Abstract
The banking of testicular tissue before highly gonadotoxic treatment is a prerequisite for the preservation of fertility in pre-pubertal boys not yet producing sperm. The aim of the current study is to evaluate the impact of a soaking temperature performed at −7 °C, −8 °C or −9 °C on the ability of frozen-thawed mouse spermatogonial stem cells (SSCs) to generate haploid germ cells after in vitro maturation. Testes of 6.5-day-old post-partum CD-1 mice were cryopreserved by using a controlled slow freezing protocol with soaking at −7 °C, −8 °C or −9 °C. Frozen-thawed pre-pubertal testicular tissues were cultured in vitro on agarose gel for 30 days. Histological evaluations were performed and flagellated late spermatids were counted after mechanical dissection of the cultured tissues. The differentiation of frozen SSCs into elongated spermatids was more efficient after treatment at −9 °C than at −7 °C and −8 °C. After dissection, flagellated late spermatids were observed by using Shorr staining. The number of flagellated late spermatids was significantly decreased after slow freezing when compared with a fresh tissue control. Therefore, the soaking temperature during slow freezing of pre-pubertal mouse testicular tissue might positively influence the course of in vitro spermatogenesis. Our slow freezing protocol with a soaking temperature at −9 °C was the optimal condition in terms of the achievement of in vitro spermatogenesis with a higher production of elongated spermatids, although the effectiveness of the maturation process was reduced compared with the fresh tissue control.






Similar content being viewed by others
References
Abney TO, Meyers RB (1987) The effects of low O2 and antioxidants on steroidogenic capacity in cultured rat Leydig cells. Adv Exp Med Biol 219:609–612
Arkoun B, Dumont L, Milazzo J-P, Way A, Bironneau A, Wils J, Macé B, Rives N (2015) Retinol improves in vitro differentiation of prepubertal mouse spermatogonial stem cells into sperm during the first wave of spermatogenesis. PLoS One 10:e0116660
Arregui L, Dobrinski I (2014) Xenografting of testicular tissue pieces: 12 years of an in vivo spermatogenesis system. Reproduction 148:R71–R84
Baert Y, Van Sean D, Haentjens P, In’t Veld P, Tournaye H, Goosses E (2013) What is the best protocol for human testicular tissue banking? Hum Reprod 28:1816–1826
Chen GR, Ge RS, Lin H, Dong L, Sottas CM, Hardy MP (2007) Development of a cryopreservation protocol for Leydig cells. Hum Reprod 22:2160–2168
Curaba M, Verleysen M, Amorim CA, Dolmans MM, Van Langendonckt A, Hovatta O, Wyns C, Donnez J (2011) Cryopreservation of pre-pubertal mouse testicular tissue by vitrification. Fertil Steril 95:1229–1234.e1
Dumont L, Arkoun B, Jumeau F, Milazzo JP, Bironneau A, Liot D, Wils J, Rondanino C, Rives N (2015) Assessment of the optimal vitrification protocol for pre-pubertal mice testes leading to successful in vitro production of flagellated spermatozoa. Andrology 3:611–625
Fishman JA, Scobie L, Takeuchi Y (2012) Xenotransplantation-associated infectious risk: a WHO consultation. Xenotransplantation 19:72–81
Garcia-Gonzalo FR, Izpisúa Belmonte JC (2008) Albumin-associated lipids regulate human embryonic stem cell self-renewal. PLoS One 3:e1384
Goossens E, Frederickx V, Geens M, De Block G, Tournaye H (2008) Cryosurvival and spermatogenesis after allografting prepubertal mouse tissue: comparison of two cryopreservation protocols. Fertil Steril 89:725–727
Goossens E, Van Saen D, Tournaye H (2013) Spermatogonial stem cell preservation and transplantation: from research to clinic. Hum Reprod 28:897–907
Honaramooz A, Snedaker A, Boiani M, Schöler H, Dobrinski I, Schlatt S (2002) Sperm from neonatal mammalian testes grafted in mice. Nature 418:778–781
Hou M, Andersson M, Eksborg S, Söder O, Jahnukainen K (2007) Xenotransplantation of testicular tissue into nude mice can be used for detecting leukemic cell contamination. Hum Reprod 22:1899–1906
