Abstract
Optimal adherence to CML therapy is of key importance to maximize treatment effectiveness. Two clinical studies (ADAGIO and Hammersmith) have proven a clear correlation between adherence and achieving optimal treatment response and have revealed that non-adherence is common in CML patients (Marin et al. in J Clin Oncol 28(24):2381–2388, 2010, Noens et al. in Haematologica 99(33):437–447, 2014). The aim of this study is to assess the extent of suboptimal adherence and to investigate motivations and behavioural patterns of adherence in a worldwide patient sample. Questionnaires were provided by the CML Advocates Network and were filled in by patients online and offline. Patient characteristics, treatment and motivations were collected. Adherence was assessed by the 8-item Morisky Medication Adherence scale. Logistic regression models were fitted to investigate the influence of different factors on adherence. Overall, 2 546 questionnaires from 63 countries and 79 CML patient organisations were evaluable. 32.7% of participants were highly adherent, 46.5% were in the medium and 20.7% in the low adherence group. Factors increasing the probability of being in the high adherence group are older age, male sex, management of side effects, only one tablet per day and feeling well informed about CML by the doctor. More than 2 years since diagnosis were significantly lowering the chance as was the use of reminding tools. Living arrangements, multiple medication and personal payment obligations increased the probability to be at least in the medium adherent group. This is the most comprehensive study conducted to date to gain knowledge about factors causing non-adherence in CML. Better information on the disease, medication and management of side effects, supported by haematologists, is key to improve adherence.
Similar content being viewed by others
Introduction
Patient adherence—defined as ‘the extent to which the patient follows medical instructions’ (Sabaté 2003)—is a complex and multifactorial issue, especially in medical conditions that require long-term therapy such as chronic phase chronic myeloid leukaemia (CML).
The introduction of tyrosine kinase inhibitors (TKIs) for the treatment of CML has substantially improved the outcome. The 10-year survival probability increased from 20 to 53% with previous usually interferon alpha (IFN)-based standard therapy (Hehlmann et al. 2003, 2007) to about 90% in the imatinib era (Bjorkholm et al. 2011; Hehlmann et al. 2011). Given the treatment success and approximately 6000 newly diagnosed patients per year in Europe (Hoffmann et al. 2015) and 6600 in the US (Howlader et al. 2015) maximizing adherence to promote optimal outcomes is crucial.
To reach or even improve the described level of effectiveness seen in clinical trials adherence to the prescribed dose of tyrosine kinase inhibitors is critical (Marin et al. 2010). The extent and effects of partial and non-adherence on the biology of CML and on treatment outcome has been investigated in several studies showing that non-adherence is more common than expected in a potentially lethal disease treated with an oral medication (Noens et al. 2014). As few as 14% of CML patients were perfectly adherent in a Belgian example described by Noens et al. (2009) while a third of the patients had to be classified as non-adherent. Also, in a Finnish sample only 23% of patients were highly adherent (Kekale et al. 2014). Similarly, in a US sample described by Darkow et al. (2007) 31% of the patients reported a treatment interruption within a year of observation. Kapoor et al. (2015) report an example from India with 22% highly adherent patients and 25% patients classified in the low adherence group. Marin et al. (2010) report 26% of patients with less than 90% adherence in their UK study population. Their study also shows the significant negative impact of non-adherence on outcomes such as complete and major molecular response there were no molecular responses in patients with an adherence below 80%.
Data on the driving factors of non-adherence in haematology, however, is still scarce. Eliasson et al. (2011) interviewed 17 patients classified as non-adherent and four classified as adherent investigating motivations for adherence and reasons for non-adherence. They identified unintentional reasons such as forgetting and problems with the prescription and intentional reasons such as the attempt to minimize side-effects by missing or reducing doses as motives for non-adherence. Often non-adherent patients were not properly informed of the consequences and generally weighted short-term effects of not taking the drug more important than the possible adverse long-term consequences.
In an Italian study, Efficace et al. (2012) found 53% of 413 patients with optimal adherence behaviour and identified social support and concomitant medication as primary drivers for adherence while lack of information was influencing adherence negatively.
