Abstract
Purpose
The aim of this study was to characterize the patterns of recurrence in patients achieving pathologic complete response (pCR) after neoadjuvant chemoradiotherapy (CRT) for locally advanced rectal cancer.
Methods
Patients with locally advanced rectal cancer treated with neoadjuvant CRT and who achieved pCR from January 2004 to December 2012 were collected. The primary outcome measurement was the patterns of recurrence.
Results
Among 195 patients who achieved pCR, 18 developed recurrence. Furthermore, local recurrence occurred in 1.5% of patients (3/195), while distant metastases occurred in 7.7% of patients (15/195), which included 7 lung metastases, 1 liver metastasis, and 8 metastases in other locations.
Conclusions
Our study indicated that patients achieving pCR following neoadjuvant CRT have a favorable prognosis, with distant metastases predominating in all recurrences. Among patients with distant metastases, non-liver metastases were the predominant pattern.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Preoperative chemoradiotherapy (CRT) has been used as the standard management strategy for locally advanced rectal cancer over the past decade (Sebag-Montefiore et al. 2009; Roh et al. 2009; Sauer et al. 2004), improving the outcome of locally advanced rectal cancer (Maas et al. 2010; Rodel et al. 2005; Garcia-Aguilar et al. 2003). Treatment response to neoadjuvant CRT is linked with oncologic outcomes (Park et al. 2012). Fifteen to twenty percent of patients with locally advanced rectal cancer might achieve pathologic complete response (pCR) after neoadjuvant CRT, which is associated with favorable long-term outcome (Park et al. 2012; Campos-Lobato et al. 2011; Smith et al. 2010).
Studies reporting the patterns of recurrence in patients achieving pCR after neoadjuvant CRT are very limited. In this study, we investigated the patterns of recurrence in this subgroup of patients.
Patients and methods
We retrospectively reviewed patients with locally advanced rectal cancer treated with preoperative CRT followed by radical resection at the Sun Yat-Sen University Cancer Center and the Sixth Affiliated Hospital of Sun Yat-Sen University between January 2004 and December 2012. Patients who achieved pCR after CRT and those who developed recurrence were enrolled in the study.
Tumors were staged according to the American Joint Committee on Cancer (AJCC) Cancer Staging Manual (Edge and Compton 2010). We defined pCR as absence of viable adenocarcinoma cells in the surgical specimen (ypT0N0). Local and distant recurrence was defined as relapse within and outside the pelvis, respectively. Time to diagnosis was defined as the time between any initial abnormal findings on follow-up examination to clinical or histological confirmation of recurrence.
Pre-treatment staging, tumor location, details of neoadjuvant and adjuvant therapy, interval to surgery, type of surgery, number of lymph nodes (LNs) retrieved, site(s) of recurrence, and salvage treatment were extracted from medical records.
We excluded patients who were diagnosed with a non-skin cancer within 5 years of the rectal cancer diagnosis, did not complete neoadjuvant CRT, and who did not undergo radical rectal resection.
Pre-treatment evaluation included digital rectal examination, chest and abdominal computed tomography (CT) scans, and endoscopic ultrasound and/or magnetic resonance imaging (MRI) of the pelvis. Prior to treatment, the pathologists of each hospital confirmed that all enrolled patients had adenocarcinoma of the rectum. Patients were treated with CRT that involved radiotherapy and fluorouracil (FU)-based chemotherapy. Surgery was generally performed 4–10 weeks following completion of CRT according to total mesorectal excision (TME) principles.
Patients were followed-up every 3 months for 2 years, every 6 months for the next 3 years, and annually thereafter. Evaluations consisted of physical examination, serum carcinoembryonic antigen levels, abdominal ultrasound, and chest radiography. Liver ultrasonography was carried out every 3 months. Chest, abdominal, and pelvic CT scans were performed every year for 5 years. Other investigations were performed when clinically indicated during follow-up.
Results
Our retrospective review determined that 771 patients with locally advanced adenocarcinoma of the rectum had undergone CRT followed by TME at the Sun Yat-Sen University Cancer Center and the Sixth Affiliated Hospital of Sun Yat-Sen University between January 2004 and December 2012. Twelve patients were excluded due to concurrent distant metastasis, concurrent malignancy, or prior history of pelvic radiotherapy. An eventual 195 patients with ypT0N0 pathology (i.e., achieved pCR) were enrolled in the present study; 18 developed recurrence. The characteristics of these 18 patients are summarized in Table 1.
