Abstract
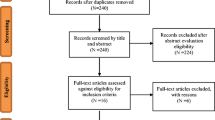
This meta-analysis was performed to clarify the association between food hypersensitivity in children and autism spectrum disorder (ASD) in detail. Relevant studies published in 8 databases before March 2020 were retrieved and screened according to established inclusion criteria. The odds ratio (OR) with the 95% confidence interval (CI) was pooled to estimate the effect. Subgroup analyses were performed in terms of publication year, study design, location, sample size, definition of food hypersensitivity, definition of ASD, and study quality score. Furthermore, we stratified studies by participant sex and age to perform a more detailed analysis. This meta-analysis included 12 published articles with 434,809 subjects. A significant association was observed between food hypersensitivity and the risk of ASD (OR = 2.792, 95% CI: 2.081–3.746). The risk of ASD among girls and subjects younger than 12 with food hypersensitivity may be greater than that among boys and those older than 12. The results of sensitivity analysis and publication bias analysis show that the association is relatively stable.
Conclusion: Our results showed a positive association between food hypersensitivity and autism spectrum disorder, and girls and subjects younger than 12 may be more sensitive to this association. The role of food hypersensitivity in the onset of ASD deserves more attention.
What is Known: • Food hypersensitivity is a term used to describe food allergies and food intolerance. • ASD is a group of neurodevelopmental disorders that are characterized by deficits in social interaction, repetitive or stereotypic behavior, and verbal communication disorder. • The prevalence rates of ASD and food hypersensitivity in the developed world are increasing. | |
What is New: • In this work, we reviewed and analyzed the available data and studies and found a positive association between food hypersensitivity and ASD. • Girls and children younger than 12 may be more sensitive to have ASD than boys and children older than 12. |


Similar content being viewed by others
Abbreviations
- AHRQ:
-
Agency for Healthcare Research and Quality
- ABC:
-
Autism Behavior Checklist
- ADI:
-
Autism Diagnostic Interview
- ADI-R:
-
Autism Diagnostic Interview-Revised
- ADOS:
-
Autism Diagnostic Observation Schedule
- ASD:
-
Autism spectrum disorder
- CARS:
-
Childhood Autism Rating Scale
- CBM:
-
China Biology Medicine disc/Sinomed
- CNKI:
-
China National Knowledge Infrastructure
- CCMD:
-
Chinese diagnostic criteria for mental disorders
- CIs:
-
Confidence intervals
- DSM:
-
Diagnostic and Statistical Manual of Mental Disorders
- FEM:
-
Fixed effects model
- HRs:
-
Hazard ratios
- IL:
-
Interleukin
- ICD:
-
International Statistical Classification of Diseases
- NHIS:
-
National Health Interview Survey
- NOS:
-
Newcastle-Ottawa Scale
- ORs:
-
Odds ratios
- PRISMA:
-
Preferred Reporting Items for Systematic Review and Meta-Analyses
- PRs:
-
Prevalence ratios
- REM:
-
Random effects model
- RRs:
-
Relative risks
- TNF:
-
Tumor necrosis factor
References
Newschaffer CJ, Croen LA, Daniels J et al (2007) The epidemiology of autism spectrum disorders. Annu Rev Public Health 28:235–258. https://doi.org/10.1146/annurev.publhealth.28.021406.144007
Wing L (1981) Sex ratios in early childhood autism and related conditions. Psychiatry Res 5(2):129–137. https://doi.org/10.1016/0165-1781(81)90043-3
Maenner M, Shaw K, Baio J et al (2020) Prevalence of autism spectrum disorder among children aged 8 years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2016. Morbidity and mortality weekly report. Surveill Summaries (Washington, DC : 2002) 69(4):1–12. https://doi.org/10.15585/mmwr.ss6904a1
Chawarska K, Paul R, Klin A, Hannigen S, Dichtel LE, Volkmar F (2007) Parental recognition of developmental problems in toddlers with autism spectrum disorders. J Autism Dev Disord 37(1):62–72. https://doi.org/10.1007/s10803-006-0330-8
