Abstract
Purpose
Colorectal cancer (CRC) rarely occurs in children and adolescents. This study aimed to perform a retrospective analysis and disclose more detailed information about CRC in patients under 20 years old.
Methods
Medical records of CRCs in patients under 20 years old referred to three tertiary hospitals in China from September 2000 to July 2019 were retrospectively reviewed. Clinicopathological characteristics, treatment processes and laboratory findings were summarized and treatment outcomes and prognostic factors were analyzed.
Results
A total of 33,394 CRC medical records were analyzed, and we identified seventy (0.21%) CRCs in patients under 20. The most common primary tumor location was the left hemicolon (35.7%). The prominent pathological types were mucinous adenocarcinoma (22.9%) and signet ring cell carcinoma (22.9%). Nearly half (47.1%) of the patients presented with distant metastasis at diagnosis. The fractions of patients with deficient mismatch repair (dMMR) protein expression and microsatellite instability-high (MSI-H) were 23.8% (5/21) and 71.4% (5/7), respectively. Forty-four patients underwent radical surgery. Fifty-five patients received chemotherapy and six patients received radiotherapy. One dMMR/MSI-H rectal cancer patient received immunotherapy and achieved a clinically complete response. The median overall survival (OS) time was 80 months. The 3-year and 5-year OS rates were 61.8% and 57.2%, respectively. An absence of distant metastasis was a favorable factor for OS. For stage II/III CRCs, classic adenocarcinoma and radical surgery were favorable factors for OS. For stage IV CRCs, primary location at the colon was a favorable factor for OS.
Conclusion
Child and adolescent CRC patients are likely to have distant metastasis, undifferentiated, left hemicolon location, and a dMMR/MSI-H phenotype at diagnosis. Additional efforts are needed to improve their survival outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third most common cancer in incidence and ranks second in terms of cancer-related mortality (Bray et al. 2018). Adolescent and young adult (AYA) cancers accounted for 5% of all newly diagnosed invasive cancers in the United States between 2011 and 2015 (Close et al. 2019). We have witnessed an overall trend of decreased incidence of CRC over the past few decades as a result of using colonoscopy and other screening modalities in the older population (Connell et al. 2017). However, CRC incidence in young individuals is steadily rising (Kasi et al. 2019). AYA CRCs present with more advanced stage, poorer cell differentiation, and higher prevalence of signet ring cell histology, and the primary tumors are commonly located in the left side of the colon at diagnosis. Although CRC accounted for only 2.5–3.5% of cancer incidence in adolescents from 15 to 19 years old from 2011 to 2015, the 5-year survival rate was lower than in many other cancers (Close et al. 2019). Both the incidence and mortality rates of CRC are increasing in China in recent decades (Arnold et al. 2017). There are few reports on child and adolescent CRCs in patients under 20 (Kaplan et al. 2019; Indini et al. 2017; Sultan et al. 2010; Yang et al. 2010), especially in China (Du et al. 2015). To better characterize the clinical features, treatment strategies, and outcomes of CRC in children and adolescents, we performed an analysis of CRCs from three tertiary hospitals in South China.
Materials and methods
Patient population
Patients with pathologically diagnosed CRC in three tertiary hospitals (Sun Yat-sen University Cancer Center, the First Affiliated Hospital, and the Sixth Affiliated Hospital of Sun Yat-sen University, Guangzhou, China) from September 2000 to July 2019 were initially considered. Eligibility criteria included the following characteristics: (1) pathologically diagnosed classic adenocarcinoma, mucinous adenocarcinoma (MA), or signet ring cell carcinoma (SRCC); and (2) under 20 years of age. Patients were excluded using following criteria: (1) prior history of other malignancies; and/or (2) severe hematopoietic, heart, lung, liver, or kidney dysfunction. Clinical characteristics, treatment process, laboratory findings, and survival outcomes were captured from the medical records and follow-up systems.
Ethics
The present study was performed in accordance with the ethical standards as presented in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards and was approved by the Ethics Committee of Sun Yat-sen University Cancer Center with a waiver of informed consent because this research was retrospective and did not involve accessing any patient identification data.
