Abstract
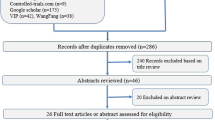
Nasal high-frequency oscillatory ventilation (NHFOV) is a new respiratory support strategy despite lacking of enough evidence in preterm infants with respiratory distress syndrome (RDS). The aim of the present systematic review was to explore whether NHFOV reduced the intubation rate as compared with nasal continuous positive airway pressure (NCPAP) as the primary respiratory support strategies in preterm infants with RDS. Medline, the Cochrane library, the Cochrane Controlled Trials Register, EMBASE, Chinese National Knowledge Infrastructure (CNKI), and Wanfang data Information Site were searched from inception to Jan 1, 2021(Prospero2019 CRD42019129316, date and name of registration: Apr 23,2019, The clinical effectiveness of NHFOV vs NCPAP for preterm babies with respiratory distress syndrome). Pooled data from clinically randomized controlled trials (RCTs) comparing NHFOV with NCPAP as the primary respiratory supporting strategies in preterm infants with RDS were performed using the fixed-effects models whenever no heterogeneity was shown. The primary outcome was intubation rate. Four randomized controlled trials involving 570 participants were included. Comparing with NCPAP, NHFOV resulted in less intubation (relative risk (RR) 0.44; 95% confidence interval (CI) 0.29–0.67, P = 0.0002), and heterogeneity was not found among the trials in the fixed-effects model (P = 0.78, I2 = 0%). Similar result also appeared in sensitivity analysis after excluding one study with significant difference (RR 0.44; 95% CI 0.25–0.78, P = 0.005) (P = 0.58, I2 = 0%).
Conclusion: NHFOV decreased the intubation rate as compared with NCPAP as primary respiratory supporting strategies in preterm infants suffering from RDS. Future research should assess whether NHFOV can reduce the incidence of bronchopulmonary dysplasia (BPD) and intubation rate in preterm infants with BPD. Fund by Natural Science Foundation of Chongqing (cstc2020jcyj-msxmX0197), and “guan’ai” preterm Study Program of Renze Foundation of Beijing(K022).
What is Known: • Nasal high-frequency oscillatory ventilation (NHFOV) has been described to be another advanced version of nasal continuous positive airway pressure (NCPAP). However, its beneficial effects among different studies as the primary modes in the early life of preterm infants with respiratory distress syndrome (RDS) were inconsistent. | |
What is New: • Comparing with NCPAP, NHFOV decreases the risk of intubation as a primary respiratory supporting strategy in early life for preterm infants suffering from RDS. |




Similar content being viewed by others
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- BPD:
-
Bronchopulmonary dysplasia
- CMV:
-
Conventional mechanical ventilation
- IV:
-
Invasive ventilation
- IVH:
-
Intraventricular hemorrhage
- NEC:
-
Necrotizing enterocolitis
- NCPAP:
-
Nasal continuous positive airway pressure
- NIPPV:
-
Nasal intermittent positive pressure ventilation
- NHFOV:
-
Nasal high-frequency oscillatory ventilation
- PVL:
-
Periventricular leukomalacia
- ROP:
-
Retinopathy of prematurity
- RDS:
-
Respiratory distress syndrome
References
Blencowe H, Cousens S, Oestergaard MZ et al (2012) National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet 379(9832):2162–2172. https://doi.org/10.1016/S0140-6736(12)60820-4
Stoll BJ, Hansen NI, Bell EF et al (2010) Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 126(3):443–456. https://doi.org/10.1542/peds.2009-2959
Smith VC, Zupancic JA, McCormick MC et al (2004) Rehospitalization in the first year of life among infants with bronchopulmonary dysplasia. J Pediatr 144(6):799–803. https://doi.org/10.1016/j.jpeds.2004.03.026
Schmidt B, Asztalos EV, Roberts RS et al (2003) Impact of bronchopulmonary dysplasia, brain injury, and severe retinopathy on the outcome of extremely low-birth-weight infants at 18 months: results from the trial of indomethacin prophylaxis in preterms. JAMA 289(9):1124–9. https://doi.org/10.1001/jama.289.9.1124
Kirpalani H, Millar D, Lemyre B et al (2013) A trial comparing noninvasive ventilation strategies in preterm infants. N Engl J Med 369(7):611–20. https://doi.org/10.1056/NEJMoa1214533
Chen L, Wang L, Li J, Wang N, Shi Y (2015) Noninvasive ventilation for preterm twin neonates with respiratory distress syndrome: a randomized controlled trial. Sci Rep 5:14483. https://doi.org/10.1038/srep14483
Lemyre B, Davis PG, De Paoli AG, Kirpalani H (2017) Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for preterm neonates after extubation. Cochrane Database Syst Rev 2:CD003212. https://doi.org/10.1002/14651858.CD003212.pub3
