Abstract
In the 20 years following the launching of the Human Genome Project, socio-ethical and legal responses to the policy issues raised have varied across jurisdictions. There seems, however, to be a move away from the more static, classical responses that characterized the first decade to a more epigenetic and complex one. The latter policy approach better reflects the dynamic nature of the science itself.
Similar content being viewed by others
Introduction
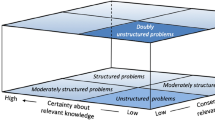
Beginning with the inception of the Human Genome Project in the 1990s, an analysis of trends in genomic policymaking reveals an interesting trajectory of seemingly haphazard approaches. In the first decade (1990–2000), the unfolding of policies on the ethical, legal and social implications (ELSI) of genomic research was surprisingly chronological. Indeed, “genethics” policies generally followed the development of the ethics guiding human biomedical research (Knoppers and Chadwick 2005). For the purpose of this analysis on the evolution of policymaking in genomics we will characterize the first decade as the static systems approach in contrast to, the more recent complex systems approach. The latter is typified by a tendency to move across and outside of disciplines and to foster international approaches via the creation of large infrastructures for future research. The case of biobanking will serve to illustrate this classification.
Static systems approach (1990–2000)
Generally, static systems exhibit linear and hierarchial characteristics. Such an ordered understanding views the chronological role-out of scientific discoveries as creating a parallel progression of regulatory responses. Like the naturalistic, separation of the species, legal systems themselves have binary separations of persons versus property, of drugs versus devices and of research versus therapy. Similarly, the one-gene-one protein has its counterpart in the one-test-one product equals one regulatory response that served as the direction for most policymaking. It has been argued that within this first decade, the medical, human rights, and public health models characterized genomic policymaking (Andrews 2001). All three models have their strengths and weaknesses.
Medical model
Drawing on the deontological basis of the physician-patient relationship, the medical model extends the self-regulatory, professional codes of conduct to the research setting. Guidelines, consensus statements, declarations and the like assimilate the researcher–participant relationship to the medical one albeit with a greater intensity of obligations to inform, to follow and to be monitored by ethics review boards. The medical model assumes, however, a form of physician–patient consensualism and trust based on ongoing communication that may not exist in the research relationship. While having the advantage of flexibility in that codes of conduct and guidelines can be updated and made specific to certain contexts (e.g. community genetics or population genomics), guidelines are ad hoc and subject to arbitrary (if not personal) interpretation via the researchers and ethics review committees that use them.
In the biobanking context, this model did, however, serve a useful purpose as it forestalled genetic-specific legislation. Generally, prior to the 1990s, the genetic (DNA) analysis of bodily tissues for research or left over after medical care did not receive much attention. For individuals, families and communities with monogenic conditions, linkage analysis and the subsequent storage of blood and tissue had no special status nor was an explicit consent sought for research on their DNA (Knoppers and Laberge 1989). This changed, however, as real or imagined ELSI-genetic scenarios began to play out in the literature. Soon the medical model as applied to genetic research was considered as an insufficient bulwark for the untoward familial and social consequences of DNA sampling (Clayton et al. 1995). Genetic exceptionalism (Murray 1997) and a proliferation of guidelines followed, often based on a conflation of medical ethics and human rights.
Human rights model
The convergence of the human rights of autonomy, privacy and justice with the same principles found in biomedical ethics, both strengthened and weakened the use of the human rights model. Since the 1948 Nuremberg Code, the Helsinki Declaration and the Belmont Principles, these time-honoured legal rights as found in international and constitutional legal instruments have been reinforced and expanded in the domain of medical research. Statements on genetic research from the ethics committee of international organizations such as World Health Organization (1997) or UNESCO (1997) began to specifically interpret these principles in the context of genetic research. The broad and open-ended nature of human rights lends itself to such a context-specific ethics interpretation in the field of genetic research. Scientific organizations such as the Human Genome Organization (HUGO) in its Statements founded its recommendations for researchers on this “marriage” of common ethico-legal principles (HUGO Ethics Committee 1996).
