Abstract
Purpose
Fusion genes can be therapeutically relevant if they result in constitutive activation of oncogenes or repression of tumor suppressors. However, the prevalence and role of fusion genes in female cancers remain largely unexplored. Here, we investigate the fusion gene landscape in triple-negative breast cancer (TNBC) and high-grade serous ovarian cancer (HGSOC), two subtypes of female cancers with high molecular similarity but limited treatment options at present.
Methods
RNA-seq was utilized to identify fusion genes in a cohort of 18 TNBC and HGSOC patients treated with the PI3K inhibitor buparlisib and the PARP inhibitor olaparib in a phase I clinical trial (NCT01623349). Differential gene expression analysis was performed to assess the function of fusion genes in silico. Finally, these findings were correlated with the reported clinical outcomes.
Results
A total of 156 fusion genes was detected, whereof 44/156 (28%) events occurred in more than one patient. Low recurrence across samples indicated that the majority of fusion genes were private passenger events. The long non-coding RNA MALAT1 was involved in 97/156 (62%) fusion genes, followed in prevalence by MUC16, FOXP1, WWOX and XIST. Gene expression of FOXP1 was significantly elevated in patients with vs. without FOXP1 fusion (P= 0.02). From a clinical perspective, FOXP1 fusions were associated with a favorable overall survival.
Conclusions
In summary, this study provides the first characterization of fusion genes in a cohort of TNBC and HGSOC patients. An improved mechanistic understanding of fusion genes will support the future identification of innovative therapeutic approaches for these challenging diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most frequently diagnosed female cancer in the United States with a lifetime risk of 12% and an expected number of 268,600 new cases and 41,760 deaths in 2019 (American Cancer Society 2019a). Triple-negative breast cancer (TNBC) occurs in 12–17% of breast cancer and is a subtype that does not express estrogen receptor (ER), progesterone receptor (PR) or human epidermal growth factor receptor 2 (HER2) (Foulkes et al. 2010). TNBC is an aggressive disease with high rates of metastasis and/or recurrence and has worse prognosis compared to HER2 + and ER + subtypes. Since TNBC patients do not respond to hormonal treatment or HER2-directed therapy, treatment options are restricted to chemotherapy such as platinum/taxane or alkylating agents.
Ovarian cancer represents the fifth most frequently diagnosed female cancer in the United States with a lifetime risk of 1.3% and an estimated number of 22,530 new cases and 13,980 deaths in 2019 (American Cancer Society 2019b). Advanced stage high-grade serous ovarian cancer (HGSOC) occurs in 70% of these patients (Koonings et al. 1989). Standard treatment for HGSOC consists of surgery followed by platinum/taxane chemotherapy. Despite these measures, the prognosis remains grim. 25% of HGSOC recur within the first 6 months after treatment and a 5-year overall survival (OS) of 31% has been reported (Jemal et al. 2009).
On the genomic level, TNBC and HGSOC share similar alterations, including widespread genomic instability, p53 mutations, deficiency in DNA damage repair and homologous recombination as well as PI3-kinase pathway activation (Cancer Genome Atlas Network 2012; Bell et al. 2011). Prior analyses indicate that PI3-kinase suppression can further inhibit homologous DNA double-strand break repair by impairing the non-oxidative pentose phosphate pathway (PPP) which physiologically provides ribose-5-phosphate for nucleoside synthesis (Hu et al. 2016). This, along with preclinical data derived from a PDX mouse model (Juvekar et al. 2012), provides the rationale to examine buparlisib and olaparib as a dual strategy to block PI3-kinase signaling and DNA repair in both diseases.
We recently assessed the safety and efficacy of this approach in the context of a multicenter phase I trial for patients with recurrent TNBC and HGSOC. Clinical responses in this study were observed in 28% of TNBC and in 29% of HGSOC patients (Matulonis et al. 2017).
Over the past years, the emergence of next-generation sequencing (NGS) technologies has dramatically transformed our ability to comprehensively assess genomic features and their impact on cancer pathogenesis and outcome. Amongst others, NGS allows for the study of fusion genes which result from translocations, interstitial deletions or chromosomal inversions of two separate genes (Mertens et al. 2015).
These genes can be therapeutically relevant if they result in constitutive activation of fused oncogenes or repression of fused tumor suppressor genes. This is exemplified by the oncogenic BCR–ABL1 fusion gene, which was first detected in patients with chronic myelogenous leukemia (CML). The inhibition of BCR–ABL1 by the tyrosine kinase inhibitor imatinib led to dramatically improved molecular responses and survival of CML patients (Roy et al. 2006). Fusion genes have also been reported in solid tumors, e.g., TMPRSS2–ERG in prostate cancer, EML4–ALK in lung cancer and EWS–FL1 in Ewing’s sarcoma (Tomlins et al. 2005; Soda et al. 2007; Owen et al. 2008). In female cancers, the ETV6–NTRK3 fusion gene has previously been described, but its prevalence is exclusively limited to secretory breast cancer in which it may be detected in > 90% of all cases (Tognon et al. 2002). The prevalence and therapeutic potential of fusion genes in TNBC and HGSOC remain unexplored.
In the present study, we investigate the fusion gene landscape in the transcriptome of 18 TNBC and HGSOC patients who were treated with buparlisib and olaparib in the aforementioned phase I trial using RNA sequencing. We identify fused genes, assess in silico whether the resulting product is still functional, and investigate whether fusion genes result in differential expression of the respective genes involved. We correlate our findings with the reported clinical outcomes and evaluate if fusion genes are associated with clinical outcomes.
