Abstract
In this double-blind randomised placebo-controlled trial it was investigated during a two-year follow-up whether oral bisphosphonates (Olpadronate 10 mg/m2/day) influence quality of life in children with osteogenesis imperfecta (OI). Thirty-four children with OI (classified according to Sillence criteria), aged 3 to 18 years of age, with a restricted level of ambulation were included. Randomisation was performed using a list of computer generated random numbers to allocate patients to receive Olpadronate or placebo. Quality of life was measured using self-perception profile for children (SPPC) and health-utility index (HUI). Differences between baseline measurements and measurements at two years follow-up were analysed within the Olpadronate and placebo group using a student’s t-test. Differences in HUI and SPPC regression coefficients were analysed by random-effects repeated measures analysis (SAS, Proc Mixed, version 8.2), adjusted for age, gender and type of OI. Within the Olpadronate group there was a significant decrease in pain utility; however, difference in six months’ regression coefficients between the placebo and Olpadronate group were not significant. Within the placebo group there was a significant increase in scholastic competence and behavioural conduct. The item behavioural conduct showed a steeper annual regression coefficient favourable for the placebo group. In the other SPPC items none of the annual regression coefficients showed a significant difference between the Olpadronate and the placebo group. Conclusion: We found only slight differences in quality of life in favour of the bisphosphonate group. A small but not significant decrease in pain was detected in the bisphosphonate group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Assessment of patient-focused health status and quality of life is recognized increasingly by clinicians, patients advocates and authorities as primary measures of need, effectiveness and efficiency in the evaluation of health care [16]. In orthopaedic surgery the effects of treatment are conventionally measured by physical function, (e.g. range of motion, walking distance) [28], whereas quality of life measures might be important to complement these conventional clinical methods [29]. Quality of life represents the functional effect of an illness and its consequent therapy upon a patient, as perceived by the patient [13]. Four components of the quality of life construct have been described: physical and occupational function, psychological state, social interactions and somatic sensation [34].
Assessment of burden of morbidity associated with orthopaedic diagnosis and the effectiveness of clinical interventions holds especially for chronic diseases. Due to substantial gains in survival rates in chronic diseases [3], the prevalence of children with a chronic disease increases, possibly influencing aspects of quality of life, like physical and occupational function, psychological state and social interactions.
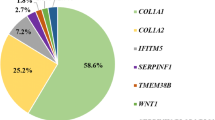
Osteogenesis imperfecta (OI) is a heritable disorder of connective tissue. Most OI types are caused by a defect in collagen type I synthesis and shows highly variable clinical expression [6]. OI is subdivided into four types, I, II, III and IV, based on clinical, radiographic and genetic characteristics [36]. In OI type I, collagen type I synthesis is reduced, in OI types II, III and IV, collagen type I synthesis is reduced and abnormal [40]. Recently, Glorieux et al. reported that in OI types V, VI and VII there is no evident mutation in type 1 collagen [21, 22, 39]. Major clinical characteristics in OI include fragility of bone, osteopenia, variable degrees of short stature, and progressive skeletal deformities. Other clinical manifestations include blue sclerae, dentinogenesis imperfecta, joint laxity and maturity-onset deafness [32]. In children with OI, consequences of the disease regarding body function and structure, activities, participation, as well as internal and external contextual factors have been described in detail but aspects of quality of life have been described sparingly [10–12].
Aspects of quality of life (perceived competence) have been described in children with OI, not treated by medication, using the self-perception profile for children (SPPC) [9, 24]. In these children, fair to strong positive perceived competence was measured. Suskauer et al. recently described the temperament in children with OI and concluded that it did not differ from non-disabled peers [37].