Tumor location
The colon comprises the left hemicolon, the right hemicolon, and the transverse colon. The left hemicolon includes the left flexura, the descending colon, and the sigmoid, and the right hemicolon comprises the cecum, the ascending colon, and the right flexura. The rectum compromises the anus to 15 cm above the anocutaneous line.
Staging and tumor biomarkers
All tumors were staged or restaged according to the 8th edition of the American Joint Committee on Cancer (AJCC) TNM staging system. Carcinoembryonic antigen (CEA) and carbohydrate antigen 19–9 (CA19-9) were assessed at diagnosis or when patients were referred to one of the above three hospitals.
Tumor molecular characterization
Primary tumors were used for tumor molecular analysis. Mismatch repair (MMR) proteins, including MLH1, MSH2, MSH6, and PMS2, were assessed by immunohistochemistry (IHC). Tumors were classified as MMR-deficient (dMMR) if loss of one or more of the proteins was shown. Microsatellite status was detected by next-generation sequencing (NGS) or polymerase chain reaction (PCR) of five microsatellite markers, including BAT25, BAT26, D5S346, D2S123, and D17S250. MSI-high (MSI-H) was defined as presence of ≥ 30% mutations as detected by NGS or ≥ 2 microsatellite marker instability by PCR. K-ras mutation was assessed by NGS and/or PCR.
Follow-up
All patients were followed at 3-month intervals during the first 2 years, at least every 6 months thereafter for an additional period of 3 years, and then once a year until March 2020. Overall survival (OS) was defined from the date of diagnosis until death from any cause or was censored at last follow-up.
Statistical analysis
Continuous data are presented as the median with range, and categorical data are presented as proportions (%). Proportions were compared using a χ2 test. Survival rates were compared with the log-rank test. A two-sided p value of < 0.05 was considered statistically significant. Covariates with p value < 0.05 by univariate analysis were subjected to multivariate analysis. All statistical analyses were performed using IBM SPSS Statistics 25.0 (IBM Co, Armork, NY, USA) and GraphPad Prism version 8.3.0 (GraphPad Software, Inc., La Jolla, CA, USA).
Results
Patient characteristics
A total of 33,394 CRC medical records were analyzed, and we identified 70 CRCs (0.21%) in patients who were under 20 years old with histological diagnoses of adenocarcinoma, some of whom were referred from other hospitals. The characteristics of the patients are shown in Table 1. Of the 70 patients, 28 were diagnosed from September 2000 to December 2009, and the other 42 patients were diagnosed between January 2010 and July 2019. The median age at diagnosis was 18 (range, 8–20), with 30 patients (42.9%) being less than 18 years old. The proportion of male and female patients was 60.0% and 40.0%, respectively. Eleven patients (15.7%) had a family history of malignant tumor, and only 3 (4.3%) had a family history of CRC (one was a parent).
Symptoms and presentation
Six (8.6%) patients presented with multiple symptoms. Common symptoms included abdominal pain (33/70, 47.1%), hemafecia (22/70, 28.6%), diarrhea (6/70, 8.6%), and abdominal distention (5/70, 7.1%). Three patients complained of acute intestinal obstruction and two patients felt an abdominal mass themselves. One patient presented with altered bowel habits, one patient had weight loss, and one patient was diagnosed incidentally during examination for his left leg pain (see Table 1).
Tumor location
The most common primary tumor location was the left hemicolon (25/70, 35.7%), followed by the rectum (19/70, 27.1%), right hemicolon (16/70, 22.9%), and transverse colon (8/70, 11.4%) (see Table 1). Synchronous multiple primary tumors of the cecum and sigmoid were only confirmed in one patient.
