Abstract
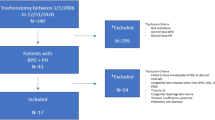
Neonatologist-performed echocardiography (NPE) is an established tool for bedside hemodynamic evaluation, including pulmonary hypertension (PH). PH may complicate bronchopulmonary dysplasia (BPD) course. Aims of this retrospective study were to assess the feasibility of NPE follow-up of infants with BPD and to describe the course of PH of infants with moderate/severe BPD. Preterm infants <32 gestational weeks or birthweight ≤1500 g with moderate/severe BPD underwent NPE follow-up, from 36 weeks postmenstrual age up to 8 months postnatal age. Twenty-three preemies were included (birth weight 840 (213) g, gestational age 26.8 (2.3) weeks); 12/23 developed mild PH, 2/12 after discharge. PH resolved at 8.9 (3.9) months. Clinical and echocardiographic variables did not differ between infants with and without PH, except pulmonary artery acceleration time (PAAT) and PAAT/right ventricle ejection time (RVET) ratio (PAAT: 36 weeks, 68.9 (11.9) vs 52.0 (19.1), p = 0.0443; 6 months: 83.9 (38.9) vs 74.8 (16.9), p = 0.0372). No deaths or admissions for PH were reported. Neonatologist’s Image Quality Assessment score attributed by the cardiologist assumed as gold standard was adequate or optimal (9.5/14 total score); inter-rater agreement was excellent (ICC 0.974).
Conclusions: NPE follow-up seems to be feasible and safe in both intensive care and outpatient clinic. Mild PH is frequently detected in moderate/severe BPD, with good prognosis.
What is Known: • Preterm infants with bronchopulmonary dysplasia (BPD) may develop pulmonary hypertension (PH) and have a late diagnosis. • Neonatologist-performed echocardiography (NPE) is an established tool for bedside hemodynamic evaluation of the neonate. | |
What is New: • To our knowledge this is the first study of NPE follow-up of moderate/severe BPD, describing the course of mild PH from diagnosis to its resolution. • NPE follow-up of BPD seems to be safe and practicable, in both intensive care and outpatient clinic, as long as neonatologists maintain a sound collaboration with pediatric cardiologists. |
Similar content being viewed by others
Data availability
The research data is confidential.
Abbreviations
- BPD:
-
Bronchopulmonary dysplasia
- CHD:
-
Congenital heart disease
- E’:
-
Peak early diastolic tissue velocity
- LV:
-
Left ventricle
- NICU:
-
Neonatal intensive care unit
- NPE:
-
Neonatologist-performed echocardiography
- PA:
-
Postnatal age
- PAAT:
-
Pulmonary artery acceleration time
- PDA:
-
Patent ductus arteriosus
- PH:
-
Pulmonary hypertension
- PMA:
-
Postmenstrual age
- PVD:
-
Pulmonary vascular disease
- RV:
-
Right ventricle
- RVET:
-
Right ventricle ejection time
- TV:
-
Tricuspid valve
References
Mourani PM, Abman SH (2010) Pulmonary vascular disease in bronchopulmonary dysplasia: physiology, diagnosis, and treatment. In: Abman SH (ed) Bronchopulmonary dysplasia. Informa Healthcare, New York, pp 347–363
Del Cerro MJ, Sabaté Rotés A, Cartón A, Deiros L, Bret M, Cordeiro M, Verdú C, Barrios MI, Albajara L, Gutierrez-Larraya F (2014) Pulmonary hypertension in bronchopulmonary dysplasia: clinical findings, cardiovascular anomalies and outcomes. Pediatr Pulmonol 49:49–59. https://doi.org/10.1002/ppul.227977