The objective of this patient-led study was to further investigate the extent of non-adherence and analyse motivations and behavioural patterns of adherence in CML on a much broader database, to explore the cultural influence and differences that exist with respect to patient adherence. Only then strategies and means to improve adherence of patients with CML can be developed.
Methods
Study population and data collection
The CML Advocates Network, connecting 106 CML patient organisations from 81 countries (20 in Western Europe, 27 in Central and Eastern Europe, 21 in Asia and Pacific Region, 8 in North America, 12 in Latin America, 18 in Middle East and Africa), conducted an international project investigating patterns of medication-taking behaviours of CML patients, supported by the CML investigator groups German CML Study Group, the French FI LMC group and the Italian GIMEMA group.
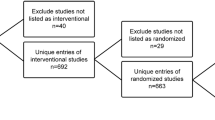
A web-based survey was launched in 12 languages (English, French, German, Italian, Hebrew, Polish, Dutch, Czech, Spanish, Portuguese, Russian, Finnish) enrolling 2151 CML patients from 63 countries from September 2012 to January 2013 via 79 CML patient association’s websites, email and patient meetings. The identical questionnaire was provided in a pen-and-paper version to patients recruited during appointments in the recruitment period in clinics in France, Germany and Italy. The questionnaire was returned by 395 patients in a pre-stamped envelope to an independent data centre in the UK. Questions included potential factors associated with non-adherence as well as on patients’ perception of disease and treatment burden.
Eligibility criteria for participating in this survey were: minimum age 18 years, presence of CML and oral treatment with TKI.
Patient demographics as well as details on diagnosis and treatment of CML were collected. Adherence was assessed by the 8-item Morisky Medication Adherence scale (MMAS-8). In case of optimal adherence the first seven items of the scale sum up to seven points. The eighth item can yield 0, 0.25, 0.5, 0.75 or 1 point depending on how often the patient had problems remembering to take all medications. This way the MMAS-8 classifies patients into low (<6 points), medium (6 to 7.75 points) and high (8 points) adherence groups (Morisky et al. 2008). The exact wording of the MMAS-8 can be found in Section F of the questionnaire (Supplement 1). In addition, questions about reasons and motives for intentional and unintentional non-adherence were asked as well as questions regarding the interaction with the treating clinician. Also, the use of tools supporting adherence were asked for.
Statistical analysis
Results are presented as proportions, means and standard deviations or medians and ranges depending on the nature of the variable. Differences between groups were tested using the Chi-squared test and Kruskal–Wallis tests depending on the nature of the data.
To assess the simultaneous influence of factors on adherence two logistic regression models were fitted as odds were not proportional between adherence groups and thus did not allow for ordinal logistic regression (Le 1998; Bender and Grouven 1998). Linearity was checked graphically. Variables that were not linearly related with adherence were transformed or categorized and dummy coded. Wald tests were used to examine significance. Odds ratios (OR) and their 95% confidence limits were calculated to describe the effect size of different factors on being at least medium adherent or being at least highly adherent. Goodness of fit was assessed using the c statistic, which is based on the ROC, thus values close to 1 indicate a meaningful model and values close to 0.5 indicate a model that is not better than chance. Level of significance was set to 5% for all statistical tests. For each regression the full as well as the final model including only the significant variables are reported in the respective tables. All calculations were performed using SAS version 9.2 software (Cary, NC, USA).
Results
Patient characteristics
Overall 2546 questionnaires completed by CML patients from 63 countries were evaluable. 2151 patients responded online, 395 questionnaires were returned on paper. 53.6% of respondents were from Western Europe (n = 1366), 14.5% from Eastern Europe (n = 368) (including Russia, n = 84), 7.8% from Anglo-American countries [n = 198, including Australia and New Zealand (n = 41 and n = 25, respectively)], 9.8% were from Asia (n = 249), 1% from Africa (n = 21), 7.8% from Latin-America (n = 198), and 5.4% from the Near and Middle East (n = 138). Eight respondents did not find their country in the provided list and thus answered ‘other’.
