Abstract
Variability in severity among different respiratory syncytial virus (RSV) seasons may influence hospital admission rates for RSV-induced lower respiratory tract infection (LRTI) in young children. The aim of the present study was to identify through logistic regression analysis, risk factors associated with higher likelihood to acquire RSV-induced LRTI, in children with symptoms severe enough to lead to hospital admission. Over four consecutive RSV seasons (2000–2004), records from children <4 years of age admitted for RSV-induced LRTI (“cases”) were compared with those from children with LRTI not due to RSV and not requiring hospitalization (“controls”). 145 “case-patients” and 295 “control-patients” were evaluated. Independent from the severity of the four epidemic seasons, seven predictors for hospitalization for RSV infection were found in the bivariate analysis: number of children in the family, chronological age at the onset of RSV season, birth weight and gestational age, birth order, daycare attendance, previous RSV infections. In the logistic regression analysis, only three predictors were detected: chronological age at the beginning of RSV season [aOR = 8.46; 95% CI:3.09–23.18]; birth weight category [aOR = 7.70; 95% CI:1.29–45.91]; birth order (aOR = 1.92; 95% CI:1.21–3.06). Conclusions: Independent from the RSV seasonality, specific host/environmental factors can be used to identify children at greatest risk for hospitalization for RSV infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lower respiratory tract infection (LRTI) due to respiratory syncytial virus (RSV) is a major cause of morbidity in infants and young children [21]. Although certain risk factors have been traditionally associated with a higher likelihood to develop severe RSV-induced LRTI, the vast majority of children hospitalized for this condition are previously normal babies [3, 21]. Solid epidemiologic data indicate that prematurity is a consistently proven risk factor for severe LTRI induced by RSV [3, 21]. However, there are other independent risk factors, which show a significant variability among studies performed in different countries and even among different RSV seasons within the same country with alternation of minor and major epidemics [1, 3, 4, 21]. This was recently demonstrated in the “Osservatorio study”, which was designed to collect epidemiological data on RSV infection in two consecutive winter epidemics (2000–2002) in Italy [16]. This study showed that, because of differences in severity of the two RSV seasons, some of the risk factors were significant in one but not in the subsequent epidemics [15]. To further expand the RSV surveillance, the “Osservatorio study” was extended for two additional winter epidemics (2002–2004). The aim of the present study was to use the data collected to identify, by means of logistic regression analysis, risk factors associated with higher likelihood to acquire RSV-induced LRTI in children with symptoms severe enough to lead to hospital admission.
Materials and methods
Study design
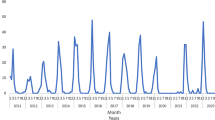
A case-control study was used to evaluate the risk factors associated with higher likelihood to acquire RSV-induced LRTI, severe enough to lead to hospital admission, over four consecutive winter epidemics in Italy (2000–2004). The pediatric centres involved (scattered over the Italian national territory), the study population, the surveillance, and the laboratory methods have been described elsewhere [13]. Briefly, all consecutive children, aged ≤4 years, referred to emergency departments for acute respiratory infection on one day of the week (Tuesday), between 8 a.m. and 2 p.m., during the “expected” epidemiological seasons (October – April) were enrolled and tested for RSV determination. Children who had received immunoprophylaxis with palivizumab (≤7, each year) were excluded. We expanded the age limit of the children to be enrolled over the “classic” 24 months, to also evaluate possible predictors of RSV-induced LRTI in an older age group. Each study site determined the date of onset and the end of the local RSV season according to a definition previously developed by the Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC) group [20]. The study protocol was approved by the local ethics board of each hospital and written informed consent was sought from parents or guardians of all children evaluated. Medical history and physical examination were recorded and evaluated and clinical assessment, including nasal secretion specimens for RSV detection, were obtained according to the usual protocol at each hospital. Nasal secretion samples were sent to the microbiology laboratory of each hospital to check for RSV by an immunoenzymatic test (TestPack RSV, Abbott, Italy) within 24 hours. Other respiratory viruses were not tested. All children were treated according to standardized protocols and the decision to admit a child to hospital for a respiratory illness was made by local non-study physicians responsible for each child’s care and was not influenced by the child’s participation in the study.
