton DF, George JM (1998) Stabilization of α-synuclein secondary structure upon binding to synthetic membranes. J Biol Chem 273:9443–9449
Del Tredici K, Rüb U, De Vos RAI, Bohl JRE, Braak H (2002) Where does Parkinson disease pathology begin in the brain? J Neuropathol Exp Neurol 61:413–426
Deng HX, Shi Y, Yang Y, Ahmeti KB, Miller N, Huang C, Cheng L, Zhai H, Dengt S, Nuytemans K, Corbett NJ, Kim MJ, Deng H, Tang B, Yang Z, Xu Y, Chan P, Hunang B, Gao XP, Song Z, Liu Z, Fecto F, Siddique N, Foroud T, Jankovic J, Ghetti B, Nicholson DA, Krainc D, Melen O, Vance JM, Pericak-Vance MA, Ma YC, Rajput AH, Siddique T (2016) Identification of TMEM230 mutations in familial Parkinson’s disease. Nat Genet 48:733–739
Der-Sarkissian A, Jao CC, Chen J, Langen R (2003) Structural organization of α-synuclein fibril structure studied by site-directed spin labelling. J Biol Chem 278:24970–24979
Dickson D, Fujishiro H, DelleDonne A, Menke J, Ahmed Z, Klos KJ, Josephs KA, Frigerio R, Burnett M, Parisi JE, Ahlskog JE (2008) Evidence that incidental Lewy body disease is pre-symptomatic Parkinson’s disease. Acta Neuropathol 115:437–444
Du HN, Tang L, Luo XY, Li HT, Hu J, Zhou JW, Hu HY (2003) A peptide motif consisting of glycine, alanine, and valine is required for the fibrillization and cytotoxicity of human α-synuclein. Biochemistry 42:8870–8878
Federoff M, Price TR, Sailer A, Scholz S, Hernandez D, Nicolas A, Singleton AB, Nalls M, Houlden H (2016) Genome-wide estimate of the heritability of multiple system atrophy. Parkinsonism Relat Disord 22:35–41
Fujishiro H, Ahn TB, Frigerio R, DelleDonne A, Josephs KA, Parisi JE, Ahlskog EJ, Dickson DW (2008) Glial cytoplasmic inclusions in neurologically normal elderly: prodromal multiple system atrophy? Acta Neuropathol 116:269–275
Garrod A (1928) The lessons of rare maladies. Lancet 211:1055–1060
Ghosh D, Mondal M, Mohite GM, Singh PK, Rankan P, Anoop A, Ghosh S, Jha NN, Kumar A, Maji SK (2013) The Parkinson’s disease-associated H50Q mutation accelerates α-synuclein aggregation in vitro. Biochemistry 52:6925–6927
Ghosh D, Sahay S, Ranjan P, Salot S, Mohite GM, Singh PK, Dwivedi S, Carvalho E, Banerjee R, Kumar A, Maji SK (2014) The newly discovered Parkinson’s disease associated Finnish mutation (A53E) attenuates α-synuclein aggregation and membrane binding. Biochemistry 53:6419–6421
Giasson BI, Murray IV, Trojanowski JQ, Lee VM-Y (2001) A hydrophobic stretch of 12 amino acid residues in the middle of α-synuclein is essential for filament assembly. J Biol Chem 276:2380–2386
Glenner GG, Wong CW (1984) Alzheimer’s disease: Initial report of the purification and characterization of a novel cerebrovascular amyloid protein. Biochem Biophys Res Commun 120:885–890
Goate A, Chartier-Harlin MC, Mullan M, Brown J, Crawford F, Fidani L, Giuffra L, Haynes A, Irving N, James L, Mant R, Newton P, Rooke K, Roques P, Talbot C, Pericak-Vance M, Roses A, Williamson R, Rossor M, Owen M, Hardy J (1991) Segregation of a missense mutation in the amyloid precursor protein gene with familial Alzheimer’s disease. Nature 349:704–706
Goedert M (2001) Alpha-synuclein and neurodegenerative diseases. Nat Rev Neurosci 2:492–501
Goedert M (2015) Alzheimer’s and Parkinson’s diseases: The prion concept in relation to assembled Aβ, tau, and α-synuclein. Science 349:1255555