In the past decade, treatment by medication (bisphosphonates) in children with OI was initiated. Bisphosphonates suppress osteoclast-mediated bone resorption [7]. Many uncontrolled trials have been performed regarding the influence of bisphosphonates on OI [1, 20, 23]. Recently, two double blind randomised placebo controlled trials were performed investigating the influence of bisphosphonates on fracture incidence, functional ability and bone mineral density. Letchocha et al. found a decrease in upper extremity fractures without a significant improvement in ambulation and muscle strength [30]. Fracture incidence in the lower extremity did not change. In our study group we showed a reduced fracture risk of 30% and increased lumbar bone mineral density in the bisphosphonate group without significant increase in functional ability level during the follow-up (2 years) as compared to the placebo group [33]. In this paper the main issue is quality of life; analyses are focused on unpublished data concerning quality of life. The severity of osteogenesis imperfecta was not similar in the two groups which were randomised prospectively (oral bisphosphonate or placebo). This might skew the outcome of this study.
The purpose of this study was to investigate whether oral bisphosphonate therapy might influence aspects of quality of life in OI children. Our hypothesis was that fewer fractures in children with OI during bisphosphonate treatment may result in less pain, and thereby improving quality of life.
Patients and methods
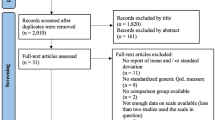
Medical histories of children with skeletal dysplasias were extracted from a database kept by the Department of Paediatric Orthopaedic Surgery, Wilhelmina Children’s Hospital of the University Medical Centre Utrecht, The Netherlands. Children were eligible for participation in the study if they had documented OI. To be able to measure a difference in functional outcome, only children with a restricted level of ambulation were included. The maximum level of ambulation, measured according to the modified Bleck scale [2, 11], was “neighbourhood walker without crutches” (maximum walking distance 250 m). Thirty-seven patients were approached to participate in the present prospective placebo-controlled randomised study with Olpadronate (3-dimethylamino-1-hydroxypropylidene-1,1-biphosphonate). One child was not able to take part in the study for religious reasons and the parents of two children refused for logistical reasons. Eventually, 16 boys and 18 girls from 3 to 18 years old were included (13 children with OI type I, 9 with OI type III, and 12 with OI type IV according to the classification proposed by Sillence) [36]. Informed consent to participate was obtained from the parents.
All patients included in this study were seen on a regular basis in a single-centre, nationwide outpatient multidisciplinary unit for children with OI. Children were consecutively randomised independently of their OI type. Randomisation was performed using a list of computer generated random numbers to allocate patients to receive oral Olpadronate in a dose of 10 mg/m2/day or placebo for a total period of 2 years. Administration of the drugs was around 7:00 a.m., fasting, half an hour before breakfast, and in upright position. With regard to possible group incomparabilities, we decided not to stratify the randomisation process but to adjust in the analysis for any baseline incomparabilities that might occur after randomisation.
Both Olpadronate and placebo were prepared as enteric-coated tablets by Tiopharma BV, Oud Beyerland, the Netherlands. To circumvent any nutritional insufficiencies, all children received a supplement of 500 mg/m2/day elementary calcium and 400 IU/day cholecalciferol. Routine care of the children was continued throughout the study (fracture treatment, intra-medullary rodding, corrective osteotomies scoliosis surgery and rehabilitation when indicated).
The study was approved by the Medical Ethical Committee of the University Medical Centre Utrecht, the Netherlands, for a maximum follow-up of 2 years, under the condition that no children below the age of 3 years were recruited. Quality of life was measured using the health utility index-mark III (HUI) [17] and self-perception profile for children (SPPC) [24, 38]. The HUI questionnaire is a non-disease specific, generic instrument and applicable in a wide range of populations and has been extensively used in Canadian children [4]. Reliability and validity of HUI has been investigated and validated in Dutch children [19]. The HUI classification system consists of eight attributes. Each attribute consists of five to six levels representing the range of functioning from normal (1) to severely impaired (5 or 6). The attributes forming the HUI system are vision (1–6), hearing (1–6), speech (1–5), ambulation (1–6), dexterity (1–6), emotion (1–5), cognition (1–6), and pain (1–5). Information from the questionnaires was converted to health state vectors in the HUI formats by an established algorithm [14]. Single attribute scores of morbidity are defined on a scale where the worst level has a score of 0 and the best level has a score of 1 [25]. Normative values are provided by Furlong et al. [15]. In this study, the attributes pain and ambulation were analyzed. The other attributes, hearing, speech, dexterity, emotion and cognition were not analyzed, because they were at maximum level during inclusion. In this study the parental (proxy) questionnaire version of the HUI was used. All parents were instructed by the investigator. This questionnaire was measured at baseline, and repeated at a six months interval.
