Abstract
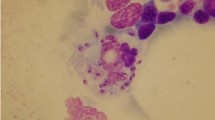
Visceral leishmaniasis (VL) remains a major health problem in old world, and India accounts for half of the world burden. The widespread emergence of resistance to standard drug in India poses a major obstacle in the control of leishmaniasis. Post-Kala-Azar dermal leishmaniasis (PKDL) is considered as main source of drug resistance. Experimental data indicate that resistance against newer drugs is also imminent. Therefore, in vitro studies were carried out to test minimum parasiticidal concentration of five conventional and newly introduced anti-leishmanial drugs against 20 field isolates of Leishmania donovani obtained from visceral and post-Kala-Azar dermal leishmaniasis patients of India. Study revealed wide range of variation in minimum inhibitory concentration of sodium antimony gluconate (SAG). PKDL isolates displayed significantly lower susceptibility to SAG and miltefosine than VL isolates with P value of 0.0006 and 0.0243, respectively. All clinical isolates had higher IC50 value for paromomycin and miltefosine as compared to reference strain indicating their vulnerability to develop unresponsiveness. However, isolates were uniformly susceptible to pentamidine and amphotericin B. The results of gene expression analysis of AQP1 were largely in agreement with phenotypic drug sensitivity results. Interestingly, significant down-regulation of AQP1 was observed in PKDL isolates as compared to VL isolates indicating their increased propensity for drug unresponsiveness. However, no significant difference in mRNA expression of LdMT and LdRos3 gene was found for two groups. The present study unravels valuable baseline scientific data showing variation in the drug susceptibility pattern in the L. donovani isolates. The information might have impact on the management and control of Indian visceral leishmaniasis.




Similar content being viewed by others
References
Addy M, Nandy A (1992) Ten years of Kala-Azar in west Bengal, part I. Did post-Kala-Azar dermal leishmaniasis initiate the outbreak in 24-Parganas? Bull World Health Organ 70:341–346
Ashutosh SS, Goyal N (2007) Molecular mechanisms of antimony resistance in Leishmania. J Med Microbiol 56:143–153
Calvopina M, Gomez EA, Sindermann H, Cooper PJ, Hashiguchi Y (2006) Relapse of new world diffuse cutaneous leishmaniasis caused by Leishmania (Leishmania) mexicana after miltefosine treatment. Am J Trop Med Hyg 75:1074–1077
de Oliveira JP, Fernandes F, Cruz AK, Trombela V, Monteiro E, Camargo AA, Barral A, de Oliveira CI (2007) Genetic diversity of Leishmania amazonensis strains isolated in northeastern Brazil as revealed by DNA sequencing, PCR-based analyses and molecular karyotyping. Kinetoplastid Biol Dis 6:5
Decuypere S, Rijal S, Yardley V, De DS, Laurent T, Khanal B, Chappuis F, Dujardin JC (2005) Gene expression analysis of the mechanism of natural Sb(V) resistance in Leishmania donovani isolates from Nepal. Antimicrob Agents Chemother 49:4616–4621
Dey A, Singh S (2007) Genetic heterogeneity among visceral and post-Kala-Azar dermal leishmaniasis strains from eastern India. Infect Genet Evol 7:219–222
Dutta A, Bandyopadhyay S, Mandal C, Chatterjee M (2005) Development of a modified MTT assay for screening antimonial resistant field isolates of Indian visceral leishmaniasis. Parasitol Int 54:119–122
El Tai NO, El FM, Mauricio I, Miles MA, Oskam L, El Safi SH, Presber WH, Schonian G (2001) Leishmania donovani: intraspecific polymorphisms of Sudanese isolates revealed by PCR-based analyses and DNA sequencing. Exp Parasitol 97:35–44
Gourbal B, Sonuc N, Bhattacharjee H, Legare D, Sundar S, Ouellette M, Rosen BP, Mukhopadhyay R (2004) Drug uptake and modulation of drug resistance in Leishmania by an aquaglyceroporin. J Biol Chem 279:31010–31017
Jha TK, Sundar S, Thakur CP, Bachmann P, Karbwang J, Fischer C, Voss A, Berman J (1999) Miltefosine, an oral agent, for the treatment of Indian visceral leishmaniasis. N Engl J Med 341:1795–1800