Goedert M, Spillantini MG (1998) Lewy body diseases and multiple system atrophy as α-synucleinopathies. Mol Psychiatry 3:462–465
Goedert M, Spillantini MG (2012) Synucleinopathies and Tauopathies. In: Brady ST, Siegel GJ, Albers RW, Price DL (eds) Basic Neurochemistry, 8th edn. Elsevier, Cambridge, pp 829–843
Goedert M, Wischik CM, Crowther RA, Walker JE, Klug A (1988) Cloning and sequencing of the cDNA encoding a core protein of the paired helical filament of Alzheimer disease: Identification as the microtubule-associated protein tau. Proc Natl Acad Sci U S A 85:4051–4055
Goedert M, Spillantini MG, Del Tredici K, Braak H (2013) 100 years of Lewy pathology. Nat Rev Neurol 9:13–24
Greffard S, Verny M, Bonnet AM, Seilhean D, Hauw JJ, Duyckaerts C (2010) A stable proportion of Lewy body bearing neurons in the substantia nigra and death suggests a model in which the Lewy body causes neuronal dearth. Neurobiol Aging 31:99–103
Greten-Harrison B, Polydoro M, Morimoto-Tomita M, Diao L, Williams AM, Nie EH, Makani S, Tian N, Castillo PE, Buchman VL, Chandra SS (2010) αβγ-Synuclein triple knockout mice reveal age-dependent neuronal dysfunction. Proc Natl Acad Sci U S A 107:19573–19578
Guo JL, Covell DJ, Daniels JP, Iba M, Stieber A, Zhang B, Riddle DM, Kwong LK, Xu Y, Trojanowski JQ, Lee VM-Y (2013) Distinct α-synuclein strains differentially promote tau inclusions in neurons. Cell 154:103–117
Harvey W, Willis R (1847) The Works of William Harvey. The Sydenham Society, London
Hasegawa M, Fujiwara H, Nonaka T, Wakabayashi K, Takahashi H, Lee VM-Y, Trojanowski JQ, Mann D, Iwatsubo T (2002) Phosphorylated α-synuclein is ubiquitinated in α-synucleinopathy lesions. J Biol Chem 277:49071–49076
Hassler R (1938) Zur Pathologie der Paralysis agitans und des postenzephalitischen Parkinsonismus. J Psychol Neurol 24:387–455
Hutton M, Lendon CL, Rizzu P, Baker M, Froelich S, Houlden H, Pickering-Brown S, Chakraverty S, Isaacs A, Grover A, Hackett J, Adamson J, Lincoln S, Dickson D, Davies P, Petersen RC, Stevens M, de Graaff E, Wauters E, van Baren J, Hillebrand M, Joosse M, Kwon JM, Nowotny P, Che LK, Norton J, Morris JC, Reed LA, Trojanoewski JQ, Basun H, Lannfelt L, Neystat M, Fahn S, Dark F, Tannenberg T, Dodd PR, Hayward N, Kwok JBJ, Schofield PR, Andreadis A, Snowden J, Craufurd D, Neary D, Owen F, Oostra BA, Hardy J, Goate A, van Swieten J, Mann D, Lynch T, Heutink P (1998) Association of missense and 5′-splice site mutations in tau with the inherited dementia FTDP-17. Nature 393:702–705
Ibánez P, Bonnet AM, Débarges B, Lohmann E, Tison F, Pollak P, Agid Y, Dürr A, Brice A (2004) Causal relation between α-synuclein gene duplication and familial Parkinson’s disease. Lancet 364:1169–1171
Ikeuchi T, Kakita A, Shiga A, Kasuga K, Kaneko H, Tan CF, Idezuka J, Wakabayashi K, Onodera O, Iwatsubo T, Nishizawa M, Takahashi H, Ishikawa A (2008) Patients homozygous and heterozygous for SNCA duplication in a family with parkinsonism and dementia. Arch Neurol 65:514–519
Iljina M, Tosatto L, Choi ML, Sang JC, Ye Y, Hughes CD, Bryant CE, Gandhi S, Klenerman D (2016) Arachidonic acid mediates the formation of abundant helical multimers of α-synuclein. Sci Rep 6:33928
