Abstract
Tumor budding grade is a very useful histological prognostic indicator for colorectal cancer patients. Recently, it has been also reported as a significant prognostic indicator in invasive breast carcinoma patients. Our group and others have previously reported that the presence of a fibrotic focus in the tumor is a very useful histological finding for accurately predicting the prognosis in patients with invasive carcinoma of no special type (ICNST) of the breast. The purpose of the present study was to investigate whether a grading system incorporating tumor budding in a fibrotic focus is superior to the conventional grading system for tumor budding to accurately predict outcomes in patients with ICNST. According to our new grading system, we classified the tumors into grade I (164 cases), grade II (581 cases), and grade III (110 cases), and the results clearly demonstrated the significant superiority of the new grading system over that of conventional tumor budding alone for accurately predicting outcomes in patients with ICNST. Our findings strongly suggest that tumor cells and tumor-stromal cells interaction play very important roles in tumor progression rather than tumor cells alone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tumor budding (TB) refers to the small clusters of dedifferentiated tumor cells at the invasive margin of a tumor, and tumor budding grade (TBG) is very useful histological prognostic indicator in patients with colorectal cancer [1,2,3,4], and recently, TBG has also been reported as a significant prognostic indicator in patients with invasive breast carcinoma [5,6,7].
Our group and others have previously reported that the presence of a fibrotic focus (FF) is a very useful histological finding for accurately predicting the outcome in patients with invasive carcinoma of no special type (ICNST) of the breast [8,9,10,11,12,13,14,15,16,17,18]. The characteristics of tumor-stromal fibroblasts forming an FF and a high tumor angiogenesis ratio have been suggested to heighten the malignant potential of ICNSTs with an FF [19, 20]; other reports have indicated that the presence of FF is clearly associated with an intratumoral hypoxic condition of ICNSTs of the breast [10, 14, 21]. Furthermore, a cDNA microarray analysis reported previously clearly demonstrated specific biological characteristics of ICNSTs with an FF [12].
The purpose of the present study was to investigate whether a grading system for tumor budding incorporating both the conventional TBG and TBG in an FF proposed by us might be superior to the conventional TBG for accurately predicting the outcomes in patients with ICNSTs of the breast.
Materials and methods
Patients and histological examinations
The subjects of this study were 855 consecutive patients with ICNST of the breast who had undergone surgical treatment without prior neoadjuvant therapy at the Saitama Medical University International Medical Center between April 2007 and December 2015. All the patients were Japanese women, ranging in age from 29 to 92 years (median, 56 years). Of the 855 patients, 588 had undergone partial mastectomy, 261 had undergone modified radical mastectomy, and the remaining 6 had undergone standard radical mastectomy. Sentinel node dissection alone had been performed in 579 patients, and both sentinel node plus non-sentinel node dissection had been performed in 276 patients. None of the patients had received radiotherapy or chemotherapy before surgery, but 833 patients had received postoperative adjuvant therapy. The adjuvant therapy in these patients consisted of endocrine therapy in 413 patients, chemotherapy in 131 patients, chemoendocrine therapy in 211 patients, and trastuzumab with an endocrine therapy regimen and a chemotherapy regimen in 78 patients. All the tumors were classified according to the pathological UICC-TNM (pTNM) classification [22]. The protocol for this study was reviewed by the institutional review board of the Saitama Medical University International Medical Center.