Pathology and staging
Classic adenocarcinoma, MA and SRCC were diagnosed in 38 patients (54.3%), 16 patients (22.9%), and 16 patients (22.9%), respectively. Almost all MAs and SRCCs were in the colon except four rectal MAs and one rectal SRCC. Thirty-three patients (47.1%) presented with distant metastasis in the abdominal and pelvic cavity (n = 16), liver parenchyma (n = 9), peritoneal surface (n = 8), lung (n = 3), distant lymph nodes (n = 3), bone (n = 2), and ovarian parenchyma (n = 1). Regional lymph node status was available in 51 patients, 41 of whom had positive regional lymph nodes. None of the patient presented with stage I disease. The number of patients with stage II and III disease was 9 and 25, respectively. Staging in 3 patients was unclear, but 2 of them were stage II or III. There were 36 patients (51.4%) with locally advanced CRC (LACRC) and 33 patients (47.1%) with distant metastasis (see Table 1).
Laboratory and molecular tests
Among 46 patients with available serum CEA and CA19-9 data, 29 patients (63.0%) exhibited elevated CEA (> 5 ng/ml) and 19 patients (41.3%) exhibited elevated CA19-9 (> 35 U/ml) levels (see Table 1).
Eleven patients exhibited K-ras mutations, and the proportion of K-ras mutation was 54.6% (6/11) (see Table 1).
MMR proteins were examined in 21 patients. Five patients (23.8%) exhibited dMMR. MLH1 and PMS2 were both negative in two rectal cancer patients, MSH2 and MSH6 were both negative in another rectal cancer patient and a left hemicolon cancer patient, and PMS2 and MSH2 were both negative in one patient with transverse colon cancer.
Microsatellite status was assessed in seven patients. Five patients exhibited MSI-H, three of whom had rectal cancer and two of whom had left hemicolon cancer. Microsatellite stability (MSS) was found in one right hemicolon cancer patient and one transverse colon cancer patient.
Five patients were detected with both MMR and MSI. Two were dMMR and MSI-H; one was pMMR and MSS. MMR and MSI status was inconsistent in two patients. One was pMMR but MSI-H, and the other was dMMR but MSS. Detailed MMR and MSI information in these five patients is shown in Table 2.
Treatment and curative effect
Twenty-five locally advanced colon cancer patients underwent radical surgery. Three received neoadjuvant treatment, with a FOLFOX (5-fluorouracil, oxaliplatin plus leucovorin) regimen in 2 patients and neoadjuvant radiotherapy in one patient. Downstaging was not observed in these three patients, but all of them received adjuvant chemotherapy with FOLFOX regimen after surgery. Twenty patients did not receive neoadjuvant treatment, only adjuvant chemotherapy, with 12 patients receiving CAPOX (capecitabine plus oxaliplatin) and 8 patients receiving FOLFOX. The remaining two patients underwent surgery only.
In 11 locally advanced rectal cancer patients, only 4 (36.4%) received neoadjuvant therapy. One received CAPOX with Avastin combined with radiotherapy as part of a clinical trial, and he experienced pathological complete remission (pCR) after surgery. One received CAPOX combined with radiotherapy, and another received FOLFOX chemotherapy only. The pathology of these latter two patients after surgery suggested T and N downstaging. The last patient received CAPOX combined with radiotherapy. However, her tumor did not exhibit obvious regression and could not be completely removed, so palliative colostomy was performed.
dMMR and MSI-H were confirmed after one cycle of capecitabine oral administration for a distal T3N1M0 rectal cancer patient, demonstrating that immunotherapy alone was applied in her case. Pembrolizumab was given for six cycles with the addition of Ipilimumab in the second and third cycles. Clinical complete response (cCR) of the tumor was found after the sixth cycle of immunotherapy. A watch and wait strategy was suggested for her, and Pembrolizumab was prescribed continuously for another four cycles.
For the 33 patients who presented with distant metastasis, 5 patients did not receive any anti-cancer treatment, and another 3 patients had palliative chemotherapy only. The remaining 25 patients underwent surgery, with 10 having radical resection of primary and metastatic foci, and 15 underwent palliative surgery. Among these 25 patients, 4 received preoperative chemotherapy, 15 received postoperative chemotherapy, 1 received adjuvant radiotherapy, and 1 received chemotherapy both before and after surgery.