Materials and methods
Patient and tumor samples
The primary objective of this study was to investigate the fusion gene landscape and the effect of fusions on the function and expression of each partner gene. Samples were derived from a subset of patients from a phase I trial (NCT01623349) (Matulonis et al. 2017). The trial tested the safety and efficacy of the PI3K inhibitor buparlisib and the PARP inhibitor olaparib in a 3 + 3 dose-escalation design in patients with TNBC (n = 24) and HGSOC (n = 46). Out of 70 enrolled patients, formalin-fixed paraffin-embedded primary tumor biopsies were available for nine TNBC and nine HGSOC patients (Table 1).
RNA extraction and transcriptome sequencing
RNA was extracted using the Qiagen RNeasy FFPE kit (Germantown, MD) adhering to the manufacturer’s instructions. Library preparation was performed with the TruSeq RNA Access Library Prep Kit (Illumina, San Diego, CA). Paired-end, 75-bp reads were generated on a NextSeq 500 using a High Output, 150 cycle kit with v2 chemistry (Illumina).
Quality control
Data output from sequencing was generated as raw test files in FASTQ format. All FASTQ files passed quality control using FASTQC v0.11.2 (http://www.bioinformatics.babraham.ac.uk/projects/fastqc). Splice-aware genome alignment was performed using the STAR aligner tool v020201 (Dobin et al. 2013). Reads were mapped to the human genome GRCh37 (hg19). Gene expression at transcript-level resolution was calculated using RSEM v.1.2.31 (Li and Dewey 2011). Gene annotations were derived from the Ensembl database (Ensembl Archive Release 94, October 2018).
Detection of fusion transcripts
Fusion genes were detected using FusionCatcher v099.6a.b (Nicorici et al. 2014). Next, to reduce false positives, we applied a stepwise filtering process and excluded read-through fusions, fusions described as “non-tumor” or “non-cancer-tissue”, fusions that consisted of two adjacent fusion partners (annotated as “distance 1000 bp”, “distance 100 kbp”, “distance 10 kbp”), fusions with ribosomal or mitochondrial genes, fusions that involved immunoglobulin genes, fusions with identical breakpoints in more than three patients, fusions with < 2 spanning pairs and unique reads, pseudogenes and fusions without annotated genes (19). This resulted in the exclusion of 374 (47%) fusion genes with a high likelihood of being false positive (Supplementary Table 1). Another 262 fusions (33%) were removed as they occurred multiple times with the same breakpoints across patients. The remaining 156 events were evaluated in silico for the predicted effect of each fusion. Supplementary Table 2 provides more information about their expected function: 109 fusions (68%) had one gene partner with a non-coding DNA sequence (non-CDS). Nineteen fusions (12%) involved a partner gene with a truncated coding region. Ten fusions (6%) were predicted to be in-frame. Three fusions (2%) were out-of-frame and seven fusions (4%) were either intronic or CDS-complete. The function of eight fusion genes (5%) could not be predicted.
Differential gene expression
Differential gene expression analyses between patient subgroups were performed using DESeq2 (v1.22.2) (Love et al. 2014), while control of type I error in multiple hypothesis testing was done by calculating q value using the q value package (v2.14.1) from R. Gene fusion rearrangements were displayed by Circus plots generated from the copy number package v.1.22.0 as previously described (Krzywinski et al. 2009; Nilsen et al. 2012). Unless otherwise stated, all analyses were performed in R (version 3.5.1).
Statistical analysis
Data are presented as of November 26, 2018. Continuous variables are presented as mean ± standard error of the mean (SEM). Overall survival (OS) was calculated as the time from first diagnosis until death. Progression-free survival (PFS) was calculated as the time from the beginning of study participation to the first observation of progressive disease. Two out of 18 patients could not be evaluated for their PFS as they were removed from the trial due to drug toxicity. Calculations of mean OS and PFS were performed using GraphPad Prism (Version 7.0e, La Jolla, CA, USA). For gene fusion correlation analyses to clinical endpoints, median OS ± 95% confidence interval [CI] was calculated by Kaplan–Meier estimators and tested with log-rank (Mantel–Cox) test using ggplot2 (v.3.1.1) and survival (v. 2.44-1.1) from R. For this purpose, subjects who were still alive or lost to follow-up were included as censored observations. OS and PFS comparisons between groups were calculated by Kaplan–Meier analyses using ggfortify from R (v.0.4.6). For all other two-group comparisons, the Wilcoxon–Mann–Whitney test was used. The Kruskal–Wallis test was applied for the testing between three groups or more. A P value of P < 0.05 was considered to be statistically significant and levels of significance were marked as follows *P < 0.05, **P < 0.01 and ***P < 0.001. Graphical representations of the data are given as boxplots.
Results
TNBC (n = 9) and HGSOC (n = 9) patients were of similar age at diagnosis, ethnicity and BRCA status (Table 1). In the TNBC cohort, four patients had adenocarcinoma and the histological subtypes of the other five TNBC patients could not be further specified. Eight of the HGSOC patients had papillary serous carcinoma and one had transitional carcinoma. A trend was noted toward to early UICC (Union of International Cancer Control) stage tumors in the TNBC subgroup whereas advanced disease stage tumors dominated in the HGSOC subcohort. PFS was measured at a mean of 10.2 ± 1.9 (± SEM) months for TNBC patients and at a mean of 18.2 ± 6.9 (± SEM) months for HGSOC patients. Mean OS was calculated for six TNBC and six HGSOC patients as available at the time of data collection. Mean OS in the TNBC cohort was 5.8 ± 2.4 (± SEM) years and 6.8 ± 0.6 (± SEM) years in the HGSOC subgroup. Intergroup comparison did not reveal a significant difference for PFS (P = 0.23) and OS (P = 0.71) between TNBC and HGSOC patients.