Lemyre B, Laughon M, Bose C, Davis PG (2016) Early nasal intermittent positive pressure ventilation (NIPPV) versus early nasal continuous positive airway pressure (NCPAP) for preterm infants. Cochrane Database Syst Rev 12:CD005384. https://doi.org/10.1002/14651858.CD005384.pub2
De Luca D, Carnielli VP, Conti G, Piastra M (2010) Noninvasive high frequency oscillatory ventilation through nasal prongs: bench evaluation of efficacy and mechanics. Intensive Care Med 36(12):2094–2100. https://doi.org/10.1007/s00134-010-2054-7
De Luca D, Piastra M, Pietrini D, Conti G (2012) Effect of amplitude and inspiratory time in a bench model of non-invasive HFOV through nasal prongs. Pediatr Pulmonol 47(10):1012–1018. https://doi.org/10.1002/ppul.22511
De Luca D, Costa R, Visconti F, Piastra M, Conti G (2016) Oscillation transmission and volume delivery during face mask-delivered HFOV in infants: bench and in vivo study. Pediatr Pulmonol 51(7):705–712. https://doi.org/10.1002/ppul.23403
Mukerji A, Singh B, Helou SE et al (2018) Use of noninvasive high-frequency ventilation in the neonatal intensive care unit: a retrospective review. Am J Perinatol 30(2):171–176. https://doi.org/10.1055/s-0034-1381317
Bottino R, Pontiggia F, Ricci C et al (2018) Nasal high-frequency oscillatory ventilation and CO2 removal: A randomized controlled crossover trial. Pediatr Pulmonol 53(9):1245–1251. https://doi.org/10.1002/ppul.24120
Mukerji A, Sarmiento K, Lee B, Hassall K, Shah V (2017) Non-invasive high-frequency ventilation versus bi-phasic continuous positive airway pressure(BP-CPAP) following CPAP failure in infants <1250g: a pilot randomized controlled trial. J Perinatol 37:49–53. https://doi.org/10.1038/jp.2016.172
Hoehn T, Krause MF (2000) Effective elimination of carbon dioxide by nasopharyngeal high-frequency ventilation. Respir Med 94(11):1132–1134. https://doi.org/10.1053/rmed.2000.0889
Fisher HS, Bohlin K, Buhrer C et al (2015) Nasal high-frequency oscillation ventilation in neonates: a survey in five European Countries. Eur J Pediatr 174:465–71. https://doi.org/10.1007/s00431-014-2419-y
Zhu XW, Zhao JN, Tang SF, Yan J, Shi Y (2017) Noninvasive high-frequency oscillatory ventilation versus nasal continuous positive airway pressure in preterm infants with moderate-severe respiratory distress syndrome: a preliminary report. Pediatr Pulmonol 52(8):1038–42. https://doi.org/10.1002/ppul.23755
Zhu XW, Feng ZC, Liu CJ et al (2021) Noninvasive high frequency oscillatory ventilation versus nasal continuous positive airway pressure in preterm infants with respiratory distress syndrome: a multi-center, prospective, randomized, controlled clinical superior trial. Neonatology 1–7. https://doi.org/10.1159/000515226. Online ahead of print.
Malakian A, Bashirnezhadkhabaz S, Aramesh MR, Dehdashtian M (2020) Noninvasive high-frequency oscillatory ventilation versus nasal continuous positive airway pressure in preterm infants with respiratory distress syndrome: a randomized controlled trial. J Matern Fetal Neonatal Med 33(15):2601–7. https://doi.org/10.1080/14767058.2018.1555810
Moher D, Liberati A, Tetzlaff J et al (2019) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Jobe AH, Bancalari E (2001) Bronchopulmonary dysplasia. Am J RespirCrit Care Med 163:1723-1729
Stoll BJ (1994) Epidemiology of necrotizing enterocolitis. Clin Perinatol 21(2):205–218
Long C, Li W, Wanwei L, Jie L, Yuan S (2016) Noninvasive ventilation with heliox for respiratory distress syndrome in preterm infant:a systematic review and meta-analysis. Can Respir J 9092871. https://doi.org/10.1155/2016/9092871
Zhu XW, Shi Y, Shi LP et al (2018) Non-invasive high-frequency oscillatory ventilation versus nasal continuous positive airway pressure in preterm infants with respiratory distress syndrome: study protocol for a multi-center prospective randomized controlled trial. Trials 19(1):319. https://doi.org/10.1186/s13063-018-2673-9
Zhu XW, Yan J, Ran Q et al (2017) Noninvasive high-frequency oscillatory ventilation versus for respiratory distress syndrome in preterm infants: a preliminary report. Chin J Neonatol 32:291–294. (In Chinese) https://doi.org/10.3760/cma.j.issn.2096-2932.2017.04.012
Long Chen, Li Wang, Juan Ma, Zhichun Feng, Jie Li, Yuan S (2019) Nasal high-frequency oscillatory ventilation in preterm infants with respiratory distress syndrome(RDS) and acute respiratory distress syndrome(ARDS) after extubation: a randomized controlled trial. Chest 155(4):740–748. https://doi.org/10.1016/j.chest.2019.01.014