Iwanaga K, Wakabayashi K, Yoshimoto M, Tomita I, Satoh H, Takashima H, Satoh A, Tsujihata M, Takahashi H (1999) Lewy body-type degeneration in cardiac plexus in Parkinson’s and incidental Lewy body diseases. Neurology 52:1269–1271
Jakes R, Spillantini MG, Goedert M (1994) Identification of two distinct synucleins from human brain. FEBS Lett 345:27–32
Jao CC, Hegde BG, Chen J, Haworth IS, Langen R (2008) Structure of membrane-bound α-synuclein from site-directed spin labelling and computational refinement. Proc Natl Acad Sci U S A 105:19666–19671
Jenner P, Morris HR, Robbins TW, Goedert M, Hardy J, Ben-Shlomo Y, Bolam P, Burn D, Hindle JV, Brooks D (2013) Parkinson’s disease – the debate on the clinical phenomenology, aetiology, pathology and pathogenesis. J Parkinson’s Dis 3:1–11
Jensen PH, Nielsen MS, Jakes R, Dotti CG, Goedert M (1998) Binding of α-synuclein to brain vesicles is abolished by familial Parkinson’s disease mutation. J Biol Chem 273:26292–26294
Kamp F, Exner N, Lutz AK, Wender N, Hegermann J, Brunner B, Nuscher B, Bartels T, Giese A, Beyer K, Eimer S, Winklhofer KF, Haass C (2010) Inhibition of mitochondrial fusion by α-synuclein is rescued by PINK1, Parkin and DJ-1. EMBO J 29:3571–3589
Kaufmann H, Nahm K, Purohit D, Wolfe D (2004) Autonomic failure as the initial presentation of Parkinson disease and dementia with Lewy bodies. Neurology 63:1093–1095
Kiely AP, Asi YT, Kara E, Limousin P, Ling H, Lewis P, Proukakis C, Quinn N, Lees AJ, Hardy J, Revesz T, Houlden H, Holton JL (2013) α-Synucleinopathy associated with G51D SNCA mutation: A link between Parkinson’s disease and multiple system atrophy? Acta Neuropathol 125:753–7690
Kisos H, Pukass K, Ben-Hur T, Richter-Landsberg C, Sharon R (2012) Increased neuronal α-synuclein pathology associates with its accumulation in oligodendrocytes in mice modelling α-synucleinopathies. PLoS ONE 7:e46817
Kordower JH, Chu Y, Hauser RA, Freeman TB, Olanow CW (2008) Lewy body-like pathology in long-term embryonic neural transplants in Parkinson’s disease. Nat Med 14:506–508
Krüger R, Kuhn W, Müller T, Woitalla D, Graeber M, Kösel S, Przuntek H, Epplen JT, Schöls L, Riess O (1998) Ala30Pro mutation in the gene encoding α-synuclein in Parkinson’s disease. Nat Genet 18:106–108
Lesage S, Anheim M, Letournel F, Bousset L, Honoré A, Rozas N, Pieri L, Madiona K, Dürr A, Melki R, Verny C, Brice A (2013) G51D α-synuclein mutation causes a novel parkinsonian-pyramidal syndrome. Ann Neurol 73:459–471
Lewy F (1912) Paralysis agitans. I. Pathologische Anatomie. In: Lewandowsky M, Abelsdorff G (eds) Handbuch der Neurologie, vol 3. Springer, Berlin, pp 920–933
Li J, Englund E, Holton JL, Soulet D, Hagell P, Lees AJ, Lashley T, Quinn NP, Rehncrona S, Björklund A, Widner H, Revesz T, Lindvall O, Brundin H (2008) Lewy bodies in grafted neurons in subjects with Parkinson’s disease suggest host-to-graft propagation. Nat Med 14:501–503
Li W, Englund E, Widner H, Mattson B, van Westen D, Lätt J, Rehncrona S, Brundin P, Björklund A, Lindvall O, Li JY (2016) Extensive graft-derived dopaminergic innervation is maintained 24 years after transplantation in the degenerating parkinsonian brain. Proc Natl Acad Sci U S A 113:6544–6549