Perceived competence was measured using the Harter self-perception profile for children (SPPC) [24]. The perceived competence scale has been cross-culturally validated for Dutch children and normative scores are available for healthy Dutch children [38]. The SPPC contains six subscales, taping five specific domains, scholastic competence, social acceptance, athletic performance, physical appearance, behavioural conduct and global self-worth. The questionnaire consists of 36 items, 6 items for each subscale. Domain scores of perceived competence are defined on a scale where the worst level is scored 1 (strongly negative) and the best level is scored 4 (strongly positive). Perceived competence questionnaires were obtained from the children without parental assistance, to avoid parental influence concerning the child’s perceived competence. In children younger than 6 years of age, Harter pictorial scales of perceived competence were used. Subscales, domains and normal values in the pictorial scale are different from the questionnaire used in children from 6–12 or 12–18 years of age. Therefore, the SPPC analysis in children younger than 6 years of age (n = 6) was not involved in analysis. This notwithstanding, these children were included in this trial because HUI analysis was applicable for this age. Other parameters measured in these young children were suitable for analysis and have already been published [33].
The fracture incidence was scored using new radiologically confirmed non-vertebral fractures.
All data were gathered by the first author (HJK).
Drug tolerability and compliance
Prior to the study, children and parents were informed about the occasional occurrence of gastrointestinal side effects reported with the use of any bisphosphonate (regurgitation, heartburn, and upper abdominal discomfort). In the Olpadronate group no side effects like esophagitis were reported. In the placebo-group one child suffered upper abdominal discomfort of unknown origin, which disappeared spontaneously within one week. Parents returned empty boxes to the investigator during outpatient clinic visit. In the Olpadronate group bone mineral density significantly increased compared to the controls [33]. This bisphosphonates effect has been reported extensively [1, 20, 23] and confirms compliance in the Olpadronate group.
Statistical analysis
Differences between baseline measurements and two-year follow-up regarding HUI and SPPC were analyzed within the Olpadronate and placebo groups using a student’s t-test. Differences in six months’ interval (repeated every 6 months) of HUI scores between the Olpadronate and placebo groups were analyzed by random-effects repeated-measures analysis (SAS, Proc Mixed, version 8.2). Differences in one year’s interval (repeated every year) of SPCC scores between the Olpadronate and placebo groups were analyzed by random-effects repeated-measures analysis (SAS, Proc Mixed, version 8.2). The correlation between the total number of fractures during the trial, mean pain score (HUI) and mean ambulation level (HUI) in treatment and placebo group, was analysed by Spearman’s correlation coefficient.
Differences are expressed as regression coefficient and 95% confidence interval (95% CI), and adjustment for age, OI type and gender was performed.
Results
Group differences in age, OI type and gender are presented in Table 1. One patient in the placebo group withdrew 3 months after randomisation for reasons of motivation and logistics. Another patient who had been assigned to the Olpadronate group encountered a clinical discussion during follow-up about specific features of his bone disorder, and his parents stopped medication at 18 months’ follow-up. Two children, one in each group, showed suboptimum adherence since they forgot to take medication once a week on average. No child reported signs or symptoms of an acute-phase reaction.
Mean values of SPPC at start and follow-up were equal or above the mean level for Dutch healthy children [38] in both the placebo and Olpadronate groups (Table 2), with the exception of athletic performance. Differences in annual regression coefficients between the Olpadronate and placebo groups are described in Table 3. In the placebo group a significant increase in scholastic competence and behavioural conduct was found. The item behavioural conduct showed a steeper annual regression coefficient (0.23) favourable for the placebo group, after adjustment for age, sex and type of OI. In the other items no annual regression coefficients showed a significant difference between the Olpadronate and placebo groups, either unadjusted or adjusted for age, sex and type of OI.