Singh Y, Tissot C, Fraga MV, Yousef N, Cortes RG, Lopez J, Sanchez-de-Toledo J, Brierley J, Colunga JM, Raffaj D, da Cruz E, Durand P, Kenderessy P, Lang HJ, Nishisaki A, Kneyber MC, Tissieres P, Conlon TW, de Luca D (2019) International evidence-based guidelines on point of care ultrasound (POCUS) for critically ill neonates and children issued by the POCUS Working Group of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC). Crit Care 24(1):65. https://doi.org/10.1186/s13054-020-2787-9
Groves AM, Singh Y, Dempsey E, Molnar Z, Austin T, El-Khuffash A, de Boode WP, European Special Interest Group ‘Neonatologist Performed Echocardiography’ (NPE) (2018) Introduction to neonatologist-performed echocardiography. Pediatr Res 84(Suppl 1):1–12. https://doi.org/10.1038/s41390-018-0076-y
de Boode WP, Singh Y, Gupta S, Austin T, Bohlin K, Dempsey E, Groves A, Eriksen BH, van Laere D, Molnar Z, Nestaas E, Rogerson S, Schubert U, Tissot C, van der Lee R, van Overmeire B, el-Khuffash A (2016) Recommendations for neonatologist performed echocardiography in Europe: consensus statement endorsed by European Society for Paediatric Research (ESPR) and European Society for Neonatology (ESN). Pediatr 80(4):465–471. https://doi.org/10.1038/pr.2016.126
Mertens L, Seri I, Marek J, Arlettaz R, Barker P, McNamara P, Moon-Grady AJ, Coon PD, Noori S, Simpson J et al (2011) Targeted neonatal echocardiography in the neonatal intensive care unit: practice guidelines and recommendations for training. Writing Group of the American Society of Echocardiography (ASE) in collaboration with the European Association of Echocardiography (EAE) and the Association for European Pediatric Cardiologists (AEPC). J Am Soc Echocardiogr 24(10):1057–1078. https://doi.org/10.1093/ejechocard/jer181
Jobe AH, Bancalari E (2001) Bronchopulmonary dysplasia. Am J Respir Crit Care Med 163:1723–1729. https://doi.org/10.1164/ajrccm.163.7.2011060
Copetti R, Cattarossi L, Macagno F, Violino M, Furlan R (2008) Lung ultrasound in respiratory distress syndrome: a useful tool for early diagnosis. Neonatology 94(1):52–59. https://doi.org/10.1159/000113059
Cummings JJ, Polin RA, AAP Committee on fetus and newborn (2016) Oxygen targeting in extremely low birth weight infants. Pediatrics 138:e20161576. https://doi.org/10.1542/peds.2016-29044
Allen J, Zwerdling R, Ehrenkranz R, Gaultier C, Geggel R, Greenough A, Kleinman R, Klijanowicz A, Martinez F, Ozdemir A, Panitch HB, Nickerson B, Stein MT, Tomezsko J, van der Anker J, American Thoracic Society (2003) Statement on the care of the child with chronic lung disease of infancy and childhood. Am J Respir Crit Care Med 168:356–396. https://doi.org/10.1164/rccm.168.3.356
Balfour-Lynn IM, Field DJ, Gringras P, Hicks B, Jardine E, Jones RC, Magee AG, Primhak RA, Samuels MP, Shaw NJ et al (2009) BTS guidelines for home oxygen in children. Thorax 64(Suppl 2):ii1–i26. https://doi.org/10.1136/thx.2009.116020
Bertino E, Spada E, Occhi L, Coscia A, Giuliani F, Gagliardi L, Gilli G, Bona G, Fabris C, De Curtis M et al (2010) Neonatal anthropometic charts: the Italian neonatal study compared with other European studies. J Pediatr Gastroenterol Nutr 51(3):353–361. https://doi.org/10.1097/MPG.0b013e3181da213e
Nestaas E, Schubert U, de Boode WP, El-Khuffash A, European Special Interest Group ‘Neonatologist Performed Echocardiography’ (NPE) (2018) Tissue Doppler velocity imaging and event timings in neonates: a guide to image acquisition, measurement, interpretation, and reference values. Pediatr Res 84(Suppl 1):18–29. https://doi.org/10.1038/s41390-018-0079-8