Jahnukainen K, Ehmcke J, Hergenrother SD, Schlatt S (2007) Effect of cold storage and cryopreservation of immature non-human primate testicular tissue on spermatogonial stem cell potential in xenografts. Hum Reprod 22:1060–1067
Jezek D, Schulze W, Kalanj-Bognar S, Vukelić Z, Milavec-Puretić V, Krhen I (2001) Effects of various cryopreservation media and freezing-thawing on the morphology of rat testicular biopsies. Andrologia 33:368–378
Keros V, Rosenlund B, Hultenby K, Aghajanova L, Levkov L, Hovatta O (2005) Optimizing cryopreservation of human testicular tissue: comparison of protocols with glycerol, propanediol and dimethylsulphoxide as cryoprotectants. Hum Reprod 20:1676–1687
Keros V, Hultenby K, Borgström B, Fridström M, Jahnukainen K, Hovatta O (2007) Methods of cryopreservation of testicular tissue with viable spermatogonia in pre-pubertal boys undergoing gonadotoxic cancer treatment. Hum Reprod 22:1384–1395
Kvist K, Thorup J, Byskov AG, Høyer PE, Møllgård K, Yding Andersen C (2006) Cryopreservation of intact testicular tissue from boys with cryptorchidism. Hum Reprod 21:484–491
Lee YA, Kim YH, Ha SJ, Kim KJ, Kim BJ, Kim BG, Choi SH, Kim IC, Schmidt JA, Ryu BY (2014) Cryopreservation of porcine spermatogonial stem cells by slow-freezing testis tissue in trehalose. J Anim Sci 92:984–995
Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, Quinn G, Wallace WH, Oktay K (2013) Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 31:2500–2510
Luetjens CM, Stukenborg JB, Nieschlag E, Simoni M, Wistuba J (2008) Complete spermatogenesis in orthotopic but not in ectopic transplants of autologously grafted marmoset testicular tissue. Endocrinology 149:1736–1747
Mazur P (1977) The role of intracellular freezing in the death of cells cooled at supraoptimal rates. Cryobiology 14:251–272
Milazzo JP, Vaudreuil L, Cauliez B, Gruel E, Massé L, Mousset-Siméon N, Macé B, Rives N (2008) Comparison of conditions for cryopreservation of testicular tissue from immature mice. Hum Reprod 23:17–28
Milazzo JP, Travers A, Bironneau A, Safsaf A, Gruel E, Arnoult C, Macé B, Boyer O, Rives N (2010) Rapid screening of cryopreservation protocols for murine pre-pubertal testicular tissue by histology and PCNA immunostaining. J Androl 31:617–630
Ogawa T, Ohmura M, Ohbo K (2005) The niche for spermatogonial stem cells in the mammalian testis. Int J Hematol 2:381–388
Pacchiarotti J, Ramos T, Howerton K, Greilach S, Zaragoza K, Olmstead M, Izadyar F (2013) Developing a clinical-grade cryopreservation protocol for human testicular tissue and cells. Biomed Res Int 2013:930–962
Perdrix A, Macé B, Milazzo JP, Liard-Zmuda A, Baron M, Rives N (2010) Ovarian tissue thawing: a comparison of two conditions. Fertil Steril 93:307–310
Poirot C, Vacher-Lavenu MC, Helardot P, Guibert J, Brugières L, Jouannet P (2002) Human ovarian tissue cryopreservation: indications and feasibility. Hum Reprod 17:1447–1452
Reuter K, Schlatt S, Ehmcke J, Wistuba J (2012) Fact or fiction: in vitro spermatogenesis. Spermatogenesis 2:245–252
Schlatt S, Kim SS, Gosden R (2002) Spermatogenesis and steroidogenesis in mouse, hamster and monkey testicular tissue after cryopreservation and heterotopic grafting to castrated hosts. Reproduction 124:339–346
Shaw JM, Jones GM (2003) Terminology associated with vitrification and other cryopreservation procedures for oocytes and embryos. Hum Reprod Update 9:583–605
Shinohara T, Inoue K, Ogonuki N, Kanatsu-Shinohara M, Miki H, Nakata K, Kurome M, Nagashima H, Toyokuni S, Kogishi K, Honjo T, Ogura A (2002) Birth of offspring following transplantation of cryopreserved immature testicular pieces and in-vitro microinsemination. Hum Reprod 17:3039–3045
Song Y, Silversides FG (2007) Production of offspring from cryopreserved chicken testicular tissue. Poult Sci 86:1390–1396