Three patients developed lateral pelvic sidewall recurrence. All recurrence occurred in the lower rectum (within 5 cm from the anal verge), and pre-treatment CT scan detected lateral LN metastasis (Fig. 1). After preoperative CRT, the metastatic LN was decreased to 2 mm. Standard TME was performed without lateral pelvic LN dissection (LPLD). However, there was recurrence in the lateral pelvic LN (LPLN), where recurrence occurred in 2 and 1 patient within 1 and 3 years, respectively, from the time of surgery. Only one patient underwent examination for 12 LN.
Lateral pelvic recurrence on computed tomography. a Pre-treatment image shows a 5-mm lymph node in the right obturator area (white arrow). b Patient underwent neoadjuvant chemoradiotherapy and the metastatic lymph node was decreased to 2 mm (white arrow). c Follow-up image at 12 months after surgery shows lateral pelvic recurrence (white arrow).
Distant metastases occurred in 7.7% of patients (15/195; median time to relapse: 14 months), including 7 lung metastases, 1 liver metastasis, and 8 metastases in other locations. In all but 2 patients, recurrence was 5 cm below the anal verge, and the median number of examined LN was 9 (range: 0–18). Four of seven lung metastases and one liver metastasis were histological confirmed. None of the patients had both local and distant recurrence.
Discussion
Following the introduction of TME and CRT, local failure rates after curative (R0) resection of locally advanced rectal cancer have decreased dramatically (Sauer et al. 2004; Collette et al. 2007; Wibe et al. 2002). Previous studies have consistently demonstrated that patients with good response after CRT have better long-term outcomes (Garcia-Aguilar et al. 2003; Park et al. 2012).
The AJCC and International Union Against Cancer recommend retrieving a minimum 12 LN to achieve appropriate staging. However, several studies have reported lower LN yield in proctectomy specimens from patients treated with preoperative CRT (Fuente et al. 2009; Marks et al. 2010; Govindarajan et al. 2011). In the present study, we retrieved much fewer LN (median number of examined LN: 8, range: 0–18) than previous reports of patients treated with neoadjuvant CRT. As has been previously reported, the number of LN harvested varies greatly even when surgical treatment and pathological evaluation have been standardized (Marks et al. 2010). At our hospitals, all colorectal surgeons involved in this study had received formal training in TME, thus all patients in this group underwent surgical treatment involving adequate TME proctectomy. The inadequate LN sampling may suggest incomplete TME, which might result in adverse oncological outcome. However, some researchers were unable to identify any relationship between the reduced numbers of LNs examined and decreased patient survival (Rullier et al. 2008; Ha et al. 2010). Moreover, a study by the Cleveland Clinic not only confirmed the association between neoadjuvant therapy and decreased number of LNs retrieved from proctectomy specimens, but also suggested that the diminished number of LNs is actually an indicator of improved tumor response and consequently decreased local recurrence rates (Campos-Lobato et al. 2013).
LPLN metastasis is another reason for the local recurrence in our data. In the present study, the failure pattern of the three cases raises the question of whether LPLD should be performed in patients with suspected LPLN metastasis based on pre-CRT CT or MRI, and how patients who may benefit from LPLD can be identified. Studies from Japan have demonstrated that the incidence of LPLN metastasis is approximately 15% in patients with advanced low rectal cancer who underwent LPLD, and varies from 10.6 to 25.5% (Konishi et al. 2010). The major drawback is that the above mentioned results were obtained from patients who had not undergone preoperative CRT. In the Western countries, the standard treatment for patients with locally advanced rectal cancer is preoperative CRT followed by TME alone. LPLN metastasis is generally considered a metastatic disease that is not amenable to surgical cure. Moreover, some studies have revealed that preoperative radiotherapy followed by TME led to acceptable local control that was as good as that achieved by extended surgery, which included LPLD (Georgiou et al. 2009; Quadros et al. 2012). Consequently, it is widely accepted in the Western countries that routine LPLD is not necessary. However, several studies have revealed that selective LPLD might improve local control and survival in patients with LPLN metastasis in advanced low rectal cancer who have been treated with preoperative CRT. Akiyoshi and colleagues showed that the rate of pathological LPLN metastasis was 