Mean values of HUI pain utility and ambulation were around level 2 (0.92), indicating mild to moderate pain that prevents no activities, and just above level 3 (0.63), respectively, which means able to walk around the neighbourhood with walking equipment, but without the help of another person.
Differences between the first and last measurements in HUI were calculated within the Olpadronate and placebo group (Table 4). Within the Olpadronate group there was a significant decrease in pain utility. Differences in six months’ regression coefficient regarding the utilities ambulation and pain are given in Table 5. None of these six months’ regression coefficients showed a significant difference, either unadjusted or adjusted for age, sex and type of OI. In the remaining items of HUI it was not possible to calculate six months’ regression coefficients because the items did not change during follow-up. Six children on Olpadronate (40%) and 5 children on placebo (29%) had no fractures throughout the study. In the Olpadronate group, four children had 1 fracture, one had 2, one had 3, two had 4 and one child had 5 fractures. Fifteen fractures had occurred during the first year and 7 during the second year of the study. In the placebo group, two children had 1 fracture, one had 2, three had 3, one had 4, two had 5, one had 7, one had 8, and one child had 10 fractures. Twenty-four had occurred during the first year and 28 during the second year of the study. Olpadronate therapy resulted in 25 percent relative fracture risk reduction.
In the Olpadronate group no significant correlations were found between pain (HUI) and number of fractures in 2 years, whereas in the placebo group a moderate significant correlation was found (−0.48, p = 0.046) (Table 6).
Discussion
We found little difference in quality of life between the bisphosphonate and placebo groups however in favour of the bisphosphonate group during the two-year follow-up. The small number of children included might be a limiting factor in this study. It was not possible to include more children with OI in the Netherlands who met our inclusion criteria. SPPC levels at start and follow-up were equal or above the mean level for Dutch healthy children [38] in both the placebo and Olpadronate group (Table 2). This high level of SPPC baseline measurement makes it difficult to measure a statistical significant improvement. Within the Olpadronate group there was a very small, significant decrease in pain. Within the placebo group scholastic competence and behavioural conduct increased during follow-up, this might be due to maturation [35]. Remarkably, a significant difference was found in annual change concerning behavioural conduct, favourable for the placebo group. We cannot explain the different development between the two groups in behavioural conduct, in this small study it might be an artifact. Olpadronate was chosen because it is one of the more potent nitrogen-containing bisphosphonates, and the efficacy and safety of the drug was investigated in growing children [5, 27]. Furthermore, oral medication is preferred in placebo-controlled studies and oral bisphosphonates have shown to be equally effective as intravenous bisphosphonates [8]. Its potency in terms of antiresorptive efficacy is comparable to that of Alendronate and Residronate [7].
Part of the results of this study, concerning bone mineral density, functional ability and fracture incidence during the trial, were reported earlier [33]. We may conclude that Olpadronate in a daily dosage of 10 mg/m2 has a measurable clinical effect since an increased bone mineral density and lower fracture incidence favourable in the Olpadronate group were found [33]. If Olpadronate had clearly influenced quality of life, we probably would have measured this.
There is a discrepancy in outcomes on quality of life between the reports of uncontrolled studies and controlled studies with bisphosphonates. In other randomised controlled trials with bisphosphonate therapy, an increased BMD and decreased fracture incidence did not clearly influence pain level as well [18, 30]. On the other hand, in several uncontrolled studies in children with OI treated with bisphosphonates, beneficial effects in terms of pain level as measured by a VAS score were reported [20, 23, 31, 41]. In these non-controlled trials the beneficial effect of bisphosphonate on pain level was explained by a decreased fracture incidence [20, 23, 31, 41]. Within our treatment group a very slight significant decrease in pain level was measured at the end of the study; however, at six months’ interval regression coefficients did not differ between the two groups. In this study pain level was measured by HUI parental (proxy) questionnaire. It might be possible that a discrepancy between observed pain by the parents and pain level in the child’s opinion existed. Perception of quality of life from the perspectives of patients, parents and paediatricians as measured by HUI has been investigated by Janse et al. [26]. They mentioned that children perceived more pain than parents observed [26]. When using the HUI in our study, it might therefore have been possible that a discrepancy between the observed pain by the parents and the pain level in the child’s opinion existed. Another intrinsic limitation of the study was that it was not possible to analyse the complete follow-up of SPPC assessment by the child itself, because some children were too young to fill in the form or were not able to read Dutch comprehensively.