While, however, the medical model provides disciplinary sanctions for clinician–researchers, the human rights approach ultimately, leads to judicial interpretation and sanctions through the courts. Theoretically, a reference case could allow the higher courts to prospectively interpret human rights in the context of genomic biobanking research, but in all likelihood, human rights cases in the field of genetic research will centre on alleged infringements. Thus, the judicial system usually serves as an after the fact interpretation of human rights in genetic research.
This places the real power of translating autonomy, privacy and justice in the hands of ethics review committees. Familiar with clinical trials, these committees are often ill-equipped for the expertise required for the evaluations of emerging technologies involving bioinformatics, and prospective, population genomics research with longitudinal data and sample collection activities. Ethics review committees also lack transparency concerning decision-making making it difficult to know what are the precedents. They often offer contradictory interpretations on the same protocol, lack appeal mechanisms and vary in their ongoing governance and oversight of genetic research. In short, they act as quasi-judicial administrative tribunals but provide none of the procedural protections (Knoppers 2009). Indeed, the interpretation of human rights via the courts may serve not only to pronounce on what privacy and confidentiality mean in the biobanking context (as opposed to clinical research), but may also one day have to pronounce on the lack of natural justice mechanisms in current ethics review. Also interesting will be the adaptation of classical public health powers to the population health context of genomic research and biobanking.
Public health model
Traditionally, this approach has been associated with state powers as concerns infectious and communicable diseases, quarantine, mandatory screening, vaccines and obligatory reporting. To date, this model has rarely been used in the domain of genetic research. Even classical newborn screening programs are less an example of state public health powers than of paediatric professional practice. Public health is housed in government, and except perhaps for health surveillance mechanisms is not suited to genomic research or policymaking. This may change, however, as the issue of genomic susceptibility and resistance to public health risks (e.g. SARS, TB, avian flu, malaria, etc.) gain importance (Brosch et al. 2007; The Malaria Genomic Epidemiology Network 2008). Until, these recent pandemic scares, however, the usefulness of biobanks and associated genomic data for State intervention in prevention and public health promotion or even for the creation of public health genomics initiatives by the State to prepare for such global and national public health concerns was not present in the literature. The International Health Regulations of the World Health Organization demonstrate the need for the elaboration of such a public health genomics model both nationally and internationally (World Health Organization 2005).
One could argue that, to date, the attractiveness of the public health model is that it promotes state intervention through “genetic-specific” legislation be it on biobanking, genetic discrimination, or, genetic testing (GINA 2008; Council of Europe 2008). Legislation is presumed to provide efficiency, certainty and clarity thereby creating a zone of political and public comfort. This may well be illusionary, however, and perversely, underscore and reinforce genetic exceptionalism and thereby the potential for stigmatization. Indeed, public health genomics would be well-served through the development of screening and vaccination (e.g. cancer, HPV) programs and for defining those factors leading to other new interventions. It has been defined as “…” the responsible and effective translation of genome-based knowledge and technologies into public policies, programs and services for the benefit of population health (Burke et al. 2006).
Conclusion
This retrospective analysis of the three traditional models that typify the first decade of genomic research reveals the underlying genetic determinism and accompanying “monogenic” philosophy that fed the exceptionalist policies of the 1990s. This approach is being increasingly questioned as a sound basis for policymaking. Like with other medical information in the past such as HIV, cancer, psychiatric illness, etc., genetic information and its ethical challenges are becoming routine. Genetic information should not be privileged, although it remains sensitive medical information. Nevertheless, the dilemmas associated with highly penetrant, or familial disorders will continue to require special attention (Foster et al. 2006). In contrast, what characterizes genomic research and biobanks since 2000 however, is the interest in understanding the role of gene–environment interaction in common disorders. Thus, the dominance of monogenic conditions as a basis for intervention through policymaking via the three models is giving way to a more complex approach as the probabilistic role of both the environment and of genetic factors in common diseases increases in importance (Goh et al. 2007).
Complex systems approach (2000–)
The rise of systems biology and the concomitant understanding of the coupling of natural and human systems in epigenetic and dynamic relationships are challenging static, linear approaches to policymaking. One of the major forces behind a more networked (Sauer et al. 2007; Branscomb 2008) and “communal” and international research strategy is the open source/access movement with its origins in the information technologies community. This has an influence on the development of the field of genomics research characterized by the efforts of the International Human Genome Sequencing Consortium that provided the sequence map of the human genome in 2003. Since the completion of this map, efforts have turned to research on population health where research participants act as “citizens” in providing data and tissues for infrastructures (biobanks/repositories) that serve for future (as yet unknown) research projects. Finally, it may seem paradoxical, but it could be argued that ultimately, there could be a convergence of policymaking approaches, under such a heterogeneous systems understanding of science.