Logan T, Bendor J, Toupin C, Thorn K, Edwards RH (2017) α-Synuclein promotes dilation of the exocytotic fusion pore. Nat Neurosci 20:681–689
Martikainen M, Päivärinta M, Hietala M, Kaasinen V (2015) Clinical and imaging findings in Parkinson disease associated with the A53E SNCA mutation. Neurol Genet 1:e27
Mazzulli JR, Xu YH, Sun Y, Knight AL, McLean PJ, Caldwell GA, Sidransky E, Grabowski GA, Krainc D (2011) Gaucher disease glucocerebrosidase and α-synuclein form a bidirectional pathogenic loop in synucleinopathies. Cell 146:37–52
Miake H, Mizusawa H, Iwatsubo T, Hasegawa M (2002) Biochemical characterization of the core structure of α-synuclein filaments. J Biol Chem 277:19213–19219
Mitsui J, Matsukawa T, Sasaki H, Yabe I, Matsushima M, Dürr A, Brice A, Takashima H, Kikuchi A, Aoki M, Ishiura H, Yasuda T, Date H, Ahsan B, Iwata A, Goto J, Ichikawa Y, Nakahara Y, Momose Y, Takahashi Y, Hara K, Kakita A, Yamada M, Takahashi H, Onodera O, Nishizawa M, Watanabe H, Ito M, Sobue G, Ishikawa K, Mizusawa H, Kanai K, Hattori T, Kuwabara S, Arai K, Koyano S, Kuroiwa Y, Hasegawa K, Yuasa T, Yasui K, Nakashima K, Ito H, Izumi Y, Kaji R, Kato T, Kusunoki S, Osaki Y, Horiuchi M, Kondo T, Murayama S, Hattori N, Yamamoto M, Murata M, Satake W, Toda T, Filla A, Klockgether T, Wüllner U, Nicholson G, Gilman S, Tanner CM, Kukull WA, Stern MB, Lee VM-Y, Trojanowski JQ, Masliah E, Low PA, Sandroni P, Ozelius LJ, Foroud T, Tsuji S (2015) Variants associated with Gaucher disease in multiple system atrophy. Ann Clin Transl Neurol 2:417–426
Nakamura K, Nemani VM, Azerbal F, Skibinski G, Levy JM, Egami K, Munishkina L, Zhang J, Gardner B, Wakabayashi J, Sesaki H, Cheng Y, Finkbeiner S, Nussbaum RL, Masliah E, Edwards RH (2011) Direct membrane association drives mitochondrial fission by the Parkinson disease-associated protein α-synuclein. J Biol Chem 286:20710–20726
Nalls MA, Pankratz N, Lill CM, Do CB, Hernandez DG, Saad M, DeStefano AL, Kara E, Bras J, Sharma M, Schulte C, Keller MF, Arepalli S, Letson C, Edsall C, Stefansson H, Liu X, Pliner H, Lee JH, Cheng R, Ikram MA, Ioannidis JP, Hadjigeorgiou GM, Bis JC, Martinez M, Perlmutter JS, Goate A, Marder K, Fiske B, Sutherland M, Xiromerisiou G, Myers RH, Clark LN, Stefansson K, Hardy JA, Heutink P, Chen H, Wood NW, Houlden H, Payami H, Brice A, Scott WK, Gasser T, Bertram L, Eriksson N, Foroud T, Singleton AB (2014) Large-scale meta-analysis of genome-wide association data identifies six new risk loci for Parkinson’s disease. Nat Genet 46:989–993
Narhi L, Wood SJ, Steavenson S, Jiang Y, Wu GM, Anafi D, Kaufman SA, Martin F, Sitney K, Denis P, Louis JC, Wypych J, Biere AL, Citron M (1999) Both familial Parkinson’s disease mutations accelerate α-synuclein aggregation. J Biol Chem 274:9843–9846
Neudorfer O, Giladi N, Elstein D, Abrahamov A, Turezkite T, Aghai E, Reches A, Bembi B, Zimran A (1996) Occurrence of Parkinson’s syndrome in type I Gaucher disease. Q J Med 89:691–694
Osterberg VR, Spinelli KJ, Weston LJ, Luk KC, Woltjer RL, Unni VK (2015) Progressive aggregation of α-synuclein and selective degeneration of Lewy inclusion-bearing neurons in a mouse model of parkinsonism. Cell Rep 10:1252–1260