Median age of patients was 51 years (range 18–96) and 52.4% of participants were male. Median time from diagnosis was 4 years (0–27). 22.8% of the responders were enrolled in a clinical trial. 97.2% were in chronic phase, 2.8% in accelerated or blastic phase. 86.2% of respondents lived with a spouse, family member or carer. In terms of highest level of education, 19.0% had up to 8 years of school education (primary/middle school degree), 28.9% had 9–12 years of education (high school degree), and 52.4% more than 12–13 years of education (e.g. university degree).
1555 patients (61.3%) were on imatinib, 554 (21.8%) on nilotinib, 332 (13.1%) on dasatinib, and 96 (3.8%) on other treatments. 1767 (69.4%) of patients were taking their medication once a day, 27.5% twice a day, 1.8% three or four times a day, and 1.3% at other schedules. 52.3% of patients did not take other concomitant medications, 28.3% one to two additional medications, and 19.4% three to six additional medications besides their TKI therapy.
81.9% of patients did not need to pay at all for their CML medication, while almost every fifth had some kind of co-payment. However, only 2% had to pay fully for their medication and 4.6% payed more than 50 Euros per month. 76.1% of patients received their medication from a pharmacy, 17.5% during the consultation with their CML doctor, and 6.4% through other channels. 47.8% need to travel at least once per month get their supply of CML medication.
75.8% of patients use some kind of tool to remind them about taking their medication, and 69.6% state that routines help them greatly to take the medication regularly. 12.8% of patients do not have a routine.
Almost all patients (98.0%) see their doctors at least once in six months, half of them (53.0%) once or twice, the other patients more than three times. Overall patients were satisfied with the information given to them by their doctors (90.9% were at least somewhat satisfied); however, only 59.3% were informed about the risks of missing doses by their doctors. Most patients (90.1%) felt that their doctors were approachable to discuss challenges of taking the CML medication.
Adherence
According to the MMAS-8, 32.7% of participants where highly adherent, 46.5% were in the medium and 20.7% in the low adherence group.
In most regions the proportion of highly adherent patients ranged between 32.1%-34.8%. A low proportion of highly adherent patients was noticeable in the Anglo-American (24.2%) and African (19.1%) countries. The proportion of medium adherent patient ranges between 40.6% and 50.4% in all countries. The rate of low adherent patients is highest in Africa with 38.1%, however, the sample size is very limited (n = 21).
Demographic factors, disease related factors, factors related to medication supply and factors related to the health care providers were investigated for their influence on adherence (Table 1).
Men tended to be more adherent than women (p = 0.0002). Age had a significant influence on adherence—while the median age of highly adherent patients was 55 years, it was 44 years in the low adherence group and 51 in the medium adherent group (p < 0.0001). Also, the education level had a significant influence (lower adherence with increasing years of education, 0 = 0.0018). However, there was a strong correlation between age and duration of education. Patients with less years of education were older than patients with more years of education [age median: 55 years (up to 8 years of education), 51 years (9–12 years), 48 years (more than 12 years)]. Patients who did not live with someone were in the low adherence group more frequently (25.6%) than patients living with a family member or partner (20.0%).
Of the patients diagnosed with CML less than a year ago, more were highly adherent (40.9%) than those who were diagnosed longer ago. Chronic phase patients were mostly medium adherent (47.4%), while patients in accelerated or blastic phase were more often either highly (38.3%) adherent or in the low adherence group (24.9%).
Investigating treatment related factors management of side effects and number of daily doses was most influential. Most patients needed to take their medication once or twice daily. 35.8% of patients taking their medication once daily were highly adherent, whereas patients taking their medication twice daily were highly adherent only in 24.9% of cases and 26.7% were in the low adherence group. The medication prescribed did also have significant influence (<0.0001) but is strongly correlated to the number of times the patient has to take the medication daily. Most patients receiving imatinib and dasatinib only had to take one dose a day (76.4 and 94.8%) while 91.5% of patients on nilotinib treatment had to take two. Having to take other medications as well was also beneficial for adherence while taking part in a clinical trial did not show an impact.