One item of the SPPC behaviour showed a different annual coefficient favourable for the Olpadronate group. We cannot explain by which mechanism bisphosphonates might influence behaviour.
In another aspect of quality of life, athletic performance (SPCC) and ambulation level (HUI), no difference was found during two years of follow-up. This is in concordance with our previous reported results on functional ability [33].
Bisphosphonate therapy results in a decreased fracture incidence, which results in decreased surgical interventions and consecutive hospitalisation and immobilisation. It is possible that quality of life ameliorates after a follow-up period longer than 2 years; a longer interval without fractures and immobilisation might be necessary to improve quality of life. If our study group would have been larger, results concerning quality of life might have been more pronounced. In our study it was not possible to recruit more children with OI who were registered in the Netherlands. In the placebo group, Spearman’s correlation coefficient between number of fractures and pain was significant, children who suffered more fractures during two years of follow-up, suffered more pain as well. No correlation was found in the Olpadronate group, possibly the lower number of fractures made correlations less clear. Another explanation is that a low pain level, especially in the bisphosphonates group, made the correlation between the number of fractures and pain level less clear. Following randomisation, there was a relatively greater amount of children with a more severe form of OI in the Olpadronate group (12 of 16 children with types III and IV OI, 75%), as compared to the placebo group (9 of 18 children with types III and IV OI, 50%). Although we adjusted for OI type, this might have influenced results concerning quality of life, ambulation level and athletic performance. In types III and IV OI, a plateau phase in functional ability has been described [10]. Therefore it might be difficult to find a possible improvement in athletic performance and ambulation level in the Olpadronate group, since 75% of the children in this group have OI type III or IV.
Role of the funding source
Financial support was granted by the University Medical Centre Utrecht, the Netherlands. The funding source was not involved in design, conduct, analysis, interpretation, writing and submission of this study.
References
Astrom E, Soderhall S (1998) Beneficial effect of bisphosphonate during five years of treatment of severe osteogenesis imperfecta. Acta Paediatr 87:64–68
Bleck EE (1981) Nonoperative treatment of osteogenesis imperfecta: orthotic and mobility management. Clin Orthop 111–122
Bleyer WA (2002) Cancer in older adolescents and young adults: epidemiology, diagnosis, treatment, survival, and importance of clinical trials. Med Pediatr Oncol 38:1–10
Boyle MH, Furlong W, Feeny D, Torrance GW, Hatcher J (1995) Reliability of the Health Utilities Index-Mark III used in the 1991 cycle 6 Canadian General Social Survey Health Questionnaire. Qual Life Res 4:249–257
Brumsen C, Hamdy NA, Papapoulos SE (1997) Long-term effects of bisphosphonates on the growing skeleton. Studies of young patients with severe osteoporosis. Medicine (Baltimore) 76:266–283
Byers PH (1989) Inherited disorders of collagen gene structure and expression. Am J Med Genet 34:72–80
Cremers SC, Pillai G, Papapoulos SE (2005) Pharmacokinetics/pharmacodynamics of bisphosphonates: use for optimisation of intermittent therapy for osteoporosis. Clin Pharmacokinet 44:551–570