Levy PT, Patel MD, Groh G, Choudhry S, Murphy J, Holland MR, Hamvas A, Grady MR, Singh GK (2016) Pulmonary artery acceleration time provides a reliable estimate of invasive pulmonary hemodynamics in children. J Am Soc Echocardiogr 29(11):1056–1065. https://doi.org/10.1016/j.echo.2016.08.013
McQuillian BM, Picard MH, Leavitt M, Weyman AE (2001) Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation 104:2797–2802. https://doi.org/10.1161/hc4801.100076
De Boode WP, Singh Y, Molnar Z, Schubert U, Savoia M, Sehgal A, Levy PT, PJ MN, El-Khuffash A, European Special Interest Group ‘Neonatologist Performed Echocardiography’ (NPE) (2018) Application of neonatologist performed echocardiography in the assessment and management of persistent pulmonary hypertension of the newborn. Pediatr Res 84(Suppl 1):68–77. https://doi.org/10.1038/s41390-018-0082-0
Mourani PM, Sontag MK, Younoszai A, Miller JI, Kinsella JP, Baker CD, Poindexter BB, Ingram DA, Abman SH (2015) Early pulmonary vascular disease in preterm infants at risk for bronchopulmonary dysplasia. Am J Respir Crit Care Med 191(1):87–95. https://doi.org/10.1164/rccm.201409-1594OC
King ME, Braun H, Goldblatt A, Liberthson R, Weyman AE (1983) Interventricular septal configuration as a predictor of right ventricular systolic hypertension in children: a cross-sectional echocardiographic study. Circulation 68:68–75. https://doi.org/10.1161/01.CIR.68.1.68
Lopez L, Colan S, Stylianou M, Granger S, Trachtenberg F, Frommelt P, Pearson G, Camarda J, Cnota J, Cohen M, Dragulescu A, Pediatric Heart Network Investigators et al (2017) Relationship of echocardiographic Z scores adjusted for body surface area to age, sex, race, and ethnicity the Pediatric Heart Network Normal Echocardiogram Database. Circ Cardiovasc Imaging 10(11):e006979. https://doi.org/10.1161/CIRCIMAGING.117.006979
Kampann C, Wiethoff CM, Wenzel A, Stolz G, Betancor M, Wippermann CF, Huth RG, Habermehl P, Knuf M, Emschermann T et al (2000) Normal values of M mode echocardiographic measurements of more than 2000 healthy infants and children in central Europe. Heart 83(6):667–672. https://doi.org/10.1136/heart.83.6.667
Cantinotti M, Scalese M, Murzi B, Assanta N, Spadoni I, De Lucia V, Crocetti M, Cresti A, Gallotta M, Marotta M et al (2014) Echocardiographic nomograms for chamber diameters and areas in Caucasian children. J Am Soc Echocardiogr 27(12):1279–92.e2. https://doi.org/10.1016/j.echo.2014.08.005
Lopez L, ACPC Section’s Quality Metrics Work Group (2018) Initial transthoracic echocardiogram image quality. Amerian College of Cardiology Quality Improvement for Institutions Program https://cvquality.acc.org/initiatives/acpc-quality-network/quality-metrics. Accessed 12 Oct 2020
Buting KV, Steeds RP, Slater LT, Rogers JK, Gkoutos GV, Kotecha D (2019) A practical guide to assess the reproducibility of echocardiographic measurements. J Am Soc Echocardiogr 32(12):1505–1515. https://doi.org/10.1016/j.echo.2019.08.015
McNamara P, Lai W (2020) Growth of neonatal hemodynamics programs and targeted neonatal echocardiography performed by neonatologists. J Am Soc Echocardiogr 33(10):A15–A16. https://doi.org/10.1016/j.echo.2020.08.009
Australasian Society for Ultrasound in Medicine. Certificate in Clinician Performed Ultrasound (CCPU) - Advanced Clinician Performed Neonatal Ultrasound (2018) https://www.asum.com.au/education/ccpu-course. Accessed 12 Oct 2020