Regarding the side effects patients with no side effects were more adherent (39.3% high, 15.6% low adherence) than patients who experience side effects (32.2% high, 21.1% low adherence) but a major difference can be seen between patients who state that they found their side effects were well managed (40.9% high, 16.7% low adherence) and those who do not think so (24.2% high, 24.9% low adherence).
The more satisfied patients were with the information they received from their CML doctors the more likely they were to be in the highly adherent group and the less likely they were to be in the low adherence group (p < 0.0001). Provided information about the risks of non-adherence did not influence adherence significantly. Patients finding their doctors were approachable to discuss challenges of taking the CML medication were more likely in the high and less likely in the low adherence group (p < 0.0001).
Matters of supply with the respective medication did influence adherence too. Personal co-payment for medication of more than 50 Euros per month had negative influence on adherence (p = 0.0088). During the first months of taking a medication the adherence was higher than thereafter. The need to travel to get the medication and the required frequency of travelling did not influence adherence. Also no interaction between travel distance and travel frequency could be detected.
Patients having to use tools to remind them about their medication are less adherent (31.0% high vs, 21.3% low adherence) than patients who do not use tools (38.1% high versus 18.9% low adherence).
Two logistic regression models were fitted starting with the variables sex, age, phase of disease, time since diagnosis and time on current medication, management of side effects, number of daily doses, co-payment obligations, use of reminding tools, living arrangements, need to take other medications besides the CML medication, information about the risks of non-adherence and satisfaction with the information received from the doctor. Education was not included as it was strongly correlated with age and the approachability of the doctor to discuss challenges was not included as it was strongly correlated with the satisfaction with information and management of side effects. Routine was not included as a factor as excluding the answer categories that are biased towards lower adherence would lead to a large proportion of missing values in the patient group with lower adherence. Instead of side effects the variable indicating the management of side effects was used as in the univariate analysis, the effect of the management of side effects was larger than the effect of having side effects but both are correlated.
The first model evaluated what factors are independently influential on being at least medium adherent versus being in the low adherence group, the second model evaluated which factors were influential on being in the high adherence group versus being in the low or medium adherent groups. p values of the Wald test, ORs and their 95% confidence limits are reported in Tables 2 and 3.
Significant influence factors for being at least medium adherent are older age, male sex, not living alone, management of side effects, having to take other medication, number of doses per day, personal payment obligations and good information about CML from the treating doctor. More than 2 years since diagnosis was significantly lowering the probability for at least medium adherence (Table 2).
Factors increasing the probability of being in the high adherence group are older age, male sex, management of side effects and only one tablet per day and feeling well informed about CML by the doctor. Living arrangements, having to take other medications and personal payment obligations, however, were not significant. More than 2 years since diagnosis were significantly lowering the chance of being highly adherent as was the use of reminding tools. The influence of reminding tools on adherence had already negative influence on the odds of being at least medium adherent (OR 0.931, p = 0.5743), but the negative influences on the odds of being highly adherent is significant (OR 0.756, p = 0.0075).
Discussion
To our knowledge this is the largest and most comprehensive study conducted to gain knowledge about drivers of adherence in CML.
There is clear evidence that survival (Hoglund et al. 2013) of CML patients is close to the age-matched general population and also quality of life in the aged-matched general population is similar for most CML patient groups (Efficace et al. 2011) when CML is treated effectively in chronic phase with current therapies. However, every fifth patient is classified as having “low adherence” according to the MMAS.
Unsurprisingly, not a single factor is responsible for adherence and prediction is difficult but there are some factors emerging as highly relevant. The main factors that can be influenced at least partially are: the quality of the doctor–patient relationship, management of side effects and the number of doses per day.