Paisán-Ruiz C, Jain S, Evans EW, Gilks WP, Simón J, van der Brug M, López de Munain A, Aparicio S, Gil AM, Khan N, Johnson J, Martinez JR, Nicholl D, Carrera IM, Pena AS, de Silva R, Lees A, Marti-Massó JF, Pérez-Tur J, Wood NW, Singleton AB (2004) Cloning of the gene containing mutations that cause PARK8-linked Parkinson’s disease. Neuron 18:595–600
Papp MI, Kahn JE, Lantos PL (1989) Glial cytoplasmic inclusions in the CNS of patients with multiple system atrophy (striatonigral degeneration, olivopontocerebellar atrophy and Shy-Drager syndrome). J Neurol Sci 94:79–100
Parkinson J (1817) An Essay on the Shaking Palsy. Sherwood, Neely and Jones, London
Parkkinen L, Hartikainen P, Alazuloff I (2007) Abundant glial α-synuclein pathology in a case without overt clinical symptoms. Clin Neuropathol 26:276–283
Pasanen P, Myllykangas L, Siitonen M, Raunio A, Kaakola S, Lyytinen J, Tienari PJ, Pöyhönen M, Paetau A (2014) A novel α-synuclein mutation A53E associated with atypical multiple system atrophy and Parkinson’s disease-type pathology. Neurobiol Aging 25:2180.e1–2180.e5
Peelaerts W, Bousset L, van der Perren A, Moskalyuk A, Pulizzi R, Giugliano M, van den Haute C, Melki R, Baekelandt V (2015) α-Synuclein strains cause distinct synucleinopathies after local and systemic administration. Nature 522:340–344
Pollock NJ, Mirra SS, Binder LI, Hansen LA, Wood JG (1986) Filamentous aggregates in Pick’s disease, progressive supranuclear palsy, and Alzheimer’s disease share antigenic determinants with microtubule-associated protein tau. Lancet II:1211
Polymeropoulos MH, Lavedan C, Lertoy R, Ide SE, Dehejia S, Dutra A, Pike B, Root H, Rubenstein J, Boyer R, Stenroos ES, Chandrasekharappa S, Athanassiadou A, Papapetropoulos T, Johnson WG, Lazzarini AM, Duvoisin RC, Di Iorio G, Golbe LI, Nussbaum RL (1997) Mutation in the α-synuclein gene identified in families with Parkinson’s disease. Science 276:2045–2047
Poorkaj P, Bird TD, Wijsman E, Nemens E, Garruto RM, Anderson L, Andreadis A, Wiederholt WC, Raskind M, Schellenberg GD (1998) Tau is a candidate gene for chromosome 17 frontotemporal dementia. Ann Neurol 43:815–825
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, Obeso J, Marek K, Litvan I, Lang AE, Halliday G, Goetz CG, Gasser T, Dubois B, Chan P, Bloem BR, Adler CH, Deuschl G (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30:1591–1599
Proukakis C, Dudzik CG, Brier T, MacKay DS, Cooper JM, Millhauser GL, Houlden H, Schapira AH (2013) A novel α-synuclein missense mutation in Parkinson disease. Neurology 80:1062–1064
Prusiner SB, Woerman AL, Mordes DA, Watts JC, Rampersaud R, Berry DB, Patel S, Oehler A, Lowe JK, Kravitz SN, Geschwind DH, Glidden DV, Halliday GM, Middleton LT, Gentleman SM, Grinberg LT, Giles K (2015) Evidence for α-synuclein prions causing multiple system atrophy in humans with parkinsonism. Proc Natl Acad Sci U S A 112:E5308–E5317
Reyes JF, Rey NL, Bousset L, Melki R, Brundin P, Angot E (2014) Alpha-synuclein transfers from neurons to oligodendrocytes. Glia 62:387–398
Rodriguez JA, Ivanova MI, Sawaya MR, Cascio D, Reyes FE, Shi D, Sangwan S, Guenther EL, Johnson LM, Zhang M, Jiang L, Arbing MA, Nannenga BL, Hattne J, Whitelegge J, Brewater AS, Messerschmidt M, Boutet S, Sauter NK, Gonen T, Eisenberg DS (2015) Structure of the toxic core of α-synuclein from invisible crystals. Nature 525:486–490