Fusion landscape of TNBC and HGSOC patients
The number of fusion genes in the entire cohort ranged from 0 and 21 per patient, with a mean of 8.7 ± 1.9 (± SEM) (Table 2). No fusion event was detected in three out of nine (33%) TNBC patients [mean 8.2 ± 2.6 (± SEM)] and two out of nine (22%) HGSOC patients [mean 9.1 ± 2.9 (± SEM)]. There was no difference in the number of fusion transcripts between TNBC and HGSOC patients (Fig. 1a, P = 0.62) and no association between the number of fusions and (1) age (P = 0.63), (2) UICC stage (P = 0.95), (3) clinical grade (P = 0.86) or (4) BRCA mutation status (P = 0.28, Supplementary Fig. 1).
Fusion landscape across TNBC and HGSOC. Box plots were used to illustrate the number of fusions per patient. No significant difference between TNBC and HGSOC patients was noted for the number of total fusions (a Mann–Whitney–Wilcoxon P = 0.62) and the number of recurrent fusions (b Mann–Whitney–Wilcoxon P = 0.5)
Only a fraction of fusion genes is recurrent
Among the 156 fusion genes, 44 (28%) events were confirmed to be recurrent in at least two patients (Table 3). This accounted for a mean of 2.4 ± 0.5 (± SEM, range 0–8) recurrent fusion events per patient. In total, 20 different recurrent fusion genes were observed. In the TNBC subgroup, a frequency of 36% (27/74 events) recurrent fusion events was detected with a mean of 3.0 ± 0.9 (± SEM, range 0–8) per patient. This compared to a lower rate of 21% recurrent fusion genes (17/82 events) in the HGSOC subgroup with a mean of 1.9 ± 0.5 (± SEM 0–4) per patient (Table 3). Intergroup comparison was not statistically significant (P = 0.5, Fig. 1b). Eleven of 20 (55%) recurrent fusion events were shared between TNBC and HGSOC patients (Fig. 2). Six fusion events were only detected in TNBC patients (SPTAN1–MALAT1, RNF213–MALAT1, MALAT1–WWOX, MALAT1–FOXP1, MALAT1–DST, ATXN3–THAP11), while three fusion genes were uniquely observed in HGSOC patients, only (OGT–MUC16, NCL–MUC16, MUC16–NCL, Fig. 2). Four fusion events (WWOX–MALAT1, THAP11–ATXN3, SMG1–MALAT1, MALAT1–VPS13B) occured in a total of three different patients each.
Frequency of the most prevalent recurrent fusion gene combinations across TNBC and HGSOC. Bar plots illustrating the most prevalent recurrent fusion gene combinations across both diseases. The gene location on its respective chromosome is given in brackets. MALAT1 was involved in the majority of fusion transcripts. Three fusions genes involving MUC16 were detected in more than one patient but were exclusively limited to HGSOC patients and were absent in TNBC patients. Eleven out of 20 (55%) of the most common fusion combinations could be observed in TNBC as well as HGSOC patients. FOXP1 was detected as a partner gene in two recurrent combinations with MALAT1 (2/20, 10%) and was additionally observed in two additional fusions. The frequency of all partner genes in recurrent and unique gene fusions is given in Supplementary Table 3
MALAT1, MUC16, FOXP1, WWOX and XIST are the most common genes partnering in gene fusions
We next examined our dataset to look for genes repeatedly involved in gene fusions. Among the five most frequently detected genes, the long non-coding RNA (lncRNA) MALAT1 was involved in 62% (97/156 events, 13 different individuals) of fusion transcripts, followed by the protein-coding mucin family gene MUC16 (12%, 19/156 events, three different individuals) and FOXP1 coding for the tumor suppressor and forkhead box transcription factor protein 1 (4%, 6/156 events, five different individuals). The tumor suppressor gene WWOX and the non-protein-coding X inactive-specific transcript (XIST) were detected in 6/156 (4%) events and four different individuals each. Table 4 illustrates the frequency of MALAT1, MUC16, FOXP1, WWOX and XIST across TNBC and HGSOC patients. A detailed overview of all detected fusion gene partners and their frequency is given in Supplementary Table 3.
MALAT1 was detected as partner gene in both subgroups but was more prevalent in TNBC (57%) as compared to HGSOC patients (43%). Fusion genes involving MUC16 were exclusively observed in HGSOC patients accounting for 22% (19/82 events) of all fusion transcripts detected in the HGSOC subgroup. Similar to MALAT1, FOXP1 was detected as a partner gene in both subgroups, noting a higher prevalence in the TNBC subgroup (83% of all FOXP1 fusion events). WWOX and XIST fusions were both identified in two TNBC and two HGSOC patients (Fig. 4).
Circos plots were used to illustrate and compare gene fusion combinations that were recurrently shared in TNBC and HGSOC patients (Fig. 3a) as compared to TBNC (Fig. 3b) and HGSOC (Fig. 3c) patients, only. MALAT1 (chr 11) was highly promiscuous and formed recurrent fusions with numerous partner genes from a number of chromosomes, including chromosomes 6, 8, 9, 14, 16, 17, and FOXP1 on chromosome 3 (Fig. 3b). In HGSOC, the fusion landscape was dominated by MUC16 on chromosome 19 which partnered with genes on nearby partner chromosomes (chr X and 2: Fig. 3c).