Case definition and control selection
During a given study year, children were considered eligible for the case-control study on the base of his/her first LRTI during that year. “Case of disease” was defined as LRTI due to RSV, occurring in a child ≤4 years of age and requiring hospital admission. From the cases we excluded patients with LRTI induced by agents other than RSV or RSV-positive but not severe enough to require hospitalization. “Controls” were selected from children who had LRTI which was with certainty not due to RSV (negativity on immunoenzymatic test performed on nasal secretions) and who did not require hospitalization. This control population was selected to determine both predictors of acquiring RSV infection and developing severe disease. All controls should have come from the same residence areas as case-patients. Since case patients ranged from 0 to 30 months of age, control patients aged ≥31 months were excluded from the total control population (N = 1064). Within the remaining group of controls (N = 729), a sample (N = 295) was randomly selected (simple random selection procedure via SPSS software) and included in the study to obtain a case-control ratio of 1:2.
For both case patients and controls evaluated in the four epidemic seasons, data related to the characteristics of the family (e.g. mother’s age, number of children in the family, father’s and mother’s educational level and social condition score) and of the children (e.g. chronological age of the child at the beginning of RSV season, birth weight, birth order, gestational age, length of breast feeding) were categorized according to cut-offs partially derived from literature [5, 10, 12] and partially imposed from the original categorization recorded in the “Osservatorio” database. In addition, children were considered to be small for gestational age (SGA) if their weight at birth fell below the 10th percentile based on gestational age and sex according to Oken’s method [15] and using the United States of America national reference.
Statistical analysis and data definitions
Descriptive statistics of the characteristics of the patients were performed and reported in terms of mean and standard deviation (SD) for the quantitative variables (chronological age, birth weight, gestational age, etc.) and in terms of absolute frequencies and percentages for the qualitative variables. Firstly, a bivariate analysis was performed and the comparison of quantitative variables between two groups of subjects (i.e. cases vs controls) was made calculating the likelihood ratio test (LR test), and reporting the bivariate odds ratio (OR) and 95% confidence interval (CI). Comparison of frequency data was performed by the chi-square test or by the Fisher’s exact test in case of expected frequencies less than five.
In order to evaluate the role of different predictors in the association with the outcome (hospitalization for RSV infection), multiple logistic regression analysis (step-down strategy) was performed. Variables that were statistically significant in the bivariate analysis or that were considered a priori important for the outcome were entered in the model. The following predictors were considered: epidemic season, father’s educational level, chronological age category at the beginning of RSV season, birth order, birth weight category, small for gestational age, daycare attendance, and previous RSV infections. The effect was expressed in terms of adjusted (a)OR and 95% CI and the LR test was performed. The models’ predictive ability has been investigated by calculating the area under the ROC curve of the model (AUC). All tests were two-sided and a P value less than 0.05 was considered statistically significant. The statistical packages used were the “Statistica release 6” (StatSoft Corp., Tulsa, OK, USA) for bivariate analyses and the “Stata release 7” (Stata Corporation, College Station, TX, USA) for multivariate analyses.
Results
Patient populations
There were 145 case-patients included in the study (plus three cases not evaluated because of missing values). There were 61 males (42.1%) and 84 females (57.9%), with a median age of 3.5 months and a median birth weight of 3,050 grams. Seventeen of the 145 (11.7%) were born preterm (at less than 36 weeks of gestational age), two had congenital heart conditions and five had a previous history of chronic lung disease.
There were 292 control-patients (plus three cases not evaluated because of missing values). There were 124 males (42.5%) and 168 females (57.5%), with a median age of 5 months. Eighteen were preterm infants (6.2%) and their birth weight was greater but not significantly different (mean = 2,310; median = 2,175 grams) from the preterm case-patients’ birth weight (mean = 1,993; median = 1,817.5) (P = 0.21).
Risk factors associated with a higher likelihood to acquire RSV-induced LRTI, severe enough to lead to hospital admission
In the bivariate analysis we considered several risk factors that could be associated with a higher likelihood to acquire RSV-induced LRTI, severe enough to lead to hospital admission.