Ospina MB, Krebs Seida J, Clark B et al (2008) Behavioural and developmental interventions for autism spectrum disorder: a clinical systematic review. PLoS One 3(11):e3755. https://doi.org/10.1371/journal.pone.0003755
Baxter AJ, Brugha TS, Erskine HE, Scheurer RW, Vos T, Scott JG (2015) The epidemiology and global burden of autism spectrum disorders. Psychol Med 45(3):601–613. https://doi.org/10.1017/s003329171400172x
Christensen DL, Maenner MJ, Bilder D et al (2019) Prevalence and characteristics of autism spectrum disorder among children aged 4 years - Early Autism and Developmental Disabilities Monitoring Network, Seven Sites, United States, 2010, 2012, and 2014. Morbidity and mortality weekly report. Surveill Summaries (Washington, DC : 2002) 68(2):1–19. https://doi.org/10.15585/mmwr.ss6802a1
Xu G, Strathearn L, Liu B, Bao W (2018) Prevalence of autism spectrum disorder among US children and adolescents, 2014–2016. JAMA 319(1):81–82. https://doi.org/10.1001/jama.2017.17812
Xu G, Strathearn L, Liu B et al (2019) Prevalence and treatment patterns of autism spectrum disorder in the United States, 2016. JAMA Pediatr 173(2):153–159. https://doi.org/10.1001/jamapediatrics.2018.4208
Pérez-Crespo L, Prats-Uribe A, Tobias A et al (2019) Temporal and geographical variability of prevalence and incidence of autism spectrum disorder diagnoses in children in Catalonia, Spain. Autism Res 12(11):1693–1705. https://doi.org/10.1002/aur.2172
Buescher AV, Cidav Z, Knapp M, Mandell DS (2014) Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr 168(8):721–728. https://doi.org/10.1001/jamapediatrics.2014.210
Leigh J, Du J (2015) Brief Report: forecasting the economic burden of autism in 2015 and 2025 in the United States. J Autism Dev Disord 45(12):4135–4139. https://doi.org/10.1007/s10803-015-2521-7
Liu Q, Chen M, Sun L et al (2019) Rational use of mesenchymal stem cells in the treatment of autism spectrum disorders. World J Stem Cells 11(2):55–72. https://doi.org/10.4252/wjsc.v11.i2.55
Malek A, Farhang S, Amiri S, Abdi S, Rezaih AR, Asadian M (2019) Risk factors for autistic disorder: a case-control study. Iran J Pediatr 29(3). https://doi.org/10.5812/ijp.80935
Xu G, Snetselaar LG, Jing J, Liu B, Strathearn L, Bao W (2018) Association of food allergy and other allergic conditions with autism spectrum disorder in children. JAMA Netw Open 1(2):e180279–e180e79. https://doi.org/10.1001/jamanetworkopen.2018.0279
Shibata A, Hitomi Y, Kambayashi Y et al (2013) Epidemiological study on the involvements of environmental factors and allergy in child mental health using the Autism Screening Questionnaire. Res Autism Spectr Disord 7(1):132–140. https://doi.org/10.1016/j.rasd.2012.06.003
Lin TY, Lin PY, Su TP et al (2014) Autistic spectrum disorder, attention deficit hyperactivity disorder, and allergy: is there a link? A nationwide study. Res Autism Spectr Disord 8(10):1333–1338. https://doi.org/10.1016/j.rasd.2014.07.009
Lomer MC (2015) Review article: The aetiology, diagnosis, mechanisms and clinical evidence for food intolerance. Aliment Pharmacol Ther 41(3):262–275. https://doi.org/10.1111/apt.13041
Cнerevko NA, Skirnevskaya AV, Rosenstein MY, Novikov PS, Muraveinik OA, Denisov AA (2018) Features of specific food hypersensitivity to dairy and cereal products in children with autism spectrum disorder. Byulleten' Sibirskoi Meditsiny 17(1):159–166. https://doi.org/10.20538/1682-0363-2018-1-159-166
Peretti S, Mariano M, Mazzocchetti C et al (2019) Diet: the keystone of autism spectrum disorder? Nutr Neurosci 22(12):825–839. https://doi.org/10.1080/1028415x.2018.1464819
Harumi J (2009) Food allergy and autism spectrum disorders: is there a link? Curr Allergy Asthma Rep 9(3):194–201. https://doi.org/10.1007/s11882-009-0029-y
Theoharides TC (2013) Is a subtype of autism an allergy of the brain? Clin Ther 35(5):584–591. https://doi.org/10.1016/j.clinthera.2013.04.009
Theoharides T, Valent P, Akin C (2015) Mast cells, mastocytosis, and related disorders. N Engl J Med 373(2):163–172. https://doi.org/10.1056/NEJMra1409760