Lou WB, Zhang WX (2017) Noninvasive high-frequency oscillatory ventilation versus nasal continuous positive airway pressure in premature infants with respiratory distress syndrome after weaning: a randomized controlled trial. Guangdong Med J 38:2037-40. (In Chinese)
Fischer HS, Bührer C, Czernik C (2019) Hazards to avoid in future neonatal studies of nasal high-frequency oscillatory ventilation: lessons from an early terminated trial. BMC Res Notes 12(1):237. https://doi.org/10.1186/s13104-019-4268-2
Klotz D, Schneider H, Schumann S et al (2018) Non-invasive high-frequency oscillatory ventilation in preterm infants: a randomised controlled cross-over trial. Arch Dis Child Fetal Neonatal Ed 103:1–5. https://doi.org/10.1136/archdischild-2017-313190
Rüegger CM, Lorenz L, Kamlin COF et al (2018) The effects of noninvasive high-frequency oscillatory ventilation on desaturations and bradycardia in very preterm infants: a randomized crossover trial. J Pediatr 201:269–273.e2. https://doi.org/10.1016/j.jpeds.2018.05.029
Lou WB, Zhang WX, Yuan L, Zhang B (2018) Comparative study of noninvasive high-frequency oscillatory ventilation and bilevel positive airway pressure ventilation for preterm infants with respiratory distress syndrome. Chinese Gen Prac 21:1983–1988.(In Chinese)
Iranpour R, Armanian AM, Abedi AR, Farajzadegan Z (2019) Nasal high-frequency ventilation (NHFV) versus nasal continuous positive airway pressure (NCPAP) as an initial therapy for respiratory distress syndrome (RDS) in preterm newborns. BMJ Pediatrics Open 3:e000443. https://doi.org/10.1136/bmjpo-2019-000443
van der Hoeven M, Brouwer E, Blanco CE (1998) Nasal high frequency ventilation in neonates with moderate respiratory insufficiency. Arch Dis Child Fetal Neonatal Ed 79(1):F61–F63. https://doi.org/10.1136/fn.79.1.f61
Li J, Li X, Huang X, Zhang Z (2019) Noninvasive high-frequency oscillatory ventilation as respiratory support in preterm infants: a meta-analysis of randomized controlled trials. Respir Res 20(1):58. https://doi.org/10.1186/s12931-019-1023-0
Wang CH, Shi LP, Ma XL et al (2017) Use of noninvasive high frequency oscillatory ventilation in very low birth weight infants. Zhonghua Er Ke Za Zhi 55(3):177–181. https://doi.org/10.3760/cma.j.issn.0578-1310.2017.03.003
Gaertner VD, Waldmann AD, Davis PG et al (2021) Transmission of oscillatory volumes into the preterm lung during noninvasive high-frequency ventilation. Am J Respir Crit Care Med 203(8):998–1005.
Czernik C, Schmalisch G, Bührer C, Proquitté H (2012) Weaning of neonates from mechanical ventilation by use of nasopharyngeal high-frequency oscillatory ventilation: a preliminary study. J Matern Fetal Neonatal Med 25(4):374–378. https://doi.org/10.3109/14767058.2011.580401
Schäfer C, Schumann S, Fuchs H, Klotz D (2019) Carbon dioxide diffusion coefficient in noninvasive high-frequency oscillatory ventilation. Pediatr Pulmonol 54(6):759–764
Bottino R, Pontiggia F, Ricci C et al (2018) Nasal high-frequency oscillatory ventilation and CO 2 removal: a randomized controlled crossover trial. Pediatr Pulmonol 53:1245–1251
Ullrich TL, Czernik C, Bührer C, Schmalisch G, Fischer HS (2017) Nasal high-frequency oscillatory ventilation impairs heated humidification: a neonatal bench study. Pediatr Pulmonol 52(11):1455–1460
De Luca D, Shankar-Aguilera S, Centorrino R, Fortas F, Yousef N, Carnielli VP (2020) Less invasive surfactant administration: a word of caution. Lancet Child Adolesc Health 4(4):331–340
Funding
Natural Science Foundation of Chongqing (cstc2020jcyj-msxmX0197) and “guan’ai” preterm Study Program of Renze Foundation of Beijing (K022).
Author information
Authors and Affiliations
Contributions
Li Jie: Dr. Li accomplished the article-extracting and data analysis, drafted the initial manuscript, and reviewed the manuscript. Chen Long: Dr. Chen conceptualized and designed the study, accomplished the article-extracting and data analysis, and revised the initial manuscript. Shi Yuan: Dr. Shi conceptualized and designed the study, accomplished the article-extracting and data analysis, and critically reviewed the manuscript for important intellectual content. All the authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, J., Chen, L. & Shi, Y. Nasal high-frequency oscillatory ventilation versus nasal continuous positive airway pressure as primary respiratory support strategies for respiratory distress syndrome in preterm infants: a systematic review and meta-analysis. Eur J Pediatr 181, 215–223 (2022). https://doi.org/10.1007/s00431-021-04190-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-04190-0