66% when they performed pre-CRT LPLD based on LPLN size and that preoperative CRT alone could not eradicate LPLN metastasis completely, thus LPLD might improve local control and survival of patients with LPLN metastasis in advanced low rectal cancer treated with preoperative CRT (Akiyoshi et al. 2014). Kim and colleagues showed that lateral pelvic recurrence is the most common pattern of local recurrence following neoadjuvant CRT plus TME alone and that patients with preoperative evidence of LPLN metastasis could benefit from LPLD even after neoadjuvant CRT (Kim et al. 2008). In our study, among the 195 patients who achieved pCR, CT scan or MRI detected lateral LN metastasis in ten patients with low rectal cancer, 3 (30%) of whom eventually developed lateral pelvic recurrence after follow-up. Although the evidence from our cohort is very limited, we agree with previous studies on the most common pattern of local recurrence, and that TME alone following preoperative CRT might be insufficient for controlling LPLN metastasis that is present before CRT. As suspicious metastatic LNs in the lateral pelvic area are a risk factor for local recurrence in patients who have undergone curative resection with preoperative concurrent CRT, and LPLD has been associated with increased morbidity such as blood loss, and urinary and sexual dysfunction, correct detection of LPLN is crucial. Previously, CT was the standard method for assessing the pre-treatment clinical nodal stage. Unfortunately, a meta-analysis (Bipat et al. 2004) reported only 55% sensitivity for LN involvement by CT staging. Consequently, more reliable imaging criteria for detecting LPLN metastasis are needed. Currently, newer techniques, e.g., MRI or positron emission tomography (PET) scanning are used to improve LN staging accuracy. Brown et al. (2003) found that high-spatial resolution MRI had a sensitivity of 85% [51/60 (95% confidence interval, CI: 74%, 92%)] and a specificity of 97% [216/221 (95% CI: 95%, 99%)] for LN (+) defined by the presence of mixed signal intensity or irregular nodal capsule border. Koh and colleagues (Koh et al. 2010) used ultra-small paramagnetic iron oxide (USPIO), a LN-specific biodegradable contrast agent with the potential to enable identification of nodal metastasis independently of LN size for MRI. They found that the USPIO enhancement pattern had higher diagnostic specificity, but the same sensitivity, as morphological findings in pathologically matched mesorectal LNs (specificity, 93 vs. 75%; sensitivity, 65 vs. 65%). It appears that PET/CT is less accurate than MRI for LN staging (Farwell et al. 2014), but has higher specificity than MRI (83–85% vs. 67%) in nodal staging (Kim et al. 2011; Cipe et al. 2013). Additionally, we believe that combined MRI and PET (fusion imaging) would increase the accuracy of nodal staging. Further studies are essential for identifying the most reliable imaging criteria for LPLN metastasis in patients treated with preoperative CRT.
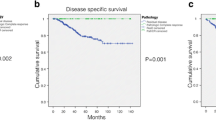
The present study demonstrates that distant metastases are the major failure pattern of patients who achieve pCR after CRT, which is similar to the findings of previous reports (Table 2). Maas and colleagues reported a 5-year distant metastasis rate of 11.2% (Maas et al. 2010). Capirci and colleagues performed a long-term analysis of 566 patients who achieved pCR, reporting a distant metastasis rate of 8.9% after a 46-month follow-up (Capirci et al. 2008). The persistence of distant metastases suggests the inadequate systemic control of the CRT regimen. Thus, the high rate of distant failure may indicate that adjuvant chemotherapy is warranted in these patients. However, the role of postoperative CT following neoadjuvant CRT and radical surgery for patients with locally advanced rectal cancer is still not entirely clear, especially in patients with pCR. Some studies suggest that there is little or no benefit from chemotherapy (Maas et al. 2010; Capirci et al. 2008; Kiran et al. 2012). However, Collette and colleagues (Collette et al. 2007) demonstrated that the administration of adjuvant chemotherapy was associated with significantly improved overall survival. Their study randomly assigned patients to adjuvant chemotherapy or no adjuvant chemotherapy after (chemo) radiation and surgery for rectal cancer. Patients with ypT0–2 tumors, but not ypT3–4 tumors, benefited from adjuvant chemotherapy; the authors explained that tumors that respond well to preoperative FU-based chemoradiation would also be sensitive to adjuvant chemotherapy involving this drug. These contrasting findings indicate that more trials involving adjuvant chemotherapy following neoadjuvant CRT should be performed in future.