In Table 1 only the statistically significant risk factors associated with a higher likelihood to acquire RSV-induced LRTI, severe enough to lead to hospital admission, are reported. The bivariate analysis showed that, although the severity of RSV-induced LRTI with hospital admission was different during the four epidemics, a variety of other risk factors could be detected. The only demographic-social characteristic associated with severe RSV-induced LRTI requiring hospitalization was the number of children in the family ≥2. Geographical area, social condition level and mother’s age category were not significant risk factors (not shown). The major predictors were the characteristics of the child itself as follows: low chronological age at the beginning of RSV season, being at least the second baby in the family, having a low birth weight (1,500–2,499 g), and a low gestational age (<33 weeks). In addition, the absence of daycare attendance was also a risk factor and higher risks could be seen in children without previous exposure to RSV infections. Having a birth weight small for the gestational age was also a risk factor but the role of the birth weight uncorrected for gestational age was a stronger predictor. Breast feeding had no significant role due to the small number of data available (n = 138). Mother’s educational level was available only in a very small subset of patients (n = 80) (not shown) and because of the strong association with father’s educational level (not shown) (P < 0.0001) only this latter variable was considered in subsequent analysis.
In the logistic regression analysis variables that were statistically significant in the bivariate analysis or that were considered a priori important for the outcome were entered in the model (see Table 1). As reported in Table 2 only three independent predictors were associated with severe RSV infection with hospitalization: a lower age category of the child, a lower birth weight category (<1500 grams), and birth order (being at least the second child in the family). The number of children in the family and gestational age were not entered in the logistic model because of the strong autocorrelation, respectively, with the variables birth order and birth weight. Indeed, the vast majority of children (84.6%) belonging to the lowest gestational age category (<33 weeks) and more than 60% of those belonging to the intermediate gestational age category (33–35 weeks) had a birth weight <2,500 grams.
Discussion
Evaluating data collected over four consecutive years in Italy, we found that, in addition to the severity of the RSV epidemics in a specific year, a variety of risk factors were associated with a higher likelihood to acquire RSV-induced LRTI, severe enough to lead to hospital admission. The only condition related to demographic and social characteristics of the family was the number of children in the family (being at least the second baby was a “risk-factor”). Among factors related to the characteristics of the children, major predictors were chronological age of the child at the onset of RSV season, birth weight and gestational age category, birth order, daycare attendance and previous episodes of RSV infections. However, in the logistic regression analysis, only three predictors turned out to be significant: chronological age at the beginning of RSV season, birth weight category, and birth order.
These results only partially confirm previous observations regarding risk factors for severe RSV infection [1, 2, 8, 11, 14, 17].
Chronological age of the child at the beginning of RSV season is a known factor for severe RSV-induced LRTI [1, 10, 17–19]. Indeed, in our study population only six children (4.1%) with a chronological age at the beginning of the season >12 months (and none between 2 to 4 years) had RSV-induced LRTI severe enough to lead to hospital admission. Aside from the incomplete development of the lung structure and the small size of the conducting airways related to the young age, data also suggest that such infants are less likely to have RSV-neutralizing maternal antibody as compared with infants born after the peak of the RSV season [6].
Birth weight was also an important risk factor in our study population. Low birth weight is often linked to low gestational age and there is no question that premature birth is, in general, associated with acute and chronic pulmonary morbidity [3, 5, 7–10, 14, 22]. Prematurity, in RSV-induced LRTI, can lead to increased need for and lengthened duration of hospital admission, intensive care, mechanical ventilation and supplemental oxygen, as well as increased mortality [1, 21]. Increased risk to develop severe RSV-induced LRTI may also be observed in the “less premature” infants, i.e. those with a gestational age of 32 weeks or greater, in the presence of other concomitant host/environmental unfavourable conditions, such as day-care attendance, low chronological age at the onset of RSV season, presence of preschool age sibling(s), and low birth weight [3, 5, 10, 21].
In the present study, gestational age, a strong risk factor in the bivariate analysis, was not included in the logistic model because of the strong autocorrelation with birth weight. Indeed, a great proportion of children belonging to two lower gestational age categories (<33 weeks and 33–35 weeks) had a birth weight <2,500 grams.
SGA has been only recently examined as an independent risk factor for hospitalization for RSV infection and, in agreement with the result of the present study, was found to be significant in a population of infants born at 33 through 35 weeks of gestation [10]. An interesting finding of the present report is that a low birth weight, corrected or uncorrected for gestational age, was a strong predictor for severe RSV-induced LRTI.
The third important predictor in our study population was birth order, i.e. being at least the second child in the family was found to be a risk factor for severe RSV-induced LRTI. A variety of studies demonstrated a trend toward higher numbers of RSV hospitalization rates in infants with any older siblings, including preschool age siblings (younger than 6 years old) who attend daycare and school age siblings (older than 3 years) [1, 3, 5–7, 10, 18, 19, 21].