For the pathological examination of the tumors, the surgically resected specimens were fixed in 10% formalin. Well-known clinicopathological factors and the degree of infiltration by tumor-infiltrating lymphocytes (TILs; %) (Supplementary Table 1), conventional TBG, and presence/absence of an FF were evaluated (Supplementary Table 1). The percentage of TILs was counted in the stromal compartment (stromal TILs; magnification × 200–400), excluding the TILs outside the tumor border and around ductal carcinoma in situ and/or normal lobules [23,24,25]. All mononuclear cells (including lymphocytes and plasma cells) were counted, while polymorphonuclear leukocytes were excluded. The denominator used to determine the % stromal TILs is the area of stromal tissue, and a full assessment of the average number of TILs in the tumor area was used, without focusing only on hotspots. In the present study, the optimal cut-off value of the TIL (%) for accurately predicting the patient outcome was examined by univariate analysis using the Cox proportional hazards regression model, and the following were determined as potential cut-off values: 0%, 0–19%, and > 19% (Supplementary Table 1). Conventional TBG (CTBG) was determined by examination of peripheral area of the tumor grade (Fig. 1) [5,6,7]. CTBG was scored based on examination of the tumor buds at the invasive front of the tumor within 1.1 mm (2 × 1 high-power field) on either side of the tumor interface with normal tissue. TB was defined as an isolated single tumor cell or a cluster composed of fewer than five tumor cells at invasive front area, and was graded according to the three categories [1,2,3,4,5,6,7]. At first, two breast pathologists (MH and TH) examined H&E-stained sections at low-power magnification (× 4 or × 10) to identify five areas each of the tumor showing the highest density of TB (hot-spot) that were suitable for examining CTBG; then, the tumor buds were counted in these five spots at × 200 magnification (Zeiss Axioskop 40, field size 0.98 mm2) (Fig. 2A–C). The maximum tumor bud count in the five hot-spots for CTB was evaluated for each case [26]. In addition, the tumor buds in the FF were also examined in cases with an FF. Briefly, an FF is surrounded by a highly cellular zone of infiltrating carcinoma cells and occupies a variable percentages of the tumor area (Fig. 2D, F) [8, 9]. The maximum tumor bud count in five areas within an FF showing the highest density of tumor bud (hot-spots) were evaluated in cases with an FF (Fig. 2D–G). Fundamentally, TB was evaluated in H&E staining [26], but immunohistochemistry for E-cadherin (Flex monoclonal mouse anti-human E-cadherin, clone NCH38, ready-to-use; DAKO, CA, USA) was performed in all cases for confirming TB cells in each case and differentiating INST from lobular carcinoma. We defined the estrogen receptor status and progesterone receptor status of the tumor cells according to the ASCO/CAP guideline [27]. Cases positive immunostaining 1 to 100% of the tumor cell nuclei for ER or PgR were interpreted as showing a positive receptor (ER- and PgR-positive, respectively) status, while cases with positive staining of < 1% or 0% of the cell nuclei were considered as being negative for ER/ PgR expression. HER2 expression in the tumor cells was also categorized according to the ASCO/CAP guideline [28,29,30] (Supplementary Table 2). The Ki-67 (MIB-1, mouse monoclonal, ready-to-use; DAKO, Glostrup, Denmark) labeling index of stroma-invasive tumor cells was calculated as the percentage of tumor cells showing positive nuclear staining for Ki-67 among all the tumor cells counted. The fields for cell counting were selected randomly in the tumor area, and hot-spots of Ki-67-positive tumor cells were selected for assessing the Ki-67 labeling index; within this area, all tumor cells in each high-power field (× 400) were examined, and at least 500 tumor cells in each tumor were counted. The Ki-67 labeling index of stroma-invasive tumor cells was set at a threshold of 20% [31].
(A) Peripheral tumor budding grade 1 tumor cells. (B) Peripheral tumor budding grade 2 tumor cells. (C) Peripheral tumor budding grade 3 tumor cells. (D–G) Tumor budding in a fibrotic focus. (D) Fibrotic focus is indicated by arrows. (F) Invasive carcinoma no special type with an fibrotic focus. (E) Intra-tumor budding grade 1 tumor cells in an fibrotic focus. (G) Intra-tumor budding grade 3 tumor cells in an fibrotic focus. (D–G)
Statistical analysis and patient outcome
Survival was evaluated over a median follow-up period of 58.0 months (range: 1.8 to 149.0 months) until March 2019. Tumor recurrence, local recurrence (breast skin), distant-organ metastasis (bone: 15 cases; lung: 10 cases; liver: 8 cases; distant lymph node: 9 cases; brain: 1; stomach: 1; multiple organs, e.g., bone/lung, bone/liver: 18 cases) and tumor-related death occurred in 79, 17, 62, and 26, respectively, of the 855 patients with ICNST enrolled in this study. Univariate and multivariate analyses were performed using the Cox proportional hazard regression model to identify the outcome predictive power of each factor. Disease-free survival curves, local recurrence, distant-organ metastasis and tumor-related death survival curves were drawn using the Kaplan–Meier method. For analyzing the risk factors for tumor recurrence, since the luminal B/HER2-positive group and HER2-positive group had less than 10 cases with tumor recurrence (nine cases in the former group and eight cases in the latter group) each other, the two groups were combined for the analysis. In regard to analysis of the risk factors for local recurrence, 10 or more cases of local recurrence were observed in each of the following groups: (1) overall cases; (2) cases aged > 39 years; (3) cases with a Ki-67 labeling index of > 20%; (4) cases with histological grade 3 (Supplementary Table 1). Therefore, we analyzed the risk factors for local recurrence in each of these groups. Similar analysis of the risk factors for distant-organ metastasis and/or tumor-related death could not be performed in all the groups, as there were < 10 cases of distant-organ metastasis and/or tumor-related death some of the groups.