Distribution of fusion genes across the genome. Circos plots illustrating all recurrent fusion rearrangements in all patients (an = 18), in TNBC patients (bn = 9) and HGSOC patients, only (cn = 9). The predominance of fusion genes involving chromosome 11 was attributable to fusion transcripts involving the lncRNAs MALAT1 located on this chromosome. MALAT1 (chromosome 11) was highly promiscuous and formed recurrent fusions with numerous partner genes from a number of chromosomes, thereby resulting in a highly complex chromosomal distribution in TNBC patients. The chromosomal distribution for HGSOC was less abundant than that for TNBC and was mostly limited to chromosome 19 (MUC16) and nearby partner chromosomes (chr X, 2). Similar to MALAT1, FOXP1 was detected as a partner gene in recurrent fusion genes in both subgroups, noting a higher prevalence in the TNBC subgroup (83% of all FOXP1 fusion events)
Differential gene expression in three fusion gene partners
Upregulation of ABL1 gene expression is a common feature of BCR–ABL1-positive versus -negative acute lymphoblastic leukemia (Juric et al. 2007). Following this trajectory, we aimed to determine whether gene fusions in our dataset would also result in differential expression of the respective genes involved. A total of 20 recurrent fusion genes were detected. One of these partner genes (C19MC) was not annotated and thus excluded from the analysis.
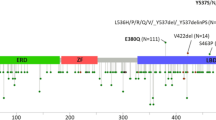
For the remaining 19 recurrent fusion partner genes, we performed differential gene expression analysis for fusion-positive versus -negative patients using DESeq2. Gene expression was significantly different in the three genes FOXP1 (P = 0.02), MUC16 (P = 0.02) and DST (P = 0.02) (Fig. 4, Table 5).
Differential gene expression in fusion partner genes. Scatter plot examining differential gene expression results from transcriptome analysis by DESeq2 in fusion-positive as compared to fusion-negative patients. A total of 20 genes were detected as recurrent fusion gene partners across our cohort. One fusion partner (C19MC) was not annotated and thus excluded from the analysis. Normalization of counts was performed separately for every gene for the combined cohort of TNBC and HGSOC patients (n = 18). MALAT1 showed no significantly altered expression in patients who carried a fusion transcript with the respective gene involved vs. those without (P value = 0.29), whereas significant overexpression of FOXP1 (P = 0.02), MUC16 (P = 0.02) and DST (P = 0.02) was noted in patients with the respective fusion transcript as compared to controls
Interestingly, although MALAT1 was the most common partner gene, its expression was not significantly altered in tumors with and without fusions (P = 0.29). Similarly, expression of WWOX (P = 0.21) and XIST (P = 0.42) was not significantly different in tumors with versus without involvement of the respective fusion gene.
Patients with FOXP1 fusion genes show significant FOXP1 overexpression and are associated with favorable overall survival
By performing differential gene expression analysis, we were able to demonstrate a functional impact of MUC16, DST and FOXP1 fusions on the expression of the respective gene. In a final step, we examined the clinical variables associated with these transcripts.
MUC16 codes for CA-125, an established serum marker for ovarian cancer in the clinic (Panza et al. 1988). In our cohort, MUC16 fusion transcripts were exclusively detected in HGSOC patients. Since MUC16 fusion genes could thus not provide a shared value for our entire study cohort, this gene was excluded from further correlation analyses. Similarly, fusion genes involving DST were deprioritized given the low frequency of DST fusion genes of only 2/18 (11%) patients which did not allow for relevant association with clinical endpoints.
Consequently, we focussed on the clinical comparison analysis of FOXP1 fusion genes for which differential gene expression was the most significant in patients with versus without a respective fusion (Fig. 5a, P = 0.02).
Correlation of FOXP1 fusion genes with gene expression and overall survival. Box plots illustrating the expression level of FOXP1 in TNBC and HGSOC patients with vs. without identified FOXP1 fusion genes. Significant overexpression was noted when FOXP1 was involved in a fusion gene (aP = 0.02). Kaplan–Meier estimators were calculated to evaluate the overall survival (OS, years) in patients with as compared to patients without FOXP1 fusion (b). For the calculation of OS, all patients alive at the time of this study were included as censored subjects. Patients lost to follow-up were censored at the last day confirmed alive. Superior survival was observed in fusion-positive patients. Given the small sample size of the here-presented study, this finding did not reach statistical significance (Mann–Whitney–Wilcoxon P = 0.08)
To estimate the prognostic impact of FOXP1 fusion transcripts on the outcome of TNBC and HGSOC patients, we performed Kaplan–Meier estimators for FOXP1 fusion-negative versus -positive patients. Median PFS on buparlisib/olaparib treatment was 12.1 months (95% CI 0.3–2.6) for patients with FOXP1 fusions as compared to 13.9 months (95% CI 0.4–3.4) in those without (P = 0.97, Supplementary Fig. 2). This lack of significance was expected since no direct association between the FOXP1 tumor suppressor gene and PI3K/PARP inhibition has been reported thus far. In a next step, we performed Kaplan–Meier estimators to determine whether FOXP1 fusions were associated with a difference in OS. Median OS in FOXP1 fusion-positive patients was 17.2 years (95% CI 0.8–10.2) as compared to a median OS of 6.2 years (95% CI 0.1–1.3) in FOXP1 fusion-negative patients (Fig. 5b). As inherent to the small sample size of this study, this OS difference was not significant (P = 0.08) and interpretations need to remain exploratory.