Singh Y, Gupta S, Groves AM, Gandhi A, Thomson J, Qureshi S, Simpson JM (2016) Expert consensus statement “neonatologist performed echocardiography (NoPE) – training and accreditation in UK. Eur J Pediatr 175:281–287 https://doi.org/10.1007/s00431-015-2633-2
Targeted Neonatal Echocardiography in Switzerland (2017) https://www.neonet.ch/en/training-courses/echocardiography-tne/. Accessed 12 Oct 2020
Svedenkrans J, Stoecklin B, Jones JG, Doherty DA, Pillow JJ (2019) Physiology and predictors of impaired gas exchange in infants with bronchopulmonary dysplasia. Am J Respir Crit Care Med 200(4):471–480. https://doi.org/10.1164/rccm.201810-2037OC
Mehler K, Udink Ten Cate FE, Keller T, Bangen U, Kribs A, Oberthuer A (2018) An echocardiographic screening program helps to identify pulmonary hypertension in extremely low birthweight infants with and without bronchopulmonary dysplasia: a single-center experience. Neonatology 113:81–88. https://doi.org/10.1159/000480694
Khemani E, McElhinney DB, Rhein L, Andrade O, Lacro RV, Thomas KC, Mullen MP (2007) Pulmonary artery hypertension in formerly premature infants with bronchopulmonary dysplasia: clinical features and outcomes in the surfactant era. Pediatrics 120:1260–1269. https://doi.org/10.1542/peds.2007-0971
Arjaans S, Haarman MG, Roofthooft MTR, Fries MWF, Kooi EMW, Bos AF, Berger RMF (2020) Fate of pulmonary hypertension associated with bronchopulmonary dysplasia beyond 36 weeks postmenstrual age. Arch Dis Child Fetal Neonatal Ed fetalneonatal-2019-318531. https://doi.org/10.1136/archdischild-2019-318531
Mourani PM, Mandell EW, Meier M, Younoszai A, Brinton JT, Wagner BD, Arjaans S, Poindexter BB, Abman SH (2018) Early pulmonary vascular disease in preterm infants is associated with late respiratory outcomes in childhood. Am J Respir Crit Care Med 199:1020–1027. https://doi.org/10.1164/rccm.201803-0428OC
Koestenberger M, Grangl G, Avian A, Gamillscheg A, Grillitsch M, Cvirn G, Burmas A, Hansmann G (2017) Normal reference values and z scores of the pulmonary artery acceleration time in children and its importance for the assessment of pulmonary hypertension. Circ Cardiovasc Imaging 10(1):e005336. https://doi.org/10.1161/CIRCIMAGING.116.005336
Nagiub M, Lee S, Guglani L (2015) Echocardiographic assessment of pulmonary hypertension in infants with bronchopulmonary dysplasia: systematic review of literature and a proposed algorithm for assessment. Echocardiography. 32(5):819–833. https://doi.org/10.1111/echo.12738
Patel MD, Breatnach CR, James AT, Choudhry S, McNamara PJ, Jain A, Franklin O, Hamvas A, Mertens L, Singh GK, El-Khuffash A, Levy PT (2019) Echocardiographic assessment of right ventricular afterload in preterm infants: maturational patterns of pulmonary artery acceleration time over the first year of age and implications for pulmonary hypertension. J Am Soc Echocardiogr 32(7):884–894.e4. https://doi.org/10.1016/j.echo.2019.03.015
Levy PT, Patel MD, Choudhry S, Hamvas A, Singh GK (2018) Evidence of echocardiographic markers of pulmonary vascular disease in asymptomatic infants born preterm at one year of age. J Pediatr 197:48–56.e2. https://doi.org/10.1016/j.jpeds.2018.02.006
Di Maria MV, Younoszai AK, Sontag MK, Miller JI, Poindexter BB, Ingram DA, Abman SH, Mourani PM (2015) Maturational changes in diastolic longitudinal myocardial velocity in preterm infants. J Am Soc Echocardiogr 28:1045–1052. https://doi.org/10.1016/j.echo.2015.04.016
Negrine RJ, Chikermane A, Wright JG, Ewer AK (2012) Assessment of myocardial function in neonates using tissue Doppler imaging. Arch Dis Child Fetal Neonatal Ed 97(4):F304–F306. https://doi.org/10.1136/adc.2009.175109