Dimeglio LA, Ford L, McClintock C, Peacock M (2005) A comparison of oral and intravenous bisphosphonate therapy for children with osteogenesis imperfecta. J Pediatr Endocrinol Metab 18:43–53
Engelbert RH, Gulmans VA, Uiterwaal CS, Helders PJ (2001) Osteogenesis imperfecta in childhood: perceived competence in relation to impairment and disability. Arch Phys Med Rehabil 82:943–948
Engelbert RH, Uiterwaal CS, Gerver WJ, van der Net JJ, Pruijs HE, Helders PJ (2004) Osteogenesis imperfecta in childhood: impairment and disability. A prospective study with 4-year follow-up. Arch Phys Med Rehabil 85:772–778
Engelbert RH, Uiterwaal CS, Gulmans VA, Pruijs H, Helders PJ (2000) Osteogenesis imperfecta in childhood: prognosis for walking. J Pediatr 137:397–402
Engelbert RH, Uiterwaal CS, Gulmans VA, Pruijs HE, Helders PJ (2000) Osteogenesis imperfecta: profiles of motor development as assessed by a postal questionnaire. Eur J Pediatr 159:615–620
Erling A (1999) Methodological considerations in the assessment of health-related quality of life in children. Acta Paediatr Suppl 88:106–107
Feeny D, Furlong W, Torrance GW, Goldsmith CH, Zhu Z, DePauw S, Denton M, Boyle M (2002) Multiattribute and single-attribute utility functions for the health utilities index mark 3 system. Med Care 40:113–128
Furlong W et al (2005) Multiplicative multi-attribute utility function for the health utilities index mark 3 (HUI3) system: a technical report. CEHPA WP#98–11. Centre for Health Economics and Policy Analysis, McMaster University, Hamilton, Canada, pp 76, 96
Furlong W, Barr RD, Feeny D, Yandow S (2005) Patient-focused measures of functional health status and health-related quality of life in pediatric orthopedics: a case study in measurement selection. Health Qual Life Outcomes 3:3
Furlong WJ, Feeny DH, Torrance GW, Barr RD (2001) The Health Utilities Index (HUI) system for assessing health-related quality of life in clinical studies. Ann Med 33:375–384
Gatti D, Antoniazzi F, Prizzi R, Braga V, Rossini M, Tato L, Viapiana O, Adami S (2005) Intravenous neridronate in children with osteogenesis imperfecta: a randomized controlled study. J Bone Miner Res 20:758–763
Gemke RJ, Bonsel GJ (1996) Reliability and validity of a comprehensive health status measure in a heterogeneous population of children admitted to intensive care. J Clin Epidemiol 49:327–333
Glorieux FH, Bishop NJ, Plotkin H, Chabot G, Lanoue G, Travers R (1998) Cyclic administration of pamidronate in children with severe osteogenesis imperfecta. N Engl J Med 339:947–952
Glorieux FH, Rauch F, Plotkin H, Ward L, Travers R, Roughley P, Lalic L, Glorieux DF, Fassier F, Bishop NJ (2000) Type V osteogenesis imperfecta: a new form of brittle bone disease. J Bone Miner Res 15:1650–1658
Glorieux FH, Ward LM, Rauch F, Lalic L, Roughley PJ, Travers R (2002) Osteogenesis imperfecta type VI: a form of brittle bone disease with a mineralization defect. J Bone Miner Res 17:30–38
Gonzalez E, Pavia C, Ros J, Villaronga M, Valls C, Escola J (2001) Efficacy of low dose schedule pamidronate infusion in children with osteogenesis imperfecta. J Pediatr Endocrinol Metab 14:529–533
Harter S (1982) The perceived competence scale for children. Child Develop 53:87–97
Horsman J, Furlong W, Feeny D, Torrance G (2003) The Health Utilities Index (HUI(R)): concepts, measurement properties and applications. Health Qual Life Outcomes 1:54
Janse AJ, Uiterwaal CS, Gemke RJ, Kimpen JL, Sinnema G (2005) A difference in perception of quality of life in chronically ill children was found between parents and pediatricians. J Clin Epidemiol 58:495–502