Rutherford NJ, Moore BD, Golde TE, Giasson BI (2014) Divergent effects of the H50Q and G51D SNCA mutations on the aggregation of α-synuclein. J Neurochem 131:859–867
Sailer A, Scholz SW, Nalls MA, Schulte C, Federoff M, Price TR, Lees A, Ross OA, Dickson DW, Mok K, Mencacci NE, Schottlaender L, Chelban V, Ling H, O’Sullivan SS, Wood NW, Traynor BJ, Ferrucci L, Federoff HJ, Mhyre TR, Morris HR, Deuschl G, Quinn N, Widner H, Albanese A, Infante J, Bhatia KP, Poewe W, Oertel W, Höglinger GU, Wüllner U, Goldwurm S, Pellecchia MT, Ferreira J, Tolosa E, Bloem BR, Rascol O, Meissner WG, Hardy JA, Revesz T, Holton JL, Gasser T, Wenning GK, Singleton AB, Houlden H (2016) A genome-wide association study in multiple system atrophy. Neurology 87:12591–11598
Sampathu DM, Giasson BI, Pawlyk AC, Trojanowski JQ, Lee VM-Y (2003) Ubiquitination of α-synuclein is not required for formation of pathological inclusions in α-synucleinopathies. Am J Pathol 163:91–100
Sanders WR (1865) Case of an unusual form of nervous disease, dystaxia or pseudo-paralysis agitans, with remarks. Edinb Med J 10:987–997
Satake W, Nakabayashi Y, Mizuta I, Hirota Y, Ito C, Kubo M, Kawaguchi T, Tsunoda T, Watanabe M, Takeda A, Tomiyama H, Nakashima K, Hasegawa K, Obata F, Yoshikawa T, Kawakami H, Sakoda S, Yamamoto M, Hattori N, Murata M, Nakamura Y, Toda T (2009) Genome-wide association study identifies common variants at four loci as genetic risk factors for Parkinson’s disease. Nat Genet 41:1303–1307
Schapira AH, Tolosa E (2010) Molecular and clinical prodrome of Parkinson disease: implications for treatment. Nat Rev Neurol 6:309–317
Schenck CH, Bundle SR, Ettinger MG, Mahowald MW (1986) Chronic behavioural disorders of human REM sleep: a new category of parasomnia. Sleep 9:293–308
Scholz SW, Houlden H, Schulte C, Sharma M, Li AS, Berg D, Melchers A, Paudel R, Gibbs JR, Simón-Sánchez J, Paisan-Ruiz C, Braas J, Ding J, Chen H, Traynor BJ, Arepalli S, Zonozi RR, Revesz T, Holton J, Wood N, Lees A, Oertel W, Wüllner U, Goldwurm S, Pellecchia MT, Illig T, Riess O, Fernandez HH, Rodriguez RL, Okun MS, Poese W, Wenning KK, Hardy JA, Singleton AB, Del Sorbo F, Schneider S, Bhatia KP, Gasser T (2009) SNCA variants are associated with increased risk for multiple system atrophy. Ann Neurol 65:610–614
Serpell LC, Berriman J, Jakes R, Goedert M, Crowther RA (2000) Fiber diffraction of synthetic α-synuclein filaments shows amyloid-like cross-β conformation. Proc Natl Acad Sci U S A 97:4897–4502
Shimozawa A, Ono M, Takahara D, Tarutani A, Imura S, Masuda-Suzukake M, Higuchi M, Yanai K, Hisanaga S, Hasegawa M (2017) Propagation of pathological α-synuclein in marmoset brain. Acta Neuropathol Commun 5:12
Simón-Sánchez J, Schulte C, Bras JM, Sharma M, Gibbs JR, Berg D, Paisan-Ruiz C, Lichtner P, Scholz SW, Hernandez DG, Krüger R, Federoff M, Klein C, Goate A, Perlmutter J, Bonin M, Nalls MA, Illig T, Gieger C, Houlden H, Steffens M, Okun MS, Racette BA, Cookson MER, Foote KD, Fernandez HH, Traynor BJ, Schreiber S, Arepalli S, Zonozi R, Gwinn K, van der Brug M, Lopez G, Chanock SJ, Schatzkin A, Park Y, Hollenbeck A, Gao J, Huang X, Wood NW, Lorenz D, Deuschl G, Chen H, Riess O, Hardy J, Singleton AB, Gasser T (2009) Genome-wide association study reveals genetic risk underlying Parkinson’s disease. Nat Genet 41:1308–1312