Angelidou A, Alysandratos K-D, Asadi S et al (2011) Brief report: “Allergic symptoms” in children with autism spectrum disorders. More than meets the eye? J Autism Dev Disord 41(11):1579–1585. https://doi.org/10.1007/s10803-010-1171-z
Petra AI, Panagiotidou S, Hatziagelaki E, Stewart JM, Conti P, Theoharides TC (2015) Gut-microbiota-brain axis and its effect on neuropsychiatric disorders with suspected immune dysregulation. Clin Ther 37(5):984–995. https://doi.org/10.1016/j.clinthera.2015.04.002
Theoharides TC, Stewart JM, Panagiotidou S, Melamed I (2016) Mast cells, brain inflammation and autism. Eur J Pharmacol 778:96–102. https://doi.org/10.1016/j.ejphar.2015.03.086
Enstrom A, Krakowiak P, Onore C et al (2009) Increased IgG4 levels in children with autism disorder. Brain Behav Immun 23(3):389–395. https://doi.org/10.1016/j.bbi.2008.12.005
Theoharides TC, Angelidou A, Alysandratos K-D et al (2012) Mast cell activation and autism. Biochim Biophys Acta (BBA) - Mol Basis Dis 1822(1):34–41. https://doi.org/10.1016/j.bbadis.2010.12.017
Camarata S (2014) Early identification and early intervention in autism spectrum disorders: accurate and effective? Int J Speech-Language Pathol 16(1):1–10. https://doi.org/10.3109/17549507.2013.858773
Tachibana Y, Miyazaki C, Ota E et al (2017) A systematic review and meta-analysis of comprehensive interventions for pre-school children with autism spectrum disorder (ASD). PLoS One 12(12):e0186502. https://doi.org/10.1371/journal.pone.0186502
Higgins J, Thompson S, Deeks J, Altman D (2003) Measuring inconsistency in meta-analyses. BMJ (Clin Res ed) 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Huedo-Medina T, Sánchez-Meca J, Marín-Martínez F, Botella J (2006) Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods 11(2):193–206. https://doi.org/10.1037/1082-989x.11.2.193
Tang W, Hu J, Zhang H, Wu P, He H (2015) Kappa coefficient: a popular measure of rater agreement. Shanghai Arch Psychiatry 27(1):62–67. https://doi.org/10.11919/j.issn.1002-0829.215010
Rostom A, Dubé C, Cranney A et al (2004) Celiac disease. Evidence Reports/Technology. Appendix D. Quality Assessment Forms. Assessments, No. 104. Rockville (MD): Agency for Healthcare Research and Quality (US). Available from: https://www.ncbi.nlm.nih.gov/books/NBK35156/)
Haidich AB (2010) Meta-analysis in medical research. Hippokratia 14(Suppl 1):29–37
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical research ed) 315(7109):629–634
Renzoni E, Beltrami V, Sestini P, Pompella A, Menchetti G, Zappella M (1995) Brief report: Allergological evaluation of children with autism. J Autism Dev Disord 25(3):327–333
Gurney JG, McPheeters ML, Davis MM (2006) Parental report of health conditions and health care use among children with and without autism: National Survey of Children's Health. Arch Pediatr Adolesc Med 160(8):825–830. https://doi.org/10.1001/archpedi.160.8.825
Garg N, Silverberg JI (2014) Association between childhood allergic disease, psychological comorbidity, and injury requiring medical attention. Ann Allergy Asthma Immunol 112(6):525–532. https://doi.org/10.1016/j.anai.2014.03.006
Bresnahan M, Hornig M, Schultz AF et al (2015) Association of maternal report of infant and toddler gastrointestinal symptoms with autism evidence from a prospective birth cohort. JAMA Psychiatry 72(5):466–474. https://doi.org/10.1001/jamapsychiatry.2014.3034
Lyall K, Van de Water J, Ashwood P, Hertz-Picciotto I (2015) Asthma and allergies in children with autism spectrum disorders: results from the CHARGE Study. Autism Res 8(5):567–574. https://doi.org/10.1002/aur.1471
Zerbo O, Leong A, Barcellos L, Bernal P, Fireman B, Croen LA (2015) Immune mediated conditions in autism spectrum disorders. Brain Behav Immun 46:232–236. https://doi.org/10.1016/j.bbi.2015.02.001