Communalism
While information technologies have long been interconnected and collaborative, the first attempt to envision the human genome at the level of the species as of interest to all of humanity is found in its characterization as the “common heritage of humanity”. This has been applied to the sea and outer space. While still recognizing the validity of intellectual property, the concept means that the human genome at the level of the species cannot be appropriated; benefits should be equally shared; use should be peaceful and protected for future generations, and, internationally governed and managed (Knoppers 1991). UNESCO’s 1997 Universal Declaration on the Human Genome and Human Rights adopted this approach for the human genome albeit in a “symbolic sense”, the practical implications seemingly giving rise to political issues for state sovereignty.
Concomitantly, the ideal of free and open dissemination of scientific knowledge for all humanity was bolstered by the networked information economy and epitomized by the creative, science commons seeking to lower barriers to research and data sharing (Joly 2007). Basic genomic knowledge has been characterized as a community resource—“a research project specifically devised and implemented to create a set of data, reagents or other material whose primary utility will be as a resource for the broad scientific community” (Wellcome Trust 2003). The most successful example of a robust public domain endeavour was the SNP consortium that provided the human genome sequence map (Thorisson and Stein 2003). This open model of international collaborative science led to the successful international HapMap project, whose data and samples are public and available to researchers from around the world (International HapMap Project website). Ensuing databases were considered as global public goods whose data were pre-emptive and precompetitive, thus avoiding intellectual property barriers on such early stage fundamental research (HUGO Ethics Committee 2002). The debate continues, but the move to encourage the publication of positive and negative findings (World Medical Association 2008), to create an international registry of clinical trials (WHO: International Clinical Trials Registry Platform) and to require data sharing (National Institutes of Health 2007) demonstrate the viability of this “democratization” movement. Its influence is most evident in the construction of national public infrastructures (i.e. biobanks) for future unspecified research where participants contribute not as patients but as citizens.
Citizenry
Since 2000, the rise of large, population infrastructures has been phenomenal. Realizing that the understanding of complex diseases required data on the interaction of an individual with the environment(s) over time and not just a disease by disease approach, the comprehension of phenotype expression, of normal genomic variation in modern heterogeneous populations has become a priority. Again, to maximize the enormous public investment in national biobanks, international collaborative efforts have emerged (Public Population Project in Genomics).
Approaches to population biobanking have not been uniform. Countries such as Estonia, Latvia, Sweden and Norway have adopted legislation specific to research in this area. Other countries here such as Spain and France have added sections on biobanking within legislation framing biomedical research generally. The majority have promoted guidance through professional codes of conduct. A common approach is to add an additional layer of governance via independent oversight structures (Wallace et al. 2008). Irrespective, the creation of more open-ended population resources for future research characterize this last decade.
Ethical challenges abound as most guidance is based on the increased emphasis on individual autonomy and privacy that emerged in human genetic research in the 1990s. Participation in the creation of such infrastructures underscores the ethics of solidarity as witnessed by the fact that there are no individual results. Indeed, traditional ethics guidance is ill-suited to the longitudinal, no-personal-benefit nature of these infrastructures involving the altruistic participation of healthy citizens with a requisite broad consent (King’s Law Journal Special Issue 2007). Moveover, in order to achieve statistical power and significance, international collaboration and data sharing are necessary and foreseen within such broad consent (Burton 2008). Elaborate data security mechanisms both protect the data and yet ensure its interoperability and transferability across borders (GenomEUtwin).
What is evident in the second decade is that while the traditional models still play a role in policymaking, increasingly, the relational, open and global nature of modern science is leading to more devolved regulatory approaches. This involves increased transparency and accountability for decision-making via governance structures as opposed to sole reliance on laws or core guiding principles. Paradoxically, the promises of personal genomics may well force this issue of governance as a matter of oversight and safety for “consumers” thereby creating convergence in the regulatory world.