In summary, 44 patients underwent radical surgery and 16 patients underwent palliative surgery. Fifty-six patients received chemotherapy, and 6 patients received radiotherapy.
Survival analysis
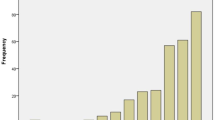
The median follow-up time of patients was 31 (0–203) months. Among all 70 patients, 4 (3.3%) were lost to follow-up. The median OS was 80.0 months for all patients. The 3-year and 5-year OS rates were 61.8% and 57.2%, respectively. When we investigated the association between clinical factors and outcomes using univariate analysis, only stage II/III (p = 0.001) was significantly associated with favorable survival (Table 3, Fig. 1).
We then explored factors affecting the survival of locally advanced and distant metastatic CRCs.
The median OS did not reach for locally advanced CRCs. The 3-year and 5-year OS rates were 77.8% and 73.5%, respectively. Classic adenocarcinoma (p = 0.019) (Table 4, Fig. 2) and radical surgery (p = 0.025) (Table 4) were significantly associated with favorable OS in univariate analysis. The 3-year and 5-year OS rates of classic adenocarcinoma were 86.4% and 86.4%, respectively, and the 3-year and 5-year OS rates of radical surgery were 80% and 75.6%, respectively. When the aforementioned factors were compared by a multivariate model using Cox proportional hazards regression analysis, radical surgery had the lower hazard ratio (HR) of 0.042 (95% CI 0.003–0.584; p = 0.018), and classic adenocarcinoma had an HR of 0.182 (95% CI 0.045–0.734; p = 0.017) (Table 4).
With respect to distant metastatic CRCs, the median OS was 23.4 months, and the 3-year and 5-year OS rates were 44.7% and 39.7%, respectively. Only primary tumor location in the colon was significantly associated with favorable survival (p = 0.044) (Table 5, Fig. 3a). The 3-year and 5-year OS rates of colon cancer were 56.7% and 49.6%, respectively. The median OS in patients who underwent radical surgery was much longer than that in patients who did not (92.83 months vs. 9.5 months), although the p value was not significant (p = 0.053) (Table 5, Fig. 3b).
Discussion
CRC rarely occurs in children and adolescents who are less than 20 years old. There are some case reports and small cohorts of child and adolescent CRCs (Shankar et al. 1999; Andersson et al. 1976; Ahn et al. 2017; Yang et al. 2015; Koh et al. 2015; Yeh et al. 2017; Vastyan et al. 2001; Noh et al. 2013), but there were only three cohorts (Sultan et al. 2010; Yang et al. 2010; Hill et al. 2007) with more than 50 patients found on PubMed, two of which were from the Surveillance, Epidemiology, and End Results (SEER) database. According to SEER statistics in the USA (Sultan et al. 2010), the age-adjusted incidence rate of CRC in children and adolescents was only 0.38 per million, and only 159 CRCs occurred in children and adolescents between January 1973 and December 2005. It is also rare in China. Of the 11,503 CRCs in the Cancer Hospital, Chinese Academy of Medical Sciences from January 1999 to December 2009, there were only 19 CRCs in patients who were between 10 and 20 years old (Du et al. 2015). No large cohort of child and adolescent CRCs has been previously reported from China. We only identified 70 patients under 20 from September 2000 to July 2019 in three hospitals. The present study is one of the largest cohorts to examine the clinicopathological and prognostic features of this disease.
The latest CRC statistics show that distant-stage diagnoses in patients younger than 50 years, 50–64 years, and 65 years and older are approximately 26%, 23%, and 19%, respectively (Siegel et al. 2020). However, nearly half of patients were stage IV in the present cohort. Presenting signs and symptoms in CRC are often vague and nonspecific, and no routine screening has been suggested. Child and adolescent CRC may have severe delays in diagnosis and/or possess intrinsically more aggressive behavior. Therefore, additional effort is needed for early recognition of this malignancy.