Consistent with previous reports, we also observed a unique pattern of distant recurrence, where there was a predominance of non-liver metastases. In our study, only one patient developed liver metastasis; extra-liver metastases involved seven lung metastases and two bone metastases. Different theories have been proposed to explain the pattern of metastases, although this process appears to be multifactorial (Ding et al. 2012). The “seed and soil” hypothesis states that, due to different organ-specific microenvironments, tumors may metastasize to specific organs independently from the vascular anatomy (Fidler 2003). However, some researchers suggest that tumors might metastasize to specific organs independently based on the differential level of thymidylate synthase (TS) mRNA, which causes differential sensitivity to 5-FU-based chemotherapy. Patients with higher TS mRNA levels easily develop pulmonary metastasis (Yamada et al. 2001). Such findings are also attributed to the nature of the venous drainage of the rectum (Watanabe et al. 2011). Intensive surveillance schemes and improved imaging technology may also contribute to the high rate of lung metastasis detected, which is consistent with that of previous studies (Kirke et al. 2007; Lee et al. 2007).
There are some potential limitations to this study. The first lies in the limited number of enrolled patients, given their good outcomes. The second potential limitation is that the number of LNs retrieved was much lower than that in previous reports on patients treated with neoadjuvant CRT. However, the inadequate LN sampling in our study may have been due to improved tumor response. The third potential limitation involves regular assessment of the circumferential resection margin (CRM) status. The CRM is considered one of the strongest predictors of surgical failure in rectal cancer (Kelly et al. 2011). We do not routinely assess the CRM status, but the pathologists at our hospitals routinely perform macroscopic evaluation of rectal cancer resection specimens. The quality of the mesorectum is classified as good (mesorectal), intermediate (intramesorectal), or poor (muscularis propria plane) (Quirke 2003). The mesorectum quality of the 18 patients included in our data was good, indicating smooth CRM on slicing.
In conclusion, our data demonstrate that distant metastases are the major failure pattern of patients who achieve pCR after CRT and that non-liver metastases are the predominant pattern of distant recurrence. Our results indicate the possible predominant pattern of distant recurrence and serve as a basis for managing LPLN metastasis in low rectal cancer. Patients with LPLN metastasis in advanced low rectal cancer treated with preoperative CRT would benefit from selective lateral LN excision.
Abbreviations
- 5-FU:
-
5-Fluorouracil
- AJCC:
-
American Joint Committee on Cancer
- APR:
-
Abdominoperineal resection
- AWD:
-
Alive with disease
- Cape:
-
Capecitabine
- chemo:
-
Chemotherapy
- CI:
-
Confidence interval
- CRM:
-
Circumferential resection margin
- CRT:
-
Chemoradiotherapy
- CT:
-
Computed tomography
- DOD:
-
Died of disease
- F:
-
Female
- FOLFOX6:
-
5-FU, leucovorin, oxaliplatin
- LAR:
-
Low anterior resection
- LN:
-
Lymph nodes
- LPLD:
-
Lateral pelvic lymph node dissection
- LPLN:
-
Lateral pelvic lymph node
- M:
-
Male
- MRI:
-
Magnetic resonance imaging
- OS:
-
Overall survival
- Oxa:
-
Oxaliplatin
- pCR:
-
Pathologic complete response
- PET:
-
Positron emission tomography
- pN (n):
-
Number of lymph nodes retrieved
- RFS:
-
Recurrence-free survival
- RT:
-
Radiotherapy
- Tar:
-
Targeted therapy
- TME:
-
Total mesorectal excision
- USPIO:
-
Ultra-small paramagnetic iron oxide
- XELOX:
-
Capecitabine and oxaliplatin
References
Akiyoshi T, Ueno M, Matsueda K, Konishi T, Fujimoto Y et al (2014) Selective lateral pelvic lymph node dissection in patients with advanced low rectal cancer treated with preoperative chemoradiotherapy based on pretreatment imaging. Ann Surg Oncol 21:189–196
Bipat S, Glas AS, Slors FJ, Zwinderman AH, Bossuyt PM et al (2004) Rectal cancer: local staging and assessment of lymph node involvement with endoluminal US, CT, and MR imaging–a meta-analysis. Radiology 232:773–783
Brown G, Richards CJ, Bourne MW, Newcombe RG, Radcliffe AG et al (2003) Morphologic predictors of lymph node status in rectal cancer with use of high-spatial-resolution MR imaging with histopathologic comparison. Radiology 227:371–377