Singleton AB, Farrer M, Johnson J, Singleton A, Hague S, Kachergus J, Hulihan M, Peuralinna T, Dutra A, Nussbaum R, Lincoln S, Crawley A, Hanson M, Maraganore D, Adler C, Cookson MR, Muenter M, Baptista M, Miller D, Blancato J, Hardy G, Gwinn-Hardy K (2003) α-Synuclein locus triplication causes Parkinson’s disease. Science 302:841
Spillantini MG, Schmidt ML, Lee VM-Y, Trojanowski JQ, Jakes R, Goedert M (1997) α-Synuclein in Lewy bodies. Nature 388:839–840
Spillantini MG, Murrell JR, Goedert M, Farlow MR, Klug A, Ghetti B (1998a) Mutation in the tau gene in familial multiple system tauopathy with presenile dementia. Proc Natl Acad Sci U S A 95:7737–7741
Spillantini MG, Crowther RA, Jakes R, Hasegawa M, Goedert M (1998b) α-Synuclein in filamentous inclusions of Parkinson’s disease and dementia with Lewy bodies. Proc Natl Acad Sci U S A 95:6469–6473
Spillantini MG, Crowther RA, Jakes R, Cairns NJ, Lantos PL, Goedert M (1998c) Filamentous α-synuclein inclusions link multiple system atrophy with Parkinson’s disease and dementia with Lewy bodies. Neurosci Lett 251:205–208
Steger M, Tonelli F, Ito G, Davies P, Trost M, Vetter M, Wachter S, Lorentzen E, Duddy G, Wilson S, Baptista MAS, Fiske BF, Fell MJ, Morrow JA, Reith AD, Alessi DR, Mann M (2016) Phosphoproteomics reveals that Parkinson’s disease kinase LRRK2 regulates a subset of Rab GTPases. eLife 5:e12813
Trétiakoff C (1919) Contribution à l’étude de l’anatomie pathologique du locus niger de Soemmering avec quelques déductions relatives à la pathogénie des troubles du tonus musculaire et de la maladie de Parkinson. Jouve, Paris
Tu P, Galvin JE, Baba M, Giasson B, Tomita T, Leight S, Nakajo S, Iwatsubo T, Trojanowski JQ, Lee VM-Y (1998) Glial cytoplasmic inclusions in white matter oligodendrocytes of multiple system atrophy brain contain insoluble α-synuclein. Ann Neurol 44:415–422
Tuttle MD, Comellas G, Nieuwkoop AJ, Covell DJ, Berthold DA, Kloepper KD, Courtney JM, Kim JK, Barclay AM, Kendall A, Wan W, Stubbs G, Schwieters CD, Lee VM-Y, George JM, Rienstra CM (2016) Solid-state NMR structure of a pathogenic fibril of full-length human α-synuclein. Nat Struct Mol Biol 23:409–415
Uchihara T, Nakamura A, Mochizuki Y, Hayashi M, Orimo S, Isozaki E, Mizutani T (2005a) Silver stainings distinguish Lewy bodies and glial cytoplasmic inclusions: Comparison between Gallyas-Braak and Campbell-Switzer methods. Acta Neuropathol 110:255–260
Uchihara T, Tsuchiya K, Nakamura A, Akiyama H (2005b) Argyrophilic grains are not always argyrophilic – distinction from neurofibrillary tangles of diffuse neurofibrillary tangles with calcification revealed by comparison between Gallyas and Campbell-Switzer methods. Acta Neuropathol 110:158–164
Ulmer TS, Bax A, Cole NB, Nussbaum RL (2005) Structure and dynamics of micelle-bound human α-synuclein. J Biol Chem 280:9595–9603
Vilarino-Güell C, Soto-Ortolaza AI, Rajput A, Mash DC, Papapetropoulos S, Pahwa R, Lyons KE, Uitti RJ, Wszolek ZK, Dickson DW, Farrer MJ, Ross OA (2011) MAPT H1 haplotype is a risk factor for essential tremor and multiple system atrophy. Neurology 76:670–672
Wakabayashi K, Yoshimoto M, Tsuji S, Takahashi H (1998) α-Synuclein immunoreactivity in glial cytoplasmic inclusions in multiple system atrophy. Neurosci Lett 249:180–182
