Abstract
It is difficult to prevent hyperammonaemia in patients with urea cycle disorders that present in the newborn period. This is true, even if treatment is started prospectively because of an affected relative. We propose several additional measures that could be used in conjunction with conventional therapy to improve the metabolic control. Catabolism could be reduced by delivering the babies by elective caesarean section, by starting intravenous glucose immediately after delivery and, possibly, by using β-blockers or octreotide and insulin. The effectiveness of sodium benzoate and sodium phenylbutyrate might be increased by giving phenobarbital to the mother before delivery and subsequently to the baby to induce the enzymes for conjugation. We would expect the proposed measures to reduce the risk of hyperammonaemia and to improve the outcome for these patients. They have not, however, previously been used in this context, so families would need to be counselled carefully and controlled studies should be undertaken.

Similar content being viewed by others
Abbreviations
- ACTH:
-
Adrenocorticotrophic hormone
- CPS:
-
Carbamyl phosphate synthetase
- ECMO:
-
Extracorporeal membrane oxygenation
- NAG:
-
N-aceylglutamate
- OTC:
-
Ornithine transcarbamylase
References
Ali A, Qureshi IA (1992) Benzoyl-CoA ligase activity in the liver and kidney cortex of weanling guinea pigs treated with various inducers: relationship with hippurate synthesis and carnitine levels. Dev Pharmacol Ther 18:55–64
Arnold J, Campbell IT, Hipkin LJ et al (1995) Manipulation of substrate utilization with somatostatin in patients with secondary multiple organ dysfunction syndrome. Crit Care Med 23:71–77
Bachmann C (2003) Long-term outcome of patients with urea cycle disorders and the question of neonatal screening. Eur J Pediatr 162(Suppl 1):S29–S33
Falconer AD, Poyser LM (1986) Fetal sympatho-adrenal mediated metabolic responses to parturition. Br J Obstet Gynaecol 93:747–753
Gebhardt B, Dittrich S, Parbel S, Vlaho S, Matsika O, Bohles H (2005) N-carbamylglutamate protects patients with decompensated propionic aciduria from hyperammonaemia. J Inherit Metab Dis 28:241–244
Gropman AL, Batshaw ML (2004) Cognitive outcome in urea cycle disorders. Mol Genet Metab 81(Suppl 1):S58–S62
Haller M, Henzler-Le Boulanger A, Sass JO, Brandis M, Zimmerhackl LB (2005) Successful extracorporeal treatment of a male with hyperammonaemic coma. Nephrol Dial Transplant 20:453–455
Herndon DN, Hart DW, Wolf SE, Chinkes DL, Wolfe RR (2001) Reversal of catabolism by beta-blockade after severe burns. N Engl J Med 345:1223–1229
Hiroma T, Nakamura T, Tamura M, Kaneko T, Komiyama A (2002) Continuous venovenous hemodiafiltration in neonatal onset hyperammonemia. Am J Perinatol 19:221–224
Hussain K (2005) Congenital hyperinsulinism. Semin Fetal Neonatal Med 10:369–376
Kern RM, Yang Z, Kim PS, Grody WW, Iyer RK, Cederbaum SD (2007) Arginase induction by sodium phenylbutyrate in mouse tissues and human cell lines. Mol Genet Metab 90:37–41
Ktorza A, Bihoreau MT, Nurjhan N, Picon L, Girard J (1985) Insulin and glucagon during the perinatal period: secretion and metabolic effects on the liver. Biol Neonate 48:204–220
Kuchler G, Rabier D, Poggi-Travert F et al (1996) Therapeutic use of carbamylglutamate in the case of carbamoyl-phosphate synthetase deficiency. J Inherit Metab Dis 19:220–222
Maestri NE, Clissold D, Brusilow SW (1999) Neonatal onset ornithine transcarbamylase deficiency: a retrospective analysis. J Pediatr 134:268–272
Maestri NE, Hauser ER, Bartholomew D, Brusilow SW (1991) Prospective treatment of urea cycle disorders. J Pediatr 119:923–928
Msall M, Batshaw ML, Suss R, Brusilow SW, Mellits ED (1984) Neurologic outcome in children with inborn errors of urea synthesis. Outcome of urea-cycle enzymopathies. N Engl J Med 310:1500–1505
Nicolaides P, Liebsch D, Dale N, Leonard J, Surtees R (2002) Neurological outcome of patients with ornithine carbamoyltransferase deficiency. Arch Dis Child 86:54–56
Picca S, Dionisi-Vici C, Abeni D et al (2001) Extracorporeal dialysis in neonatal hyperammonemia: modalities and prognostic indicators. Pediatr Nephrol 16:862–867
Qureshi IA, Lebel S, Letarte J (1989) Development and inducibility of the hepatic and renal hippurate-synthesizing system in sparse-fur (spf) mutant mice with ornithine transcarbamylase deficiency. Biochem Int 19:657–666
Ramboer C, Thompson RP, Williams R (1969) Controlled trials of phenobarbitone therapy of neonatal jaundice. Lancet 1:966–968
Schubiger G, Bachmann C, Barben P, Colombo JP, Tonz O, Schupbach D (1991) N-acetylglutamate synthetase deficiency: diagnosis, management and follow-up of a rare disorder of ammonia detoxication. Eur J Pediatr 150:353–356
Sperling MA, DeLamater PV, Phelps D, Fiser RH, Oh W, Fisher DA (1974) Spontaneous and amino acid-stimulated glucagon secretion in the immediate postnatal period. Relation to glucose and insulin. J Clin Invest 53:1159–1166
Summar M (2001) Current strategies for the management of neonatal urea cycle disorders. J Pediatr 138:S30–S39
Uchino T, Endo F, Matsuda I (1998) Neurodevelopmental outcome of long-term therapy of urea cycle disorders in Japan. J Inherit Metab Dis 21(Suppl 1):151–159
Vogels BA, Maas MA, Daalhuisen J, Quack G, Chamuleau RA (1997) Memantine, a noncompetitive NMDA receptor antagonist improves hyperammonemia-induced encephalopathy and acute hepatic encephalopathy in rats. Hepatology 25:820–827
Whitelaw A, Bridges S, Leaf A, Evans D (2001) Emergency treatment of neonatal hyperammonaemic coma with mild systemic hypothermia. Lancet 358:36–38
Acknowledgements
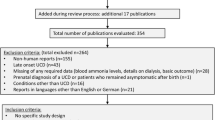
We would like to thank Dr Claude Bachmann for valuable discussion and particularly for permission to publish Fig. 1. We are also grateful to Dr Khalid Hussain for his help with this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leonard, J.V., Ward Platt, M.P. & Morris, A.A.M. Hypothesis: proposals for the management of a neonate at risk of hyperammonaemia due to a urea cycle disorder. Eur J Pediatr 167, 305–309 (2008). https://doi.org/10.1007/s00431-007-0486-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-007-0486-z