In agreement with the majority of reports, other conditions related to demographic and social characteristics of the family (the number of children in the family) or of the environment (daycare attendance) were found in the bivariate analysis to be able to increase the likelihood to be hospitalized for RSV-induced LRTI [1, 3, 5–7, 10, 18, 19, 21]. While the number of children in the family was not entered in the logistic model because of the strong autocorrelation with the variable birth order, daycare attendance did not reach a significant value in the logistic regression analysis, probably because of the small number of children attending daycare in our study population [3 (2.1%) in the “case” group and 24 (22.0%) in the “control” group]. Despite other conditions, such as father’s and mother’s educational level, mother’s age category, social conditions, breast feeding, family history of allergy and gender and exposure to cigarette smoking, that were not statistically relevant in our study population, we cannot exclude that other socio-economical and environmental factors might be important [1, 3, 5–7, 10, 18, 19, 21]. As shown for other Mediterranean countries [5], exposure to tobacco smoke at home has decreased during recent years in Italy as a result of anti-smoking campaigns and better health education, and this may explain our surprising results.
Due to the low number of children with specific characteristics, other risk factors such as presence of chronic lung diseases or of congenital heart diseases, immunodeficiency, haematological malignancies, bone-marrow or organ transplants, and cystic fibrosis were not analysed. Moreover, since only in the second, third and fourth RSV season a limited number of children had received immunoprophylaxis with palivizumab, its protective effect could not be evaluated.
In summary, evaluating four RSV seasons, characterized by inter-annual alternation of minor and major epidemics, we found, in addition to prematurity, a limited number of other conditions which appear to influence the severity of RSV-induced LTRI in infants and young children. However, before translating to clinical practice these indications, other similar studies performed in different countries are required, including a broader number of children and covering other RSV epidemic seasons. This information should be valuable to better determine hospital resource management and individualize RSV prophylaxis programs in preterm and term infants.
Abbreviations
- LRTI:
-
lower respiratory tract infection
- RSV:
-
respiratory syncytial virus
- PICNIC:
-
Pediatric Investigators Collaborative Network on Infections in Canada
- SD:
-
standard deviation
- LR test:
-
likelihood ratio test
- OR:
-
odds ratio
- CI:
-
confidence interval
- SGA:
-
small for gestational age
- aOR:
-
adjusted OR
References
Boyce TG, Mellen BG, Mitchel EF, Wright PF, Griffin MR (2000) Rates of hospitalization for respiratory syncytial virus infection among children in Medicaid. J Pediatr 137:865–870
Bulkow LR, Singleton RJ, Karron RA, Harrison LH, Alaska RSV Study Group (2002) Risk factors for severe respiratory syncytial virus infection among Alaska native children. Pediatrics 109:210–212
Carbonell-Estrany X, Figueras-Aloy J, the Infeccio´n Respiratoria Infantil por Virus Respiratorio Sincitial Study Group, Law BJ, the Pediatric Investigators Collaborative Network on Infections in Canada Study Group (2004) Identifying risk factors for severe respiratory syncytial virus among infants born after 33 through 35 completed weeks of gestation: different methodologies yield consistent findings. Pediatr Infect Dis J 23(11 Suppl):S193–S201
Duppenthaler A, Gorgievski-Hrisoho M, Frey U, Aebi C (2003) Two-year periodicity of respiratory syncytial virus epidemics in Switzerland. Infection 31:75–80
Figueras-Aloy J, Carbonell-Estrany X, Quero J, Iris Study Group (2004) Case-control study of the risk factors linked to respiratory syncytial virus infection requiring hospitalization in premature infants born at a gestational age of 33–35 weeks in Spain. Pediatr Infect Dis J 23:815–820
Glezen WP, Paredes A, Allison JE, Taber LH, Frank AL (1981) Risk of respiratory syncytial virus infection for infants from low-income families in relationship to age, sex, ethnic group, and maternal antibody level. J Pediatr 98:708–715