Discussion
In this study, transcriptome sequencing was applied to identify gene fusions in a cohort of 18 TNBC and HGSOC patients. Fusion events were detected by the use of the FusionCatcher algorithm, a tool validated to confirm true-positive gene fusions with reported filtering rates of ~ 40% (Nicorici et al. 2014; Engqvist et al. 2018; Parris et al. 2018). To further minimize the number of false-positive events in our analysis, we applied additional filtering steps. In total, this resulted in a number of 156/792 (20%) fusions which were kept for further exploration. This number compares to a similar filtering strategy reported in a 2018 study by Fimereli and colleagues, which reported a fraction of 316/1222 (26%) true fusion events identified by the deFuse algorithm with Ensemble release 62 (reference genome hg19, 22).
The mean number of fusion transcripts per patient in our study was reported at 8.7 ± 1.9 (± SEM). The prevalence of fusion genes was not significantly different between both tumor types (P = 0.62). Previous reports using FusionCatcher have reported a mean rate of 132.7 ± 31.0 (± SEM, range 12–613) and 34.7 ± 4.4 (± SEM, range 0–266) fusion events per sample in breast and ovarian cancers, respectively (Engqvist et al. 2018; Parris et al. 2018). It must be noted that the cohorts in those studies were not exclusively restricted to TNBC and HGSOC and are thus not entirely comparable to our analysis. Similarly, Fimereli and colleagues did not preselect their breast cancer cohort for TNBC patients and observed that the number of fusion genes per sample ranged between 0 and 31 with a mean of 6.7 fusion genes, noting the highest prevalence in HER2-positive tumors, which were not part of our study (Fimereli et al. 2018).
Overall, 109/156 (68%) fusion genes in our study had one gene partner with a non-CDS, but only 7/156 (4%) were confirmed to be CDS-complete. Engqvist and colleagues recently reported a comparable rate of 76% non-CDS fusion genes in a cohort of 96 early-stage ovarian cancer patients (Engqvist et al. 2018). A similar rate of 86% non-CDS fusion genes has been reported by Parris and colleagues for a cohort of 185 breast cancer patients (Parris et al. 2018). Our data thus suggest that non-CDS fusion gene partners seem to be similarly prevalent in TNBC and HGSOC as previously confirmed for the aforementioned unselected populations of breast and ovarian cancers.
It has been described that the rate of recurrent fusion genes in breast and ovarian cancers is low and may be even more limited in tumors with high genomic instability (Mertens et al. 2015; Yoshihara et al. 2015). Correspondingly, only 44/156 (28%) fusion genes in our cohort were detected in more than two patients. None of these fusion genes have been previously detected in the TCGA cohort for breast and ovarian cancers (Yoshihara et al. 2015). At the same time, 59/88 (67%) of the individual genes we identified had also been reported by Yoshihara and colleagues in their extensive interrogation of 4366 tumor samples (Yoshihara et al. 2015). Our analysis thus supports prior studies indicating that the majority of gene fusions in epithelial cancers are most likely private passenger events with low recurrence across samples (Mertens et al. 2015).
The majority of fusion genes in our study involved at least one partner gene located on chromosome 11. Such chromosomal hotspots for fusion genes have been reported. The study by Fimereli and colleagues has observed fusion hotspots in breast cancer on chromosomes 17, 8 and 20 (Fimereli et al. 2018). Similar to our observation, the majority of fusion transcripts in the studies by Engqvist et al. (2018) and Parris et al. (2018) equally involved chromosome 11 as predominant fusion hotspot. This striking relationship was mostly attributable to fusion transcripts involving the lncRNA MALAT1 located on chromosome 11.
Long non-coding RNAs are defined by having a length exceeding 200 nucleotides (Mendell 2016). The human genome encodes many thousands of these lncRNAs but their role in cancer remains to be comprehensively characterized. MALAT1 was one of the first human lncRNAs to be discovered in samples of metastatic lung cancer cells (Ji et al. 2003). Since then, it has been shown to be associated with metastasis and poor survival in multiple malignancies including breast cancer (Gutschner et al. 2013). Its exact molecular function, however, still remains poorly understood. MALAT1 fusion genes were previously detected in breast cancer and ovarian cancer samples (Engqvist et al. 2018; Parris et al. 2018). In these samples, MALAT1 was determined to be highly promiscuous with over 400 partner genes, indicating that the majority of MALAT1 fusions may occur at the RNA level (Parris et al. 2018).
In our cohort, MALAT1 was involved in 97/156 (62%) fusion genes and partnered with 68 different gene partners. 55/74 (74%) fusion genes in TNBC and 42/82 (51%) fusion genes in HGSOC involved MALAT1 as one of their partnering genes. Overall, MALAT1 fusions were detectable in six TNBC and seven HGSOC patients. Since lncRNAs do not generate a corresponding fusion protein but may influence the expression of the respective fusion partner, further research is necessary to elucidate their role for tumor formation.
The expression of partner genes involved in gene fusions may be substantially altered once fused to a partner gene with promoter activity (Juric et al. 2007). To examine how fusion genes affected differential gene expression of both partner genes in our cohort, we next performed differential gene expression analysis for the 19 most common fusion partner genes in our cohort. Among these, FOXP1, MUC16 and DST showed a significantly altered expression in those patients who carried a respective fusion transcript as compared to those without. Notably, and in contrast to prior reports in ovarian cancer, no such relationship was observed for MALAT1 (Engqvist et al. 2018).