In previous reports, histological types of MA and SRCC are approximately 10% and 1% among all CRCs (Verhulst et al. 2012; Gopalan et al. 2011; Nitsche et al. 2013; Hyngstrom et al. 2012), but the proportions of MA and SRCC are higher in children and adolescents than in adults (Kaplan et al. 2019). In the current study, MA (22.9%) and SRCC (22.9%) histology was observed much more frequently than reported in adults. Several studies have indicated poor prognosis in patients with mucinous histology (Verhulst et al. 2012; Hyngstrom et al. 2012; Sung et al. 2008). However, other studies found that neither MA nor SRCC was an independent predictor of decreased survival (Li et al. 2019; Nitsche et al. 2016). Herein, we found that MA and SRCC indicated poor prognosis for LACRC.
Due to the rarity of CRC in patients from such young age groups, clinical management and treatment approaches are generally decided according to experiences from the management of adult patients. The NCCN and ESMO guidelines both recommend multimodal treatment of locally advanced rectal cancer (LARC), involving neoadjuvant concurrent fluoropyrimidine-based chemotherapy with pelvic radiation, total mesorectal excision (TME), and adjuvant chemotherapy. In our study, among the nine LARC patients who underwent radical surgery, only three received neoadjuvant chemoradiation. Infertility might be the primary reason for omitting radiotherapy in LARC patients. Radical surgery was not successfully performed in two patients, both of whom died within 2 years after diagnosis.
For metastatic patients, surgery and chemotherapy were the most mainstream treatments in the present study and five patients did not receive any anti-cancer treatment for some reason. Radical surgery, which occurred in approximately 33.3% of patients in our cohort, may represent the only method to prolong survival for them. A previously study reported 5-year survival rates in patients diagnosed with distant metastasis from the ages of 20–49, 50–64, and 65 and older of 21%,16%, and 10%, respectively (Siegel et al. 2020). In our study, the 5-year OS rate of CRCs in patients under 20 was 39.7%, which is much higher than in patients older than 20. The higher rate of radical surgery may contribute to this increased rate of survival.
Health providers should do further investigations, such as genetic studies, to better understand the disease and to identify age-appropriate solutions. Clinicians and patients should be more engaged because more drugs are currently available, such as molecular targeted drugs and a multidisciplinary therapy model, which is implemented in most hospitals.
dMMR was represented in 15–20% of stage II/III CRCs and in approximately 5% in the metastatic setting (Auclin et al. 2017). Five (23.8%) patients were dMMR, and 4 (66.7%) patients were MSI-H in our cohort, which is far higher than rates observed in adults. As dMMR/MSI-H is a major risk factor for CRC and involves a high percentage of dMMR/MSI-H in children and adolescent CRC patients, it is necessary to assess dMMR/MSI-H status when children and adolescents are diagnosed with CRC. However, MSI/MMR status was only available in a small number of patients, and more patients are needed for further validation. There was also a discrepancy between the results of immunohistochemistry and molecular detection in one patient who was dMMR but MSS and in one patient who was pMMR but MSI-H in our cohort. There are some reasons for this discrepancy. Some MMR gene variants do not affect the structure of their corresponding antigens and allow for retained normal MMR protein expression, but MMR proteins cannot recognize and repair DNA damage. Deficiencies in certain MMR proteins, such as MSH6, are not sufficient to result in MSI. Assessment of MSI and dMMR status discrepancy can be associated with a false-positive or a false-negative. Immune checkpoint blockades (ICBs), such as anti-PD-1 antibody and anti-CTLA-4 antibody, are effective in MSI-H/dMMR metastatic CRC. Recent studies in the refractory CRC setting have led to US Food and Drug Administration approvals for Pembrolizumab and Nivolumab (with or without Ipilimumab) for MSI-H/dMMR metastatic CRC.