Two major factors affecting adherence that can be influenced by health care professionals is the management of side effects and the provision of the patients with relevant information on CML. As our results show that not the fact of having side effects influences adherence strongly although side effects are frequent with all TKIs (Baccarani et al. 2014) but how well the side effects are managed every room for improvement should be used. It should also be noted that patients who feel well informed about their disease are significantly more adherent while information on the risks of missing doses did not have influence. This emphasizes that informing patients instead of only instructing them is more useful especially in chronic diseases as it has been shown before (Joosten et al. 2008) and that training for health care professionals to empower their health adherence counselling abilities can be beneficial (Sabaté 2003; Hirji et al. 2013).
Only having to remember one dose per day is a major factor driving adherence. It makes TKIs that only have to be taken once daily a good choice as a standard therapy concerning adherence (Baccarani et al. 2013). Potentially beneficial effects of other treatment schemes have to be weighed against a potential decrease in adherence for the individual patient.
The general importance of a good doctor–patient relationship has been described often in adherence research and cannot be emphasized enough especially in chronic diseases (Efficace et al. 2012; Vermeire et al. 2001). Generally, it is important for physicians to understand the impact they may be having on adherence, and to be involved in promoting better adherence in their CML patients. The high adherence population tended to be more open with their physicians as they are more likely to admit to missing a dose. This could be linked to the fact that they also find their physicians to be more approachable. Those with high adherence are also more likely to be satisfied with the information provided by their doctor.
The adverse influence of co-payments for TKIs had been described before (Kapoor et al. 2015; Dusetzina et al. 2014) and also in our data we saw that less personal payment obligations and living alone were factors especially increasing the patient’s probability to be at least medium adherent which is important as being in the low adherence group will most probably result in treatment failure (Marin et al. 2010).
In our analysis, the use of reminding tools is negatively related to adherence. It is, however, more likely that patients who have problems to be adherent will also be more likely to use a reminding tool and that their adherence level would be even lower without the tool. To truly access then benefits of reminding tools they need to be studied prospectively.
Mainly in the first but also in the second year after the diagnosis of CML patients are more likely to be adherent than later on. This might result from the first confrontation with a diagnosis of leukaemia but the effect wears off with treatment success and side effects of medication being more evident than impairment by the disease itself.
The positive influence of higher age on adherence in our analysis seems surprising at first as the adherence of older patients is often assumed to be suboptimal although it is not very well described in the literature (Banning 2008; Gellad et al. 2011; Balkrishnan 1998), but is likely resulting from data collection that was done mostly online resulting in a median age of 51 years (in comparison to an estimated median age in Europe of 56 years at diagnosis (Hoffmann et al. 2015)) with only 25% of the patients being older than 61 years. Only 7% (n = 189) were older than 70 and only 38 patients were older than 80 years. So the very old age group is strongly underrepresented and a decline in adherence in this group has been observed in other studies (Dunabr-Jacob and Mortimer-Stephens 2001). However, the observation that the ‘young-old’—aged 60 to 70 years—demonstrate the highest levels of adherence has also been made before (Dunabr-Jacob and Mortimer-Stephens 2001). Also there might be a correlation with the number of medications patients have to take per day. The effect of more medications that have to be taken influencing adherence positively has also already been described by Efficace et al. (2012). Patients who have to take medications with an instant response to non-adherence might be more adherent to their CML medication as well, because they take it together with the other medication.
In the end, improving adherence is team work—of the patients, their doctors, relatives, nurses and pharmacists on one side, of patient organisations, expert groups and researchers on the other hand. Key factors predicting non-adherence can potentially help physicians and patient organisations to identify patients early who need more information and help to cope with their disease and medication.