Convergence
The advent of personal genomics companies offering online whole genome scanning services seems to have made a quantum leap in the democratization of genomic knowledge. The hope (hype?) of the broad availability of sequencing will foster increasing personal use. Leaving access costs aside (since they are constantly falling), the promises of precise predictive and personal scans are for the large part, however, empty and premature. Indeed, “[o]ver the next five years, the challenge for genome medicine is thus not to make a significant move into the clinic” (Cho 2009).
With perhaps the exception of pharmacogenetics not only as a screening tool for adverse events, but also for drug targeting, personalized medicine is far from ready for a direct-to-consumer approach. Moveover, “[a]lthough improving drug safety using data from drug metabolizing enzymes and transporter studies might be within reach, implementing drug individualization for optimal drug efficacy is significantly more challenging.” (Gurwitz et al. 2006).
The major obstacle to acquiring the scientific validity and specificity to move forward is the integration and use of population data together with personal, medical data in a systemic and systematic way across multiple levels of organization and time frames. Systems medicine seems to offer such an integrated strategy (Auffray 2009). As the next decade moves us from population biobanks to personal genomics, new regulatory challenges will occur since a “genome scan reveals information that is medical, genealogical and recreational” (Prainsack et al. 2008). It is precisely this convergence of the “populational” with the personal that will mark the next decade. Population databases will be used by disease studies and pharma to validate, replicate and compare. In universal health-care systems, the advent of electronic medical records—the informatic nexus between personal care, medication, and participation in clinical and or fundamental research—will be possible, thereby offering a more “holistic” approach to health.
Conclusion
The era of the “social genome” (Knoppers and Joly 2007) has produced a humanistic and solidarity-based approach to genome research, one that may be both more efficient and hopefully, more transparent. The issue remains, however, whether like the science, governance structures can go beyond national biobanks and become international to ensure respect of the public trust, participation and investment in large population studies and informatics in health care. Like the personal data privacy directives of the 1990s and the need for mutual safe harbour recognition between states, the international exchange of data in emerging consortia necessitates such mutual recognition of the validity of diverse, national models of policymaking and data security.
We would argue that the three models of the first decade could well serve a purpose in the next era of systems medicine. As much as possible, the medical profession should fulfil its obligation to offer informed advice and systematically follow-up patients and research participants while framing concomitant ethical obligations through prospective professional guidelines. The human rights model will have to encompass not only individual rights and duties, but also frame collective health rights that promote the public good. Public health crosses whole populations, and sub-populations. Genomics research will have to find its place as an important source of knowledge for population health and health systems planning. One thing is certain, policymaking will have to be as epigenetic and dynamic as the science!
References
Andrews LB (2001) A conceptual framework for genetic policy: comparing the medical, public health, and fundamental rights models. Wash Univ Law Q 79:221
Auffray C (2009) Systems medicine: the future of medical genomics and healthcare. Genome Med 1:2
Branscomb LM (2008) Research alone is not enough. Science 321:915–916
Brosch R, Gordon SV, Garnier T, Eiglmeier K, Frigui W, Valenti P, Dos Santos S, Duthoy S, Lacroix C, Garcia-Pelayo C, Inwald JK, Golby P, Garcia JN, Hewinson RG, Behr MA, Quail MA, Churcher C, Barrell BG, Parkhill J, Cole ST (2007) Genome plasticity of BCG and impact on vaccine efficacy. Proc Natl Acad Sci U S A 104:5596
Burke W, Khoury MJ, Stewart A, Zimmern RL, Group Bellagio (2006) The path from genome-based research to population health: development of an international public health genomics network. Genet Med 8:451