MUC16 is a mucin family gene that codes for Cancer Antigen 125 (CA-125). CA-125 has been used to monitor ovarian cancer in the clinic for many years (NIH consensus conference 1995). Expectedly, MUC16 was determined to be a frequent driver fusion transcript in the ovarian cancer study by Engqvist and colleagues (Engqvist et al. 2018) and was similarly prevalent in 3/9 (33%) of HGSOC patients in our cohort.
The most notable candidate gene in our study, however, FOXP1, was involved in fusion genes of a total of four TNBC patients (one case with two detectable FOXP1 fusion genes) and one HGSOC patient. The presence of FOXP1 fusion genes corresponded to a significant overexpression of FOXP1. Correlation studies with clinical endpoints need to remain exploratory, mostly since only one HGSOC patient was tested positive for carrying a FOXP1 fusion gene. However, the median OS in FOXP1 fusion positive patients was 17.2 years as compared to a median OS of 6.2 years in FOXP1 fusion negative patients (P = 0.08). The potential role of FOXP1 as a prognostic marker in oncology remains controversial. High FOXP1 expression has previously been linked to metastasis and poor five-year OS in a cohort of 101 non-small cell lung cancer patients (Feng et al. 2012). At the same time, other studies have reported an association between FOXP1 overexpression and inferior outcome in the context of hematologic malignancies such as follicular lymphoma and diffuse-large B-cell lymphoma (Mottok et al. 2018; Barrans et al. 2004).
Our observation may be in line with previous studies in breast cancer that observed high FOXP1 protein expression to be a favorable prognostic marker in patients with estrogen receptor (ER)-positive breast cancer (Bates et al. 2008; Fox et al. 2004; Rayoo et al. 2009). Our analysis expands the scope of these latter studies by investigating the presence of FOXP1 fusion genes in TNBC and HGSOC. Notably, as 83% of the identified FOXP1 fusion genes in our cohort have been detected in TNBC patients, we conclude that FOXP1 may act as a tumor suppressor independently of ER expression. The correlation detected in this study should be treated with caution given the small sample size inherent to a phase I study. Similarly, the comparison between fusion-positive (n = 5) and fusion-negative (n = 13) patients was not balanced in numbers and thus biased for a greater variation (P = 0.02). More comprehensive analyses will be needed to confirm the prognostic value of FOXP1 fusion genes.
The limited sample size in our study remains an inevitable shortcoming of this analysis. Tumor tissue from initial diagnosis was only available for 18/69 patients of the entire study cohort meaning that our analysis might not have been powered to detect significant differences. It must also be noted that, despite its merits and meticulous filtering, RNA-seq may not detect some fusion genes including those involving non-transcribed enhancer or promoter elements (Kim and Salzberg 2011). Future approaches will thus have to complement transcriptome analysis by whole-genome-sequencing and RT-PCR.
In summary, our analysis provides the first comprehensive analysis of the fusion gene landscape in a homogeneously treated cohort of TNBC and HGSOC patients. We provide evidence for the low frequency of recurrent fusion genes in both cancer types. The lncRNA MALAT1 was a highly prevalent fusion partner in our analysis, but larger studies will have to further determine its potential as prognostic biomarker in TNBC and HGSOC. Interestingly, three fusion gene partners showed a significantly altered expression in patients carrying the respective fusion. Among these, FOXP1 fusions seem to be associated with a favorable prognosis in TNBC and HGSOC patients. Such observations may help to increase our understanding on the role of fusion genes in female cancer. This seems particularly relevant for cancers with limited treatment options such as TNBC and HGSOC, for which a better mechanistic understanding of how fusion genes interfere with functional gene expression may provide vital clues to finding new and innovative therapeutic strategies.
References
American Cancer Society (2019a) Cancer facts and figures 2019. Key statistics for breast cancer. American Cancer Society, Atlanta, GA. https://www.cancer.org/content/cancer/en/cancer/breast-cancer/about/how-common-is-breast-cancer/#references
American Cancer Society (2019b) Cancer facts and figures 2019. Key statistics for ovarian cancer. American Cancer Society. Atlanta, GA. https://www.cancer.org/cancer/ovarian-cancer/about/key-statistics.html
Barrans SL, Fenton JAL, Banham A, Owen RG, Jack AS (2004) Strong expression of FOXP1 identifies a distinct subset of diffuse large B-cell lymphoma (DLBCL) patients with poor outcome. Blood 104:2933–2935
Bates GJ, Fox SB, Han C, Launchbury R, Leek RD, Harris AL, Banham AH (2008) Expression of the forkhead transcription factor FOXP1 is associated with that of estrogen receptor-beta in primary invasive breast carcinomas. Breast Cancer Res Treat 111:453–459