Tan Y, Thomas S, Lee BK (2019) Parent-reported prevalence of food allergies in children with autism spectrum disorder: National health interview survey, 2011–2015. Autism Res 12(5):802–805. https://doi.org/10.1002/aur.2106
Geng X, Wu L, Song L (2010) Study on food intolerance in children with autism and the curative effect of avoiding intolerance food. Chin J Appl Clin Pediatr 7:511–512
Li S, Wang X, Sun Z et al (2014) The food intolerance in patients with autism spectrum disorder. China J Health Psychol 22(2):181–182
Hu Q (2017) The study of food intolerlance specific IgG antibodiy in children with autism spectrum disoeder [Master]. Nanhua University
Lu M, Hu Y (2018) Review on the effects and mechanisms of food allergy on autism spectrum disorders. Chin J Child Health Care 26(04):389–91+95
Guo J, Li E (2016) Research progress on food intolerance in children with autism. Chin J Clin Rational Drug Use 9(11):176–177. https://doi.org/10.15887/j.cnki.13-1389/r.2016.11.122
Wu Y, Hou X, Feng Y (2016) Research progress on children with autism and food intolerance. Chin J Child Health Care 24(10):1052–54+58
Theoharides TC, Tsilioni I, Patel AB, Doyle R (2016) Atopic diseases and inflammation of the brain in the pathogenesis of autism spectrum disorders. Transl Psychiatry:6. https://doi.org/10.1038/tp.2016.77
Apicella F, Costanzo V, Purpura G (2020) Are early visual behavior impairments involved in the onset of autism spectrum disorders? Insights for early diagnosis and intervention. Eur J Pediatr 179(2):225–234. https://doi.org/10.1007/s00431-019-03562-x
Tsilioni I, Taliou A, Francis K, Theoharides T (2015) Children with autism spectrum disorders, who improved with a luteolin-containing dietary formulation, show reduced serum levels of TNF and IL-6. Transl Psychiatry 5:e647. https://doi.org/10.1038/tp.2015.142
Taliou A, Zintzaras E, Lykouras L, Francis K (2013) An open-label pilot study of a formulation containing the anti-inflammatory flavonoid luteolin and its effects on behavior in children with autism spectrum disorders. Clin Ther 35(5):592–602. https://doi.org/10.1016/j.clinthera.2013.04.006
Theoharides T, Tsilioni I (2018) Tetramethoxyluteolin for the treatment of neurodegenerative diseases. Curr Top Med Chem 18(21):1872–1882. https://doi.org/10.2174/1568026617666181119154247
Patel A, Theoharides T (2017) Methoxyluteolin inhibits neuropeptide-stimulated proinflammatory mediator release via mTOR activation from human mast cells. J Pharmacol Exp Ther 361(3):462–471. https://doi.org/10.1124/jpet.117.240564
Lange KW, Hauser J, Reissmann A (2015) Gluten-free and casein-free diets in the therapy of autism. Curr Opinion Clin Nutrit Metabol Care 18(6):572–575. https://doi.org/10.1097/mco.0000000000000228
Levine S, Kodesh A, Viktorin A et al (2018) Association of maternal use of folic acid and multivitamin supplements in the periods before and during pregnancy with the risk of autism spectrum disorder in offspring. JAMA Psychiatry 75(2):176–184. https://doi.org/10.1001/jamapsychiatry.2017.4050
Voskuhl R (2011) Sex differences in autoimmune diseases. Biol Sex Differ 2(1):1. https://doi.org/10.1186/2042-6410-2-1
Funding
This study was funded by National Natural Science Foundation of China (grant number: 81872704).
Author information
Authors and Affiliations
Contributions
Hong Li, Haixia Liu, and Yehuan Sun designed the research; Hong Li, Haixia Liu, and Xin Chen conducted the research; Hong Li, Haixia Liu, and Jian Zhang analyzed the data; Hong Li and Haixia Liu, and Xin Chen wrote the paper. Yehuan Sun mainly reviewed the paper and Guanglei Tong assisted. Hong Li and Haixia Liu had primary responsibility for the final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by Gregorio Paolo Milani
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Li, H., Liu, H., Chen, X. et al. Association of food hypersensitivity in children with the risk of autism spectrum disorder: a meta-analysis. Eur J Pediatr 180, 999–1008 (2021). https://doi.org/10.1007/s00431-020-03826-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-020-03826-x