Kumar D, Kulshrestha A, Singh R, Salotra P (2009) In vitro susceptibility of field isolates of Leishmania donovani to miltefosine and amphotericin B: correlation with sodium antimony gluconate susceptibility and implications for treatment in areas of endemicity. Antimicrob Agents Chemother 53:835–838
Mandal S, Maharjan M, Singh S, Chatterjee M, Madhubala R (2010) Assessing aquaglyceroporin gene status and expression profile in antimony-susceptible and -resistant clinical isolates of Leishmania donovani from India. J Antimicrob Chemother 65:496–507
Mishra M, Biswas UK, Jha DN, Khan AB (1992) Amphotericin versus pentamidine in antimony-unresponsive Kala-Azar. Lancet 340:1256–1257
Mishra J, Saxena A, Singh S (2007) Chemotherapy of leishmaniasis: past, present and future. Curr Med Chem 14:1153–1169
Pandey BD, Pandey K, Kaneko O, Yanagi T, Hirayama K (2009) Relapse of visceral leishmaniasis after miltefosine treatment in a Nepalese patient. Am J Trop Med Hyg 80:580–582
Perez-Victoria FJ, Sanchez-Canete MP, Castanys S, Gamarro F (2006) Phospholipid translocation and miltefosine potency require both L. donovani miltefosine transporter and the new protein LdRos3 in Leishmania parasites. J Biol Chem 281:23766–23775
Sanyal RK (1985) Leishmaniasis in the Indian subcontinent. In: Chang KP, Bray RS (eds) Leishmaniasis. Elsevier Science, Amsterdam, pp 443–467
Shaked-Mishan P, Ulrich N, Ephros M, Zilberstein D (2001) Novel intracellular SbV reducing activity correlates with antimony susceptibility in Leishmania donovani. J Biol Chem 276:3971–3976
Singh S, Sivakumar R (2004) Challenges and new discoveries in the treatment of leishmaniasis. J Infect Chemother 10:307–315
Singh S, Chaudhry VP, Wali JP (1996) Transfusion-transmitted Kala-Azar in India. Transfusion 36:848–849
Singh S, Biswas A, Wig N, Aggarwal P, Sood R, Wali JP (1999) A new focus of visceral leishmaniasis in sub-Himalayan (Kumaon) region of northern India. J Commun Dis 31:73–77
Singh S, Sharma U, Mishra J (2011) Post-Kala-Azar dermal leishmaniasis: recent developments. Int J Dermatol 50:1099–1108
Sundar S, Olliaro PL (2007) Miltefosine in the treatment of leishmaniasis: clinical evidence for informed clinical risk management. Ther Clin Risk Manag 3:733–740
Sundar S, More DK, Singh MK, Singh VP, Sharma S, Makharia A, Kumar PC, Murray HW (2000) Failure of pentavalent antimony in visceral leishmaniasis in India: report from the center of the Indian epidemic. Clin Infect Dis 31:1104–1107
Thakur CP, Kumar K (1992) Post Kala-Azar dermal leishmaniasis: a neglected aspect of Kala-Azar control programmes. Ann Trop Med Parasitol 86:355–359
Thakur CP, Kanyok TP, Pandey AK, Sinha GP, Messick C, Olliaro P (2000) Treatment of visceral leishmaniasis with injectable paromomycin (aminosidine). An open-label randomized phase-II clinical study. Trans R Soc Trop Med Hyg 94:432–433
Zerpa O, Ulrich M, Blanco B, Polegre M, Avila A, Matos N, Mendoza I, Pratlong F, Ravel C, Convit J (2007) Diffuse cutaneous leishmaniasis responds to miltefosine but then relapses. Br J Dermatol 156:1328–1335
Acknowledgments
The authors wish to thank Dr. SK Bhattacharya, the then Director, Rajendra Memorial Institute of Medical Sciences, Patna and Dr. HK Majumder, Head, Infectious Disease and Immunology Division, Indian Institute of Chemical Biology, Calcutta for the kind gift of VL and PKDL strains used in this study. This work was supported by an intramural grant from All India Institute of Medical Sciences, New Delhi to SS. The financial assistance in the form of research fellowship from Council of Scientific and Industrial Research, Government of India, to JM is also acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mishra, J., Madhubala, R. & Singh, S. Visceral and post-Kala-Azar dermal leishmaniasis isolates show significant difference in their in vitro drug susceptibility pattern. Parasitol Res 112, 1001–1009 (2013). https://doi.org/10.1007/s00436-012-3222-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-012-3222-1