References
Baccarani M, Deininger MW, Rosti G, Hochhaus A, Soverini S, Apperley JF et al (2013) European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood 122(6): 872–884
Baccarani M, Efficace F, Rosti G (2014) Moving towards patient-centered decision-making in chronic myeloid leukemia: assessment of quality of life and symptom burden. Haematologica 99(2):205–208
Balkrishnan R (1998) Predictors of medication adherence in the elderly. Clin Ther 20(4):8
Banning M (2008) Older people and adherence with medication: a review of the literature. Int J Nurs Stud 45(10):11
Bender R, Grouven U (1998) Using binary logistic regression models for ordinal data with non-proportional odds. J Clin Epidemiol 51(10):7
Bjorkholm M, Ohm L, Eloranta S, Derolf A, Hultcrantz M, Sjoberg J et al (2011) Success story of targeted therapy in chronic myeloid leukemia: a population-based study of patients diagnosed in Sweden from 1973 to 2008. J Clin Oncol 29(18): 2514–2520
Darkow T, Henk H, Thomas S, Feng W, Baladi J, Goldberg G et al (2007) Treatment interruptions and non-adherence with imatinib and associated healthcare costs: a retrospective analysis among managed care patients with chronic myelogenous leukaemia. Pharmacoeconomics 25(6):15
Dunbar-Jacob J, Mortimer-Stephens MK (2001) Treatment adherence in chronic disease. J Clin Epidemiol 54(12):S57–S60
Dusetzina SB, Winn AN, Abel GA, Huskamp HA, Keating NL (2014) Cost sharing and adherence to tyrosine kinase inhibitors for patients with chronic myeloid leukemia. J Clin Oncol 32(4): 306–311.
Efficace F, Baccarani M, Breccia M, Alimena G, Rosti G, Cottone F et al (2011) Health-related quality of life in chronic myeloid leukemia patients receiving long-term therapy with imatinib compared with the general population. Blood 118(17): 4554–4560
Efficace F, Baccarani M, Rosti G, Cottone F, Castagnetti F, Breccia M et al (2012) Investigating factors associated with adherence behaviour in patients with chronic myeloid leukemia: an observational patient-centered outcome study. Br J Cancer 107(6):904–909
Eliasson L, Clifford S, Barber N, Marin D (2011) Exploring chronic myeloid leukemia patients’ reasons for not adhering to the oral anticancer drug imatinib as prescribed. Leuk Res 35(5): 626–630
Gellad WF, Grenard JL, Marcum ZA (2011) A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother 9(1):12
Hehlmann R, Berger U, Pfirrmann M, Hochhaus A, Metzgeroth G, Maywald O et al (2003) Randomized comparison of interferon alpha and hydroxyurea with hydroxyurea monotherapy in chronic myeloid leukemia (CML-study II): prolongation of survival by the combination of interferon alpha and hydroxyurea. Leukemia 17(8):1529–1537
Hehlmann R, Berger U, Pfirrmann M, Heimpel H, Hochhaus A, Hasford J et al (2007) Drug treatment is superior to allografting as first-line therapy in chronic myeloid leukemia. Blood 109(11): 4686–4692
Hehlmann R, Lauseker M, Jung-Munkwitz S, Leitner A, Muller MC, Pletsch N et al (2011) Tolerability-adapted imatinib 800 mg/d versus 400 mg/d versus 400 mg/d plus interferon-alpha in newly diagnosed chronic myeloid leukemia. J Clin Oncol 29(12): 1634–1642
Hirji I, Gupta S, Goren A, Chirovsky DR, Moadel AB, Olavarria E et al (2013) Chronic myeloid leukemia (CML): association of treatment satisfaction, negative medication experience and treatment restrictions with health outcomes, from the patient’s perspective. Health Qual Life Outcomes 11:167
Hoffmann VS, Baccarani M, Hasford J, Lindoerfer D, Burgstaller S, Sertic D et al (2015) The EUTOS population-based registry: incidence and clinical characteristics of 2904 CML patients in 20 European Countries. Leukemia 29(6):1336–1343
Hoglund M, Sandin F, Hellstrom K, Bjoreman M, Bjorkholm M, Brune M et al (2013) Tyrosine kinase inhibitor usage, treatment outcome, and prognostic scores in CML: report from the population-based Swedish CML registry. Blood 122(7): 1284–1292.