Capirci C, Valentini V, Cionini L, De Paoli A, Rodel C et al (2008) Prognostic value of pathologic complete response after neoadjuvant therapy in locally advanced rectal cancer: long-term analysis of 566 ypCR patients. Int J Radiat Oncol Biol Phys 72:99–107
Cipe G, Ergul N, Hasbahceci M, Firat D, Bozkurt S et al (2013) Routine use of positron-emission tomography/computed tomography for staging of primary colorectal cancer: does it affect clinical management? World J Surg Oncol 11:49
Collette L, Bosset JF, den Dulk M, Nguyen F, Mineur L et al (2007) Patients with curative resection of cT3-4 rectal cancer after preoperative radiotherapy or radiochemotherapy: does anybody benefit from adjuvant fluorouracil-based chemotherapy? A trial of the European Organisation for Research and Treatment of Cancer Radiation Oncology Group. J Clin Oncol 25:4379–4386
de Campos-Lobato LF, Stocchi L, da Luz Moreira A, Geisler D, Dietz DW et al (2011) Pathologic complete response after neoadjuvant treatment for rectal cancer decreases distant recurrence and could eradicate local recurrence. Ann Surg Oncol 18:1590–1598
de Campos-Lobato LF, Stocchi L, de Sousa JB, Buta M, Lavery IC et al (2013) Less than 12 nodes in the surgical specimen after total mesorectal excision following neoadjuvant chemoradiation: it means more than you think! Ann Surg Oncol 20:3398–3406
de la Fuente SG, Manson RJ, Ludwig KA, Mantyh CR (2009) Neoadjuvant chemoradiation for rectal cancer reduces lymph node harvest in proctectomy specimens. J Gastrointest Surg 13:269–274
Ding P, Liska D, Tang P, Shia J, Saltz L et al (2012) Pulmonary recurrence predominates after combined modality therapy for rectal cancer: an original retrospective study. Ann Surg 256:111–116
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17:1471–1474
Farwell MD, Pryma DA, Mankoff DA (2014) PET/CT imaging in cancer: current applications and future directions. Cancer
Fidler IJ (2003) The pathogenesis of cancer metastasis: the ‘seed and soil’ hypothesis revisited. Nat Rev Cancer 3:453–458
Garcia-Aguilar J, Hernandez de Anda E, Sirivongs P, Lee SH, Madoff RD et al (2003) A pathologic complete response to preoperative chemoradiation is associated with lower local recurrence and improved survival in rectal cancer patients treated by mesorectal excision. Dis Colon Rectum 46:298–304
Georgiou P, Tan E, Gouvas N, Antoniou A, Brown G et al (2009) Extended lymphadenectomy versus conventional surgery for rectal cancer: a meta-analysis. Lancet Oncol 10:1053–1062
Govindarajan A, Gonen M, Weiser MR, Shia J, Temple LK et al (2011) Challenging the feasibility and clinical significance of current guidelines on lymph node examination in rectal cancer in the era of neoadjuvant therapy. J Clin Oncol 29:4568–4573
Ha YH, Jeong SY, Lim SB, Choi HS, Hong YS et al (2010) Influence of preoperative chemoradiotherapy on the number of lymph nodes retrieved in rectal cancer. Ann Surg 252:336–340
Kelly SB, Mills SJ, Bradburn DM, Ratcliffe AA, Borowski DW et al (2011) Effect of the circumferential resection margin on survival following rectal cancer surgery. Br J Surg 98:573–581
Kim TH, Jeong SY, Choi DH, Kim DY, Jung KH et al (2008) Lateral lymph node metastasis is a major cause of locoregional recurrence in rectal cancer treated with preoperative chemoradiotherapy and curative resection. Ann Surg Oncol 15:729–737
Kim DJ, Kim JH, Ryu YH, Jeon TJ, Yu JS et al (2011) Nodal staging of rectal cancer: high-resolution pelvic MRI versus (1)(8)F-FDGPET/CT. J Comput Assist Tomogr 35:531–534
Kiran RP, Kirat HT, Burgess AN, Nisar PJ, Kalady MF et al (2012) Is adjuvant chemotherapy really needed after curative surgery for rectal cancer patients who are node-negative after neoadjuvant chemoradiotherapy? Ann Surg Oncol 19:1206–1212
Kirke R, Rajesh A, Verma R, Bankart MJ (2007) Rectal cancer: incidence of pulmonary metastases on thoracic CT and correlation with T staging. J Comput Assist Tomogr 31:569–571
Koh DM, George C, Temple L, Collins DJ, Toomey P et al (2010) Diagnostic accuracy of nodal enhancement pattern of rectal cancer at MRI enhanced with ultrasmall superparamagnetic iron oxide: findings in pathologically matched mesorectal lymph nodes. AJR Am J Roentgenol 194:W505–W513