Bell D, Berchuck A, Birrer M et al. (2011) Integrated genomic analyses of ovarian carcinoma. Nature 474:609–615. https://doi.org/10.1038/nature10166
Cancer Genome Atlas Network (2012) Comprehensive molecular portraits of human breast tumours. Nature 490:61–70
Dobin A, Davis CA, Schlesinger F, Drenkow J, Zaleski C, Jha S, Batut P, Chaisson M, Gingeras TR (2013) STAR: ultrafast universal RNA-seq aligner. Bioinformatics 29:15–21
Engqvist H, Parris TZ, Rönnerman EW, Söderberg EMV, Biermann J, Mateoiu C, Sundfeldt K, Kovács A, Karlsson P, Helou K (2018) Transcriptomic and genomic profiling of early-stage ovarian carcinomas associated with histotype and overall survival. Oncotarget 9:35162–35180
Feng J, Zhang X, Zhu H, Wang X, Ni S, Huang J (2012) High expression of FoxP1 is associated with improved survival in patients with non-small cell lung cancer. Am J Clin Pathol 138:230–235
Fimereli D, Fumagalli D, Brown D, Gacquer D, Rothé F, Salgado R, Larsimont D, Sotiriou C, Detours V (2018) Genomic hotspots but few recurrent fusion genes in breast cancer. Genes Chromosom Cancer 57:331–338
Foulkes WD, Smith IE, Reis-Filho JS (2010) Triple-negative breast cancer. N Engl J Med 363:1938–1948
Fox SB, Brown P, Han C, Ashe S, Leek RD, Harris AL, Banham AH (2004) Expression of the forkhead transcription factor FOXP1 is associated with estrogen receptor alpha and improved survival in primary human breast carcinomas. Clin Cancer Res 10:3521–3527
Gutschner T, Hämmerle M, Diederichs S (2013) MALAT1—a paradigm for long noncoding RNA function in cancer. J Mol Med 91:791–801
Hu H, Juvekar A, Lyssiotis CA, Lien EC, Albeck JG, Oh D, Varma G, Hung YP, Ullas S, Lauring J, Seth P, Lundquist MR, Tolan DR, Grant AK, Needleman DJ, Asara JM, Cantley LC, Wulf GM (2016) Phosphoinositide 3-kinase regulates glycolysis through mobilization of aldolase from the actin cytoskeleton. Cell 164:433–446
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ (2009) Cancer statistics. CA Cancer J Clin 59:225–249
Ji P, Diederichs S, Wang W, Böing S, Metzger R, Schneider PM, Tidow N, Brandt B, Buerger H, Bulk E, Thomas M, Berdel WE, Serve H, Müller-Tidow C (2003) MALAT-1, a novel noncoding RNA, and thymosin beta4 predict metastasis and survival in early-stage non-small cell lung cancer. Oncogene 22:8031–8041
Juric D, Lacayo NJ, Ramsey MC, Racevskis J, Wiernik PH, Rowe JM, Goldstone AH, O’Dwyer PJ, Paietta E, Sikic BI (2007) Differential gene expression patterns and interaction networks in BCR-ABL-positive and -negative adult acute lymphoblastic leukemias. J Clin Oncol 25:1341–1349
Juvekar A, Burga LN, Hu H, Lunsford EP, Ibrahim YH, Balmañà J, Rajendran A, Papa A, Spencer K, Lyssiotis CA, Nardella C, Pandolfi PP, Baselga J, Scully R, Asara JM, Cantley LC, Wulf GM (2012) Combining a PI3K inhibitor with a PARP inhibitor provides an effective therapy for BRCA1-related breast cancer. Cancer Discov 2:1048–1063
Kim D, Salzberg SL (2011) TopHat-fusion: an algorithm for discovery of novel fusion transcripts. Genome Biol 12:R72
Koonings PP, Campbell K, Mishell DR, Grimes DA (1989) Relative frequency of primary ovarian neoplasms: a 10-year review. Obstet Gynecol 74:921–926
Krzywinski M, Schein J, Birol I, Connors J, Gascoyne R, Horsman D, Jones SJ, Marra MA (2009) Circos: an information aesthetic for comparative genomics. Genome Res 19:1639–1645
Li B, Dewey CN (2011) RSEM: accurate transcript quantification from RNA-Seq data with or without a reference genome. BMC Bioinform 12:323
Love MI, Huber W, Anders S (2014) Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol 15:550
Matulonis UA, Wulf GM, Barry WT, Birrer M, Westin SN, Farooq S, Bell-McGuinn KM, Obermayer E, Whalen C, Spagnoletti T, Luo W, Liu H, Hok RC, Aghajanian C, Solit DB, Mills GB, Taylor BS, Won H, Berger MF, Palakurthi S et al (2017) Phase I dose escalation study of the PI3kinase pathway inhibitor BKM120 and the oral poly (ADP ribose) polymerase (PARP) inhibitor olaparib for the treatment of high-grade serous ovarian and breast cancer. Ann Oncol 28:512–518
Mendell JT (2016) Targeting a long noncoding RNA in breast cancer. N Engl J Med 374:2287–2289
Mertens F, Johansson B, Fioretos T, Mitelman F (2015) The emerging complexity of gene fusions in cancer. Nat Rev Cancer 15:371–381
Mottok A, Jurinovic V, Farinha P, Rosenwald A, Leich E, Ott G, Horn H, Klapper W, Boesl M, Hiddemann W, Steidl C, Connors JM, Sehn LH, Gascoyne RD, Hoster E, Weigert O, Kridel R (2018) FOXP1 expression is a prognostic biomarker in follicular lymphoma treated with rituximab and chemotherapy. Blood 131:226–235
Nicorici D, Satalan M, Edgren H, Kangaspeska S, Murumagi A, Kallioniemi O, Virtanen S, Kilkku O (2014) FusionCatcher—a tool for finding somatic fusion genes in paired-end RNA-sequencing data, bioRxiv. https://doi.org/10.1101/011650
NIH consensus conference (1995) Ovarian cancer. Screening, treatment, and follow-up. NIH Consensus Development Panel on Ovarian Cancer. JAMA 273:491–497