Roberson DA, Cui W, Chen Z, Madronero LF, Cuneo BF (2007) Annular and septal Doppler tissue imaging in children: normal z-score tables and effects of age, heart rate, and body surface area. J Am Soc Echocardiogr 20:1276–1284. https://doi.org/10.1016/j.echo.2007.02.023
Eidem BW, McMahon CJ, Cohen RR, Wu J, Finkelshteyn I, Kovalchin JP, Ayres NA, Bezold LI, O'Brian Smith E, Pignatelli RH (2004) Impact of cardiac growth on Doppler tissue imaging velocities: a study in healthy children. J Am Soc Echocardiogr 17:212–221. https://doi.org/10.1016/j.echo.2003.12.005
Eriksen BH, Nestaas E, Hole T, Liestøl K, Støylen A, Fugelseth D (2014) Myocardial function in term and preterm infants. Influence of heart size, gestational age and postnatal maturation. Early Hum Dev 90(7):359–364. https://doi.org/10.1016/j.earlhumdev.2014.04.010
Breatnach CR, El-Khuffash A, James A, McCallion N, Franklin O (2017) Serial measures of cardiac performance using tissue Doppler imaging velocity in preterm infants <29weeks gestations. Early Hum Dev 108:33–39. https://doi.org/10.1016/j.earlhumdev.2017.03.012
El-Khuffash A, Schubert U, Levy PT, Nestaas E, de Boode WP, European Special Interest Group ‘Neonatologist Performed Echocardiography’ (NPE) (2018) Deformation imaging and rotational mechanics in neonates: a guide to image acquisition, measurement, interpretation, and reference values. Pediatr Res 84(Suppl 1):30–45. https://doi.org/10.1038/s41390-018-0080-2
Levy PT, El-Khuffash A, Patel MD, Breatnach CR, James AT, Sanchez AA, Abuchabe C, Rogal SR, Holland MR, McNamara PJ et al (2017) Maturational patterns of systolic ventricular deformation mechanics by two-dimensional speckle-tracking echocardiography in preterm infants over the first year of age. J Am Soc Echocardiogr 30(7):685–698.e1. https://doi.org/10.1016/j.echo.2017.03.003
Author information
Authors and Affiliations
Contributions
MS designed the study, performed the data collection and analysis, drafted the manuscript, and approved the final manuscript as submitted. LC performed statistical analysis and participated to data analysis. AT, FRM, DP, PF, and LC participated to data collection and were involved in data analysis. PM participated to study design and made critical revisions to the final manuscript. All authors were involved in the production of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The study received approval from the Ethical Committee of the Friuli Venezia Giulia region, Udine, Italy (Approval No. CEUR-2018-OS-119-ASUIUD).
Consent to participate
Not applicable
Consent for publication
Not applicable
Code availability
Not applicable
Additional information
Communicated by Daniele De Luca
There are no prior publications or submissions with any overlapping information, including studies and patients. Preliminary results were presented as abstract at the 6th Congress of the European Academy of Pediatric Societies (EAPS 2016), Geneva (Switzerland) October 21–25, 2016.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 24 kb)
Rights and permissions
About this article
Cite this article
Savoia, M., Morassutti, F.R., Castriotta, L. et al. Pulmonary hypertension in a neonatologist-performed echocardiographic follow-up of bronchopulmonary dysplasia. Eur J Pediatr 180, 1711–1720 (2021). https://doi.org/10.1007/s00431-021-03954-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-03954-y