Howlader N, Noone A, Krapcho M, Garshell J, Miller D, Altekruse S et al (2015) SEER cancer statistics review, 1975–2012. National Cancer Institute, Bethesda, MD. http://seer.cancer.gov/csr/1975_2012/
Joosten EA, DeFuentes-Merillas L, De Weert G, Sensky T, Van Der Staak C, de Jong CA (2008) Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychother Psychosom 77(4):219–226
Kapoor J, Agrawal N, Ahmed R, Sharma SK, Gupta A, Bhurani D (2015) Factors influencing adherence to imatinib in indian chronic myeloid leukemia patients: a cross-sectional study. Mediterr J Hematol Infect Dis 7(1): e2015013
Kekale M, Talvensaari K, Koskenvesa P, Porkka K, Airaksinen M (2014) Chronic myeloid leukemia patients’ adherence to peroral tyrosine kinase inhibitors compared with adherence as estimated by their physicians. Patient Preference Adherence 8:1619–1627
Le CT (1998) Applied categorical data analysis. Wiley, New York
Marin D, Bazeos A, Mahon FX, Eliasson L, Milojkovic D, Bua M et al (2010) Adherence is the critical factor for achieving molecular responses in patients with chronic myeloid leukemia who achieve complete cytogenetic responses on imatinib. J Clin Oncol 28(14):2381–2388
Morisky DE, Ang A, Krousel-Wood M, Ward HJ (2008) Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens 10(5):348–354
Noens L, van Lierde MA, De Bock R, Verhoef G, Zachee P, Berneman Z et al (2009) Prevalence, determinants, and outcomes of nonadherence to imatinib therapy in patients with chronic myeloid leukemia: the ADAGIO study. Blood 113(22): 5401–5411
Noens L, Hensen M, Kucmin-Bemelmans I, Lofgren C, Gilloteau I, Vrijens B (2014) Measurement of adherence to BCR-ABL inhibitor therapy in chronic myeloid leukemia: current situation and future challenges. Haematologica 99(3): 437–447
Sabaté E (2003) Adherence to long-term therapies: evidence for action. WHO Library Cataloguing-in-Publication Data, Geneva
Vermeire E, Hearnshaw H, Van Royen P, Denekens J (2001) Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther 26(5):331–342
Author contribution
JG designed research, performed research, collected data, analyzed and interpreted data, and wrote manuscript; GS designed research, performed research, collected data, analyzed and interpreted data; FB collected data; MD collected data; JJ collected data; TG collected data; JP collected data; ED collected data; JH analyzed and interpreted data, and wrote the manuscript; VSH performed statistical analysis, analyzed and interpreted data, and wrote the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Overall support for this project: financial research support from Ariad, BMS, Novartis, Pfizer.
Conflict of interest
Giora Sharf: Patient Advisor of Ariad, Novartis, BMS, Pfizer. Jan Geissler: Patient Advisor of Ariad, Novartis, BMS, Pfizer Mina Daban: Patient Advisor of Ariad, Novartis, BMS, Pfizer, Jana Pelouchova: Patient Advisor of Ariad, BMS, Novartis. Felice Bombaci, Patient Advisor of Ariad, BMS, Novartis, Tony Gavin: Patient Advisor of Roche, Novartis, BMS, Ariad, Pfizer, Celgene, Knapp Pharmaceuticals, Sanofi Aventis, Takeda, Janssen, GSK, Genzyme, Gilead; advisor for NICE (The National Institute for Health & Care Excellence—England & Wales) and AWMSG (The All Wales Medicines Strategy Group).
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Geissler, J., Sharf, G., Bombaci, F. et al. Factors influencing adherence in CML and ways to improvement: Results of a patient-driven survey of 2546 patients in 63 countries. J Cancer Res Clin Oncol 143, 1167–1176 (2017). https://doi.org/10.1007/s00432-017-2372-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-017-2372-z
Keywords
- CML treatment adherence
- Patient-driven survey
- Adherence patient motivations
- Optimal adherence
- Morisky Medication Adherence scale
- Factors causing nonadherence
- Tyrosine kinase inhibitors
- Molecular response
- Driving factors of nonadherence
- Haematology
- Chronic myeloid leukaemia
- Patient advocacy
- Behavioural patterns of adherence