Nilsen G, Liestøl K, Van Loo P, Moen Vollan HK, Eide MB, Rueda OM, Chin S-F, Russell R, Baumbusch LO, Caldas C, Børresen-Dale A-L, Lingjaerde OC (2012) Copynumber: efficient algorithms for single- and multi-track copy number segmentation. BMC Genom 13:591
Owen LA, Kowalewski AA, Lessnick SL (2008) EWS/FLI mediates transcriptional repression via NKX2.2 during oncogenic transformation in Ewing’s sarcoma. PLoS One 3:1965
Panza N, Pacilio G, Campanella L, Peluso G, Battista C, Amoriello A, Utech W, Vacca C, Lombardi G (1988) Cancer antigen 125, tissue polypeptide antigen, carcinoembryonic antigen, and beta-chain human chorionic gonadotropin as serum markers of epithelial ovarian carcinoma. Cancer 61:76–83
Parris TZ, Rönnerman EW, Engqvist H, Biermann J, Truvé K, Nemes S, Forssell-Aronsson E, Solinas G, Kovács A, Karlsson P, Helou K (2018) Genome-wide multi-omics profiling of the 8p11-p12 amplicon in breast carcinoma. Oncotarget 9:24140–24154
Rayoo M, Yan M, Takano EA, Bates GJ, Brown PJ, Banham AH, Fox SB (2009) Expression of the forkhead box transcription factor FOXP1 is associated with oestrogen receptor alpha, oestrogen receptor beta and improved survival in familial breast cancers. J Clin Pathol 62:896–902
Roy L, Guilhot J, Krahnke T, Guerci-Bresler A, Druker BJ, Larson RA, O’Brien S, So C, Massimini G, Guilhot F (2006) Survival advantage from imatinib compared with the combination interferon-alpha plus cytarabine in chronic-phase chronic myelogenous leukemia: historical comparison between two phase 3 trials. Blood 108:1478–1484
Soda M, Choi YL, Enomoto M, Takada S, Yamashita Y, Ishikawa S, Fujiwara S, Watanabe H, Kurashina K, Hatanaka H, Bando M, Ohno S, Ishikawa Y, Aburatani H, Niki T, Sohara Y, Sugiyama Y, Mano H (2007) Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature 448:561–566
Tognon C, Knezevich SR, Huntsman D, Roskelley CD, Melnyk N, Mathers JA, Becker L, Carneiro F, MacPherson N, Horsman D, Poremba C, Sorensen PHB (2002) Expression of the ETV6-NTRK3 gene fusion as a primary event in human secretory breast carcinoma. Cancer Cell 2:367–376
Tomlins SA, Rhodes DR, Perner S, Dhanasekaran SM, Mehra R, Sun X-W, Varambally S, Cao X, Tchinda J, Kuefer R, Lee C, Montie JE, Shah RB, Pienta KJ, Rubin MA, Chinnaiyan AM (2005) Recurrent fusion of TMPRSS2 and ETS transcription factor genes in prostate cancer. Science 310:644–648
Yoshihara K, Wang Q, Torres-Garcia W, Zheng S, Vegesna R, Kim H, Verhaak RGW (2015) The landscape and therapeutic relevance of cancer-associated transcript fusions. Oncogene 34:4845–4854
Funding
JE is supported by a postdoctoral fellowship of Deutsche Krebshilfe (German Cancer Aid). JMW is supported by a postdoctoral fellowship of Deutsche Forschungsgemeinschaft (German Research Foundation). SN is supported by the National Institutes of Health under Award Number R00LM011595. GMW is supported by the Breast Cancer Research Foundation (BCRF), the Mary Kay Ash Foundation, the Breast Cancer Alliance, the Men’s Initiative of the Dana-Farber Harvard Cancer Center (DFHCC), a Stand Up to Cancer Dream Team Translational Research Grant and a Program of the Entertainment Industry Foundation (SU2C-AACR-DT0209).
Author information
Authors and Affiliations
Contributions
JE, YJH, JMW, ISV and GMW conceived and designed the study. JE, SN and GMW collected the RNA-seq data. JE, YJH, JMW, ISV and CJM conducted the bioinformatics processing and analysis. GMW, KG, UAM and PAK provided the clinical data. All authors participated in interpreting the data and writing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
PAK reports personal fees from Astra Zeneca, Merck, Pfizer, Tesaro and Bayer, outside the submitted work. UAM reports personal fees from Astra Zeneca, Myriad Genetics, Clovis, Merck, Eli Lilly, Mersana, Geneos, Fuji Film, 2X Oncology, Cerulean, Immunogen and Novartis, outside the submitted work. GMW reports grants from SU2C-AACRDT0209, Mary Kay Ash Fundation, Ovarian Cancer Research Foundation, Breast Cancer Alliance, Breast Cancer Research Foundation, NIH RO1 1R01CA226776-01 and Merck, during the conduct of the study. In addition, GMW has a patent application 14/348810, Compositions and Methods for the Treatment of proliferative diseases pending, and a patent US 20090258352 A1, Pin1 as a marker for abnormal cell growth licensed to Cell Signaling; R&D Systems. All other authors declare no conflicts.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical approval
All procedures performed in this study were performed in accordance with the Declaration of Helsinki and the International Conference on Harmonization Good Clinical Practice. All patients provided written informed consent to allow the use of available biopsies for the analysis and research purposes of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Eismann, J., Heng, Y.J., Waldschmidt, J.M. et al. Transcriptome analysis reveals overlap in fusion genes in a phase I clinical cohort of TNBC and HGSOC patients treated with buparlisib and olaparib. J Cancer Res Clin Oncol 146, 503–514 (2020). https://doi.org/10.1007/s00432-019-03078-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-019-03078-9