Holman RC, Shay DK, Curns AT, Lingappa JR, Anderson LJ (2003) Risk factors for bronchiolitis associated deaths among infants in the United States. Pediatr Infect Dis J 22:483–489
Joffe S, Escobar GJ, Black SB, Armstrong MA, Lieu TA (1999) Rehospitalization for respiratory syncytial virus among premature infants. Pediatrics 104(4 Pt 1):894–899
Kramer MS, Demissie K, Yang H, Platt RW, Sauve R, Liston R (2000) The contribution of mild and moderate preterm birth to infant mortality: fetal and infant health study group of the Canadian perinatal surveillance system. JAMA 284:843–849
Law BJ, Langley JM, Allen U, Paes B, Lee DS, Mitchell I, Sampalis J, Walti H, Robinson J, O’Brien K, Majaesic C, Caouette G, Frenette L, Le Saux N, Simmons B, Moisiuk S, Sankaran K, Ojah C, Singh AJ, Lebel MH, Bacheyie GS, Onyett H, Michaliszyn A, Manzi P, Parison D (2004) The Pediatric Investigators Collaborative Network on Infections in Canada study of predictors of hospitalization for respiratory syncytial virus infection for infants born at 33 through 35 completed weeks of gestation. Pediatr Infect Dis J 23:806–814
Liese JG, Grill E, Fischer B, Roeckl-Wiedmann I, Carr D, Belohradsky BH, Munich RSV Study Group (2003) Incidence and risk factors of respiratory syncytial virus-related hospitalizations in premature infants in Germany. Eur J Pediatr 162:230–236
Medici MC, Arcangeletti MC, Merolla R, Chezzi C, Osservatorio VRS Study Group (2004) Incidence of respiratory syncytial virus infection in infants and young children referred to the emergency departments for lower respiratory tract diseases in Italy. Acta Biomed Ateneo Parmense 75:26–33
Medici MC, Arcangeletti MC, Rossi GA, Lanari M, Merolla R, Paparatti UD, Chezzi C, Osservatorio VRS Study Group (2006) Four year incidence of respiratory syncytial virus infection in infants and young children referred to the emergency departments for lower respiratory tract diseases in Italy: the “Osservatorio VRS” study (2000–2004). New Microbiol 29:35–43
Nielsen HE, Siersma V, Andersen S, Gahrn-Hansen B, Mordhorst CH, Norgaard-Pedersen B, Roder B, Sorensen TL, Temme R, Vestergaard BF (2003) Respiratory syncytial virus infection—risk factors for hospital admission: a case-control study. Acta Paediatr 92:1314–1321
Oken E, Kleinman KP, Rich-Edwards J, Gillman MW (2003) A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr 3:6–15
Rossi GA, Medici MC, Merolla R, Osservatorio VRS Study Group (2005) Incidence of respiratory syncytial virus positivity in young Italian children referred to the emergency departments for lower respiratory tract infection over two consecutive epidemic seasons. Infection 33:18–24
Simoes EAF (2003) Environmental and demographic risk factors for respiratory syncytial virus lower respiratory tract disease. J Pediatr 143(suppl):S118–S126
Stevens TP, Sinkin RA, Hall CB, Maniscalco WM, McConnochie KM (2000) Respiratory syncytial virus and premature infants born at 32 weeks’ gestation or earlier: hospitalization and economic implications of prophylaxis. Arch Pediatr Adolesc Med 154:55–61
Wang EE, Law BJ, Boucher FD, Stephens D, Robinson JL, Dobson S, Langley JM, McDonald J, MacDonald NE, Mitchell I (1996) Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC) study of admission and management variation in patients hospitalised with respiratory syncytial viral lower respiratory tract infection. J Pediatr 129:390–395
Wang EEL, Law BJ, Stephens D (1995) Pediatric Investigators Collaborative Network on Infections in Canada (PICNIC) prospective study of risk factors and outcomes in patients hospitalized with respiratory syncytial viral lower respiratory tract infection. J Pediatr 126:212–219
Weisman LE (2003) Populations at risk for developing respiratory syncytial virus and risk factors for respiratory syncytial virus severity: infants with predisposing conditions. Pediatr Infect Dis J 22:S33–S39
World Health Organization (1970) The prevention of perinatal mortality and morbidity. World Health Organization, Geneva
Acknowledgements
The study “Osservatorio VRS” was sponsored by Abbott S.p.A., Italy.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Rossi, G.A., Medici, M.C., Arcangeletti, M.C. et al. Risk factors for severe RSV-induced lower respiratory tract infection over four consecutive epidemics. Eur J Pediatr 166, 1267–1272 (2007). https://doi.org/10.1007/s00431-007-0418-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-007-0418-y