Burton PR, Hansell AL, Fortier I, Manolio TA, Khoury MJ, Little J, Elliott P (2008) Size matters: just how big is Big?: quantifying realistic sample size requirements for human genome epidemiology. Int J Epidemiol. http://ije.oxfordjournals.org/cgi/content/abstract/dyn147. Accessed 25 Aug 2008
Cho MK (2009) Translating genomics into the clinic: moving to the post-Mendelian world. Genome Med 1:7
Clayton EW, Steinberg KK, Khoury MJ, Thomson E, Andrews L, Kahn MJ, Kopelman LM, Weiss JO (1995) Informed consent for genetic research on stored tissue samples. JAMA 274:1786
Council of Europe (2008) Additional protocol to the convention on human rights and biomedicine, concerning genetic testing for health purposes, Strasbourg
Foster MW, Royal CDM, Sharp RR (2006) The routinisation of genomics and genetics: implications for ethical practices. J Med Ethics 32:635
GenomEUtwin. http://www.genomeutwin.org/
GINA (2008) Genetic Information Nondiscrimination Act of 2008, Public Law No. 110-233, 122 Stat. 881 (May 21)
Goh K-I, Cusick ME, Valle D, Childs B, Vidal M, Barabasi A-L (2007) The human disease network. Proc Natl Acad Sci U S A 104:8685–8690
Gurwitz D, Lunshof JE, Altman RB (2006) A call for the creation of personalized medicine databases. Nat Rev Drug Discov 5:23
HUGO Ethics Committee (1996) Statement on the principled conduct of genetic research, London
HUGO Ethics Committee (2002) Statement on human genomic databases, London
Joly Y (2007) Open source approaches in biotechnology: Utopia revisited. Maine Law Rev 59:386
King’s Law Journal Special Issue (2007) Governing genetic databases: collection, storage and use. Kings Law J 18:201–312
Knoppers BM (1991) Human dignity and genetic heritage, Law Reform Commission of Canada, 1991. ISBN: 0662580559
Knoppers BM (2009) Challenges to ethics review in health research. Health Law Review (in press)
Knoppers BM, Chadwick R (2005) Human genetic research: emerging trends in ethics. Nat Rev Genet 6:75
Knoppers BM, Joly Y (2007) Our social genome? Trends Biotechnol 25:284–288
Knoppers BM, Laberge C (1989) DNA sampling and informed consent. CMAJ 140:1023
Murray RF (1997) Genetic exceptionalism and future diaries: is genetic information different from other medical information? In: Rothstein MA (ed) Genetic secrets. Yale University Press, New Haven. ISBN 97–80300080636
National Institutes of Health (2007) Policy for sharing of data obtained in NIH supported or conducted genome-wide association studies (GWAS), United States
Prainsack B, Reardon J, Hindmarsh R, Gottweis H, Naue U, Lunshof JE (2008) Personal genomes: misdirected precaution. Nature 456:34
Public Population Project in Genomics (P3G). http://www.p3gconsortium.org
Sauer U, Heinemann M, Zamboni N (2007) Getting closer to the whole picture. Science 315:550–551
The International HapMap Project. http://www.hapmap.org/
The Malaria Genomic Epidemiology Network (2008) A global network for investigating the genomic epidemiology of malaria. Nature 456:732
Thorisson GA, Stein LD (2003) The SNP Consortium website: past, present and future. Nucleic Acids Res 31:124
UNESCO (1997) Universal Declaration on the Human Genome and Human Rights, Paris
Wallace S, Bédard K, Kent A, Knoppers BM (2008) Governance mechanisms and population biobanks: building a framework for trust. GenEdit 6:1–11. http://www.humgen.umontreal.ca/int/GE/en/2008-2.pdf
Wellcome Trust (2003) Sharing data from large-scale biological research projects: a system of tripartite responsibility, UK
World Health Organization (1997) Proposed international guidelines on ethical issues in medical genetics and genetic services, Geneva
World Health Organization (2005) International health regulations, Geneva
World Medical Association (2008) Declaration of Helsinki–Ethical principles for medical research involving human subjects, Seoul
World Health Organization. International clinical trials registry platform. http://www.who.int/ictrp/en/
Acknowledgments
Professor, Faculties of Law and Medicine, Canada Research Chair in Law and Medicine, Centre de Recherche en Droit Public, Université de Montréal. The author would like to thank Ma’n H. Abdul-Rahman, LL.B., for his kind assistance. This research was funded in part by Genome Canada and Genome Quebec and through the European Community’s Seventh Framework Programme (FP7/2007-2013), ENGAGE project, grant agreement HEALTH-F4-2007-201413.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Knoppers, B.M. Genomics and policymaking: from static models to complex systems?. Hum Genet 125, 375–379 (2009). https://doi.org/10.1007/s00439-009-0644-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00439-009-0644-7