Landsmeer-Beker EA, Massa GG, Maaswinkel-Mooy PD, van de Kamp JJ, Papapoulos SE (1997) Treatment of osteogenesis imperfecta with the bisphosphonate Olpadronate (dimethylaminohydroxypropylidene bisphosphonate). Eur J Pediatr 156:792–794
Laupacis A, Bourne R, Rorabeck C, Feeny D, Wong C, Tugwell P, Leslie K, Bullas R (1993) The effect of elective total hip replacement on health-related quality of life. J Bone Joint Surg Am 75:1619–1626
Laupacis A, Rorabeck CH, Bourne RB, Feeny D, Tugwell P, Sim DA (1989) Randomized trials in orthopaedics: why, how, and when? J Bone Joint Surg Am 71:535–543
Letocha AD, Cintas HL, Troendle JF, Reynolds JC, Cann CE, Chernoff EJ, Hill SC, Gerber LH, Marini JC (2005) Controlled trial of pamidronate in children with types III and IV osteogenesis imperfecta confirms vertebral gains but not short-term functional improvement. J Bone Miner Res 20:977–986
Plotkin H, Rauch F, Bishop NJ, Montpetit K, Ruck-Gibis J, Travers R, Glorieux FH (2000) Pamidronate treatment of severe osteogenesis imperfecta in children under 3 years of age. J Clin Endocrinol Metab 85:1846–1850
Roughley PJ, Rauch F, Glorieux FH (2003) Osteogenesis imperfecta-clinical and molecular diversity. Eur Cell Mater 5:41–47
Sakkers R, Kok D, Engelbert R, van Dongen A, Jansen M, Pruijs H, Verbout A, Schweitzer D, Uiterwaal C (2004) Skeletal effects and functional outcome with Olpadronate in children with osteogenesis imperfecta: a 2-year randomised placebo-controlled study. Lancet 363:1427–1431
Schipper HS, Clinch JJ, Olwenly CLM (1996) Quality of life studies: definitions and conceptual issues. In: Spilker B (ed) Quality of life and pharmacoeconomics in clinical trials. Lippincott-Raven, Philadelphia, pp 11–23
Shevlin M, Adamson G, Collins K (2003) The self-perception profile for children (SPPC): a multiple-indicator multiple-wave analysis using LISREL. Pers Indiv Differ 35:1993–2005
Sillence DO, Senn A, Danks DM (1979) Genetic heterogeneity in osteogenesis imperfecta. J Med Genet 16:101–116
Suskauer SJ, Cintas HL, Marini JC, Gerber LH (2003) Temperament and physical performance in children with osteogenesis imperfecta. Pediatrics 111:E153–E161
van Dongen-Melman JEWM, Koot HM, Verhulst FC (2001) Cross-cultural validation of Harter’s self-perception profile for children in a Dutch sample. Educ Psychol Meas 739–753
Ward LM, Rauch F, Travers R, Chabot G, Azouz EM, Lalic L, Roughley PJ, Glorieux FH (2002) Osteogenesis imperfecta type VII: an autosomal recessive form of brittle bone disease. Bone 31:12–18
Willing MC, Pruchno CJ, Atkinson M, Byers PH (1992) Osteogenesis imperfecta type I is commonly due to a COL1A1 null allele of type I collagen. Am J Hum Genet 51:508–515
Zacharin M, Kanumakala S (2004) Pamidronate treatment of less severe forms of osteogenesis imperfecta in children. J Pediatr Endocrinol Metab 17:1511–1517
Acknowledgement
We thank all children and parents who participated in the study. We gratefully acknowledge the Wilhelmina Children’s Hospital of the University Medical Centre Utrecht for funding the study.
Conflict of interest statement
None of the authors had any financial or personal relationship with other persons or organisations that could inappropriately influence this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Kok, D.H.J., Sakkers, R.J.B., Janse, A.J. et al. Quality of life in children with osteogenesis imperfecta treated with oral bisphosphonates (Olpadronate): a 2-year randomized placebo-controlled trial. Eur J Pediatr 166, 1155–1161 (2007). https://doi.org/10.1007/s00431-006-0399-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-006-0399-2