Konishi T, Watanabe T, Nagawa H, Oya M, Ueno M et al (2010) Preoperative chemoradiation and extended pelvic lymphadenectomy for rectal cancer: Two distinct principles. World. J Gastrointest Surg 2:95–100
Lee WS, Yun SH, Chun HK, Lee WY, Yun H (2007) Clinical usefulness of chest radiography in detection of pulmonary metastases after curative resection for colorectal cancer. World J Surg 31:1502–1506
Maas M, Nelemans PJ, Valentini V, Das P, Rodel C et al (2010) Long-term outcome in patients with a pathological complete response after chemoradiation for rectal cancer: a pooled analysis of individual patient data. Lancet Oncol 11:835–844
Marks JH, Valsdottir EB, Rather AA, Nweze IC, Newman DA et al (2010) Fewer than 12 lymph nodes can be expected in a surgical specimen after high-dose chemoradiation therapy for rectal cancer. Dis Colon Rectum 53:1023–1029
Park IJ, You YN, Agarwal A, Skibber JM, Rodriguez-Bigas MA et al (2012) Neoadjuvant treatment response as an early response indicator for patients with rectal cancer. J Clin Oncol 30:1770–1776
Quadros CA, Falcao MF, Carvalho ME, Ladeia PA, Lopes A (2012) Metastases to retroperitoneal or lateral pelvic lymph nodes indicated unfavorable survival and high pelvic recurrence rates in a cohort of 102 patients with low rectal adenocarcinoma. J Surg Oncol 106:653–658
Quirke P (2003) Training and quality assurance for rectal cancer: 20 years of data is enough. Lancet Oncol 4:695–702
Rodel C, Martus P, Papadoupolos T, Fuzesi L, Klimpfinger M et al (2005) Prognostic significance of tumor regression after preoperative chemoradiotherapy for rectal cancer. J Clin Oncol 23:8688–8696
Roh MS, Colangelo LH, O’Connell MJ, Yothers G, Deutsch M et al (2009) Preoperative multimodality therapy improves disease-free survival in patients with carcinoma of the rectum: NSABP R-03. J Clin Oncol 27:5124–5130
Rullier A, Laurent C, Capdepont M, Vendrely V, Belleannee G et al (2008) Lymph nodes after preoperative chemoradiotherapy for rectal carcinoma: number, status, and impact on survival. Am J Surg Pathol 32:45–50
Sauer R, Becker H, Hohenberger W, Rodel C, Wittekind C et al (2004) Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351:1731–1740
Sebag-Montefiore D, Stephens RJ, Steele R, Monson J, Grieve R et al (2009) Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial. Lancet 373:811–820
Smith KD, Tan D, Das P, Chang GJ, Kattepogu K et al (2010) Clinical significance of acellular mucin in rectal adenocarcinoma patients with a pathologic complete response to preoperative chemoradiation. Ann Surg 251:261–264
Watanabe K, Saito N, Sugito M, Ito M, Kobayashi A et al (2011) Predictive factors for pulmonary metastases after curative resection of rectal cancer without preoperative chemoradiotherapy. Dis Colon Rectum 54:989–998
Wibe A, Moller B, Norstein J, Carlsen E, Wiig JN et al (2002) A national strategic change in treatment policy for rectal cancer–implementation of total mesorectal excision as routine treatment in Norway. A national audit. Dis Colon Rectum 45:857–866
Yamada H, Ichikawa W, Uetake H, Shirota Y, Nihei Z et al (2001) Thymidylate synthase gene expression in primary colorectal cancer and metastatic sites. Clin Colorectal Cancer 1:169–173 (discussion 174)
Acknowledgements
This work was supported by funds from Nature Science Foundation of China (No. 81101591); Natural Science Foundation of Guangdong Province, China (No. S2011040005278; No. 9151008901000157); and Science and Technology Planning Project of Guangdong Province, China (No. 2010B060900043).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors report no conflicts of interest in this work.
Ethical approval
This study was approved by the ethics committees of the Sun Yat-Sen University Cancer Center and the Sixth Affiliated Hospital of Sun Yat-Sen University and was performed in accordance with the ethical standards laid down in the Declaration of Helsinki. The persons included in the study provided informed consent prior to their inclusion in the study.
Additional information
W.-H. Fan and J. Xiao contributed equally to this work.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Fan, WH., Xiao, J., An, X. et al. Patterns of recurrence in patients achieving pathologic complete response after neoadjuvant chemoradiotherapy for rectal cancer. J Cancer Res Clin Oncol 143, 1461–1467 (2017). https://doi.org/10.1007/s00432-017-2383-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-017-2383-9