In this study, the patient who received ICBs as neoadjuvant treatment achieved cCR and did not have surgery. Recently, PD-1 plus CTLA-4 blockade was demonstrated as highly effective in early-stage dMMR colon cancers (Chalabi et al. 2020). For the higher percentage of dMMR/MSI-H in child and adolescent CRCs, these patients may greatly benefit from immunotherapy. However, only a few patients have been reported (Chalabi et al. 2020; Zhang et al. 2019; Liu et al. 2020), and more data are needed for confirming and determining the best combination of immunotherapy with or without chemotherapy and/or radiotherapy to achieve a higher complete response rate and longer OS. There are some ongoing clinical trials attempting to add ICBs as neoadjuvant treatments for LACRC. In addition, we initiated a phase II clinical trial to combine PD-1 blockade with chemoradiation for dMMR/MSI-H unresectable CRCs. Genetic testing should be performed upon initial diagnosis for all child and adolescent CRCs, and immunotherapy is a promising modality for facilitating survival benefits in these patients.
There are some limitations to our study. This study is not a prospective cohort and has some of the inherent inadequacies of retrospective investigations. For example, molecular detections were available in only a small number of patients. In addition, the cohort covered nearly 20 years, thus a proportion of patients were lost, which may cause bias during analysis. Consequently, our observations warrant further consideration and validation in a larger patient series.
Conclusions
Child and adolescent CRCs are prone to having distant metastasis, poor pathological type, left hemicolon location, and dMMR/MSI-H phenotype. Fortunately, active comprehensive treatment, including radical surgery, conveys a survival benefit. In addition, it is necessary to do a comprehensive examination in those who have symptoms as early as possible due to the prognosis of early-stage patients being much better.
Data availability
The data and material that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- CRC:
-
Colorectal cancer
- dMMR:
-
Deficient of mismatch repair
- MSI-H:
-
Microsatellite instability-high
- OS:
-
Overall survival
- AYA:
-
Adolescent and young adult
- MA:
-
Mucinous adenocarcinoma
- SRCC:
-
Signet ring cell carcinoma
- AJCC:
-
American Joint Committee on Cancer
- TNM:
-
Tumor-node-metastasis
- CEA:
-
Carcinoembryonic antigen
- CA19-9:
-
Carbohydrate antigen 19–9
- MMR:
-
Mismatch repair
- IHC:
-
Immunohistochemistry
- NGS:
-
Next-generation sequencing
- PCR:
-
Polymerase chain reaction
- K-ras:
-
Kirsten rat sarcoma viral oncogene
- LACRC:
-
Locally advanced colorectal cancer
- MSS:
-
Microsatellite stability
- pMMR:
-
Proficient of mismatch repair
- pCR:
-
Pathological complete remission
- cCR:
-
Clinical complete response
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- SEER:
-
Surveillance, Epidemiology, and End Results
- NCCN:
-
National Comprehensive Cancer Network
- ESMO:
-
European Society for Medical Oncology
- LARC:
-
Locally advanced rectal cancer
- TME:
-
Total mesorectal excision
- ICB:
-
Immune checkpoint blockade
References
Ahn CH, Kim SC (2017) Two case reports: colorectal adenocarcinoma in children. Med (Balt) 96(46):e8074. https://doi.org/10.1097/MD.0000000000008074
Andersson A, Bergdahl L (1976) Carcinoma of the colon in children: a report of six new cases and a review of the literature. J Pediatr Surg 11(6):967–971. https://doi.org/10.1016/s0022-3468(76)80075-9
Arnold M, Sierra M, Laversanne M, Soerjomataram I, Jemal A, Bray F (2017) Global patterns and trends in colorectal cancer incidence and mortality. Gut 66(4):683–691. https://doi.org/10.1136/gutjnl-2015-310912