Song HW, Wilkinson MF (2012) In vitro spermatogenesis: a long journey to get tails. Spermatogenesis 2:238–244
Travers A, Arkoun B, Safsaf A, Milazzo JP, Absyte A, Bironneau A, Perdrix A, Sibert L, Macé B, Cauliez B, Rives N (2013) Effects of vitamin A on in vitro maturation of pre-pubertal mouse spermatogonial stem cells. PLoS One 8:e82819
Unni S, Kasiviswanathan S, D’Souza S, Khavale S, Mukherjee S, Patwardhan S, Bhartiya D (2012) Efficient cryopreservation of testicular tissue: effect of age, sample state, and concentration of cryoprotectant. Fertil Steril 97:200–208
Woods EJ, Benson JD, Agca Y, Critser JK (2004) Fundamental cryobiology of reproductive cells and tissues. Cryobiology 48:146–156
Wyns C, Van Langendonckt A, Wese FX, Donnez J, Curaba M (2008) Long-term spermatogonial survival in cryopreserved and xenografted immature human testicular tissue. Hum Reprod 23:2402–2414
Wyns C, Curaba M, Vanabelle B, Van Langendonckt A, Donnez J (2010) Options for fertility preservation in pre-pubertal boys. Hum Reprod Update 16:312–328
Wyns C, Curaba M, Petit S, Vanabelle B, Laurent P, Wese JF, Donnez J (2011) Management of fertility preservation in pre-pubertal patients: 5 years’ experience at the Catholic University of Louvain. Hum Reprod 26:737–747
Yildiz C, Mullen B, Jarvi K, McKerlie C, Lo KC (2013) Effect of different cryoprotectant agents on spermatogenesis efficiency in cryopreserved and grafted neonatal mouse testicular tissue. Cryobiology 67:70–75
Yokonishi T, Sato T, Komeya M, Katagiri K, Kubota Y, Nakabayashi K, Hata K, Inoue K, Ogonuki N, Ogura A, Ogawa T (2014) Offspring production with sperm grown in vitro from cryopreserved testis tissues. Nat Commun 5:4320
Acknowledgments
The authors are grateful to Agathe Way for her assistance with the immunohistochemistry.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare no competing interests.
Additional information
This study was supported by a PhD grant from ”La Région Haute-Normandie” (awarded to Brahim Arkoun) and funding from Rouen University Hospital, Institute for Research and Innovation in Biomedicine, Agence de la Biomédecine and “la Ligue nationale contre le cancer”.
Electronic supplementary material
Below is the link to the electronic supplementary material.
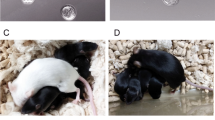
Fig. S1
Representation of experimental procedures performed with pre-pubertal (6.5 dpp) mouse testes. a Controlled slow freezing of pre-pubertal mouse testes with various soaking temperatures (−7 °C, −8 °C or −9 °C) before their storage in liquid nitrogen at −196 °C. b Thawing procedure of immature mouse testes. c In vitro culture of frozen-thawed pre-pubertal mouse testes on agarose gels at a gas-liquid interphase, according to the various soaking temperatures used above. d Set of experiments performed after culture of the frozen-thawed pre-pubertal mouse testicular tissues (D DMSO, dpp day post-partum, FCS fetal calf serum, KSR knock-out serum replacement, L-15 Leibovitz medium, LN 2 liquid nitrogen, α-MEM alpha-minimum essential medium, RE retinol, RIA radioimmunoassay, S sucrose). (PDF 363 kb)
Fig. S2
Assessment of Leydig cell functional integrity during in vitro culture of frozen-thawed pre-pubertal (6.5 dpp) mouse testes using the −9 °C condition. Results indicate the mean of testosterone concentration in the culture medium under the various conditions tested. Data are expressed as mean ± SEM; n = 4 mouse testes for each condition. *Statistically significant difference between −9 °C and fresh tissue control; P < 0.05 (D day, NS not significant). (PDF 246 kb)
Rights and permissions
About this article
Cite this article
Arkoun, B., Dumont, L., Milazzo, JP. et al. Does soaking temperature during controlled slow freezing of pre-pubertal mouse testes influence course of in vitro spermatogenesis?. Cell Tissue Res 364, 661–674 (2016). https://doi.org/10.1007/s00441-015-2341-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-015-2341-2