Wilhelm BG, Mandad S, Truckenbrodt S, Kröhnert K, Schäfer C, Rammner B, Koo SJ, Classen GA, Krauss M, Haucke V, Urlaub H, Rizzoli SO (2014) Composition of isolated synaptic boutons reveals the amounts of vesicle trafficking proteins. Science 344:1023–1028
Wischik CM, Novak M, Thøgersen HC, Edwards PC, Runswick MJ, Jakes R, Walker JE, Milstein C, Roth M, Klug A (1988a) Isolation of a fragment of tau derived from the core of the paired helical filament of Alzheimer disease. Proc Natl Acad Sci U S A 85:4506–4510
Wischik CM, Novak M, Edwards PC, Klug A, Tichelaar W, Crowther RA (1988b) Structural characterization of the core of the paired helical filament of Alzheimer disease. Proc Natl Acad Sci U S A 85:4884–4888
Woerman AL, Stöhr J, Aoyagi A, Rampersaud R, Krejciova Z, Watts JC, Ohyama T, Patel S, Widjaja K, Oehler A, Sanders DW, Diamond MI, Seeley WW, Middleton LT, Gentleman SM, Mordes DA, Südhof TC, Giles K, Prusiner SB (2015) Propagation of prions causing synucleinopathies in cultured cells. Proc Natl Acad Sci U S A 112:E4949–E4958
Yap TL, Gruschus JM, Vewlayati A, Westbroek W, Goldin E, Moaven N, Sidransky E, Lee JC (2011) α-Synuclein interacts with glucocerebrosidase providing a molecular link between Parkinson and Gaucher diseases. J Biol Chem 286:28080–28088
Yoshino H, Hirano M, Stoessl AJ, Imamichi Y, Ikeda A, Li Y, Funayama M, Yamada I, Nakamura Y, Sossi V, Farrer MJ, Nishioka K, Hattori N (2017) Homozygous alpha-synuclein p.A53V in familial Parkinson’s disease. Neurobiol Aging 57:248e7–248e12
Ysselstein D, Joshi M, Mishra V, Griggs AM, Asaiago JM, McCabe GP, Stanciu LA, Post CB, Rochet JC (2015) Effects of impaired membrane interactions on α-synuclein aggregation and neurotoxicity. Neurobiol Dis 79:150–163
Zarranz JJ, Alegre J, Gómez-Esteban JC, Lezcano E, Ros R, Ampuero I, Vidal L, Hoenicka J, Rodriguez O, Atarés B, Llorens V, Gomez-Tortosa E, del Ser T, Munoz DG, de Yebenes JG (2003) The new mutation, E46K, of α-synuclein causes Parkinson and Lewy body dementia. Ann Neurol 55:164–173
Zimprich A, Biskup S, Leitner P, Lichtner P, Farrer M, Lincoln S, Kachergus J, Hulihan M, Uitti RJ, Calne DB, Stoessl AJ, Pfeiffer RF, Patenge N, Carbajal IC, Vieregge P, Asmus F, Müler-Myhsok B, Dickson DW, Meitinger T, Strom TM, Wszolek ZK, Gasser T (2004) Mutations in LRRK2 cause autosomal-dominant parkinsonism with pleomorphic pathology. Neuron 18:601–607
Acknowledgements
MGS is supported by the UK Medical Research Council, Alzheimer’s Research UK, Gates International, Astra Zeneca, Cambridge Biomedical Centre, Addenbrooke’s Hospital Trust, the National Centre for the Replacement, Refinement and Reduction of Animals in Research and Horizon 2020 IMPRiND. MG is an Honorary Professor in the Department of Clinical Neurosciences of the University of Cambridge. He is supported by the UK Medical Research Council (MC_U105184291), the EU Joint Programme – Neurodegenerative Disease Research and Horizon 2020 IMPRiND.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Spillantini, M.G., Goedert, M. Neurodegeneration and the ordered assembly of α-synuclein. Cell Tissue Res 373, 137–148 (2018). https://doi.org/10.1007/s00441-017-2706-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-017-2706-9