Auclin E, Zaanan A, Vernerey D, Douard R, Gallois C, Laurent-Puig P et al (2017) Subgroups and prognostication in stage III colon cancer: future perspectives for adjuvant therapy. Ann Oncol 28(5):958–968. https://doi.org/10.1093/annonc/mdx030
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Chalabi M, Fanchi LF, Dijkstra KK, Van den Berg JG, Aalbers AG, Sikorska K et al (2020) Neoadjuvant immunotherapy leads to pathological responses in MMR-proficient and MMR-deficient early-stage colon cancers. Nat Med 26(4):566–576. https://doi.org/10.1038/s41591-020-0805-8
Close AG, Dreyzin A, Miller KD, Seynnaeve B, Rapkin LB (2019) Adolescent and young adult oncology-past, present, and future. CA Cancer J Clin 69(6):485–496. https://doi.org/10.3322/caac.21585
Connell LC, Mota JM, Braghiroli MI, Hoff PM (2017) The rising incidence of younger patients with colorectal cancer: questions about screening, biology, and treatment. Curr Treat Options Oncol 18(4):23. https://doi.org/10.1007/s11864-017-0463-3
Du F, Shi SS, Sun YK, Wang JW, Chi Y (2015) Clinicopathological characteristics and prognosis of colorectal cancer in Chinese adolescent patients. Chin Med J (Engl) 128(23):3149–3152. https://doi.org/10.4103/0366-6999.170256
Gopalan V, Smith RA, Ho YH, Lam AK (2011) Signet-ring cell carcinoma of colorectum–current perspectives and molecular biology. Int J Colorectal Dis 26(2):127–133. https://doi.org/10.1007/s00384-010-1037-z
Hill DA, Furman WL, Billups CA, Riedley SE, Cain AM, Rao BN et al (2007) Colorectal carcinoma in childhood and adolescence: a clinicopathologic review. J Clin Oncol 25(36):5808–5814. https://doi.org/10.1200/JCO.2007.12.6102
Hyngstrom JR, Hu CY, Xing Y, You YN, Feig BW, Skibber JM et al (2012) Clinicopathology and outcomes for mucinous and signet ring colorectal adenocarcinoma: analysis from the national cancer data base. Ann Surg Oncol 19(9):2814–2821. https://doi.org/10.1245/s10434-012-2321-7
Indini A, Bisogno G, Cecchetto G, Vitellaro M, Signoroni S, Massimino M et al (2017) Gastrointestinal tract carcinoma in pediatric and adolescent age: the Italian TREP project experience. Pediatr Blood Cancer 64:12. https://doi.org/10.1002/pbc.26658
Kaplan MA, Ozaydin S, Yerlikaya H, Karaagac M, Gumus M, Cil T et al (2019) Clinicopathologic and prognostic differences between three different age groups (child/adolescent, young adults, and adults) of colorectal cancer patients: a multicentre study. Oncol Res Treat 42(10):516–522. https://doi.org/10.1159/000502120
Kasi PM, Shahjehan F, Cochuyt JJ, Li Z, Colibaseanu DT, Merchea A (2019) Rising proportion of young individuals with rectal and colon cancer. Clin Colorectal Cancer 18(1):e87–e95. https://doi.org/10.1016/j.clcc.2018.10.002
Koh KJ, Lin LH, Huang SH, Wong JU (2015) CARE–pediatric colon adenocarcinoma: a case report and literature review comparing differences in clinical features between children and adult patients. Med (Balt) 94(6):e503. https://doi.org/10.1097/MD.0000000000000503
Li C, Zheng H, Jia H, Huang D, Gu W, Cai S et al (2019) Prognosis of three histological subtypes of colorectal adenocarcinoma: A retrospective analysis of 8005 Chinese patients. Cancer Med 8(7):3411–3419. https://doi.org/10.1002/cam4.2234
Liu DX, Li DD, He W, Ke CF, Jiang W, Tang JH et al (2020) PD-1 blockade in neoadjuvant setting of DNA mismatch repair-deficient/microsatellite instability-high colorectal cancer. Oncoimmunology 9(1):1711650. https://doi.org/10.1080/2162402X.2020.1711650
Nitsche U, Zimmermann A, Späth C, Müller T, Maak M, Schuster T et al (2013) Mucinous and signet-ring cell colorectal cancers differ from classical adenocarcinomas in tumor biology and prognosis. Ann Surg 258(5):775–783. https://doi.org/10.1097/SLA.0b013e3182a69f7e
Nitsche U, Friess H, Agha A, Angele M, Eckel R, Heitland W et al (2016) Prognosis of mucinous and signet-ring cell colorectal cancer in a population-based cohort. J Cancer Res Clin Oncol 142(11):2357–2366. https://doi.org/10.1007/s00432-016-2224-2
Noh SY, Oh SY, Kim SH, Kim HY, Jung SE, Park KW (2013) Fifteen-year-old colon cancer patient with a 10-year history of ulcerative colitis. World J Gastroenterol 19(15):2437–2440. https://doi.org/10.3748/wjg.v19.i15.2437
Shankar A, Renaut AJ, Whelan J, Taylor I (1999) Colorectal cancer in adolescents. Ann R Coll Surg Engl 81(2):100–104
Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC et al (2020) (2020) Colorectal cancer statistics. CA Cancer J Clin 70(3):145–164. https://doi.org/10.3322/caac.21601
Sultan I, Rodriguez-Galindo C, El-Taani H, Pastore G, Casanova M, Gallino G et al (2010) Distinct features of colorectal cancer in children and adolescents: a population-based study of 159 cases. Cancer 116(3):758–765. https://doi.org/10.1002/cncr.24777
Sung CO, Seo JW, Kim KM, Do IG, Kim SW, Park CK (2008) Clinical significance of signet-ring cells in colorectal mucinous adenocarcinoma. Mod Pathol 21(12):1533–1541. https://doi.org/10.1038/modpathol.2008.170
Vastyan AM, Walker J, Pintér AB, Gerrard M, Kajtar P (2001) Colorectal carcinoma in children and adolescents–a report of seven cases. Eur J Pediatr Surg 11(5):338–341. https://doi.org/10.1055/s-2001-18548
Verhulst J, Ferdinande L, Demetter P, Ceelen W (2012) Mucinous subtype as prognostic factor in colorectal cancer: a systematic review and meta-analysis. J Clin Pathol 65(5):381–388. https://doi.org/10.1136/jclinpath-2011-200340
Yang R, Cheung MC, Zhuge Y, Armstrong C, Koniaris LG, Sola JE (2010) Primary solid tumors of the colon and rectum in the pediatric patient: a review of 270 cases. J Surg Res 161(2):209–216. https://doi.org/10.1016/j.jss.2008.12.003
Yang S, Liu G, Zheng S, Dong K, Ma Y, Xiao X (2015) Signet-ring cell carcinoma of the colon: a case report of a 9-year-old boy. Oncol Lett 10(3):1632–1634. https://doi.org/10.3892/ol.2015.3403
Yeh YS, Chang YT, Ma CJ, Huang CW, Tsai HL, Chen YT et al (2017) First-decade patient with colorectal cancer carrying both germline and somatic mutations in APC gene. BMC Cancer 17(1):849. https://doi.org/10.1186/s12885-017-3878-0
Zhang J, Cai J, Deng Y, Wang H (2019) Complete response in patients with locally advanced rectal cancer after neoadjuvant treatment with nivolumab. Oncoimmunology 8(12):e1663108. https://doi.org/10.1080/2162402X.2019.1663108
Acknowledgements
We thank the medical staff and patients for their contribution to this study.
Funding
This study was funded by the National Natural Science Foundation of China (grant number 81672987).
Author information
Authors and Affiliations
Contributions
Conceptualization: CZ, WX; Methodology: Xiaohao Wang; Data curation: CZ, HC, SN; Formal analysis: QW, HC; Resources: Xiaojun Wu, PD, ZP, Xiangbo Wan, YB; Software: Xiaohao Wang; Writing—Original draft: CZ, WX; Writing-Review and Editing: YG.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Approval was obtained from the Ethics Committee of Sun Yat-sen University Cancer Center. The procedures used in this study adhere to the tenets of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhou, C., Xiao, W., Wang, X. et al. Colorectal cancer under 20 years old: a retrospective analysis from three tertiary hospitals. J Cancer Res Clin Oncol 147, 1145–1155 (2021). https://doi.org/10.1007/s00432-020-03397-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-020-03397-2