Results
Prognostic power of conventional tumor budding grade
Univariate analyses clearly demonstrated that progressive increase of the CTBG and of the TBG in the FF were associated with an increased risk of tumor recurrence, distant-organ metastasis, and tumor-related death, but not local recurrence (Table 1; Fig. 3A–D).
(A, B) Disease-free survival and tumor-related death survival periods decreased significantly with increasing peripheral tumor budding grade. (C, D) Disease-free survival and tumor-related death survival periods decreased significantly with increasing tumor budding grade in a fibrotic focus. HR, hazard ratio; CI, confidence interval; Gr., grade
Proposed system for tumor budding
Next, we attempted to develop a new grading system for tumor budding incorporating CTBG and the TBG in the FF in ICNSTs (Table 2). In cases without an FF, the CTBG was the final TB grade, while in cases with an FF, the TBG in the FF was added to the CTBG, e.g., in a case with an FF, CTB grade 2 and TB grade 2 in the FF were assigned a score of 4 (total TBG: 4) and finally classified into grade II of the proposed tumor budding grading system; in another case with an FF, CTB grade 3 and TB grade 3 in the FF were assigned a score of 6 (total TBG: 6) and finally classified into grade III of the proposed tumor budding grading system. The total TBG was classified into score 1 to 6; according to the results of univariate analysis performed to identify the predictors of tumor recurrence and tumor-related death, the score classes in the proposed tumor budding grading system (ProTBGS) were re-graded into grade I, grade II, and grade III (Table 2; Fig. 4A–D).
Prognostic power of the proposed tumor budding grading system
The abilities of the CTBG and ProTBGS to predict the clinical outcome were evaluated separately, along with those of well-known clinicopathological factors and tumor-infiltrating lymphocytes (%) (Supplementary Table 1) using model 1 (CTBG) and model 2 (ProTBGS), respectively.
Multivariate analysis using model 1 identified CTBG grade 3 as being associated with significantly increased hazard ratios for tumor recurrence and distant-organ metastasis, but not for local recurrence or tumor-related death (Table 3). Presence of an FF and presence of muscle invasion were significantly associated with tumor recurrence, distant-organ metastasis, and tumor-related death (Table 3). Histological grade 3 was significantly associated with local recurrence, distant-organ metastasis, and tumor-related death (Table 3). Multivariate analyses using model 2 identified ProTBGS grade III as being associated with significantly increased hazard ratios (as high as the presence of muscle invasion) for tumor recurrence, distant-organ metastasis, and tumor-related death (Table 3). Histological grade 3 was significantly associated with local recurrence and tumor-related death (Table 3).
Table 4 shows the factors that were found to be significantly associated with tumor recurrence and/or overall survival according to the UICC pTNM stages. In UICC pTNM stage I cases, analysis using model 1 identified CTBG grade 3 and a Ki-67 labeling index of ≧20% as being significantly associated with tumor recurrence, and analysis using model 2 identified ProTBGS grade III and a Ki-67 labeling index of ≧20% as being significantly associated with tumor recurrence. In UICC pTNM stage II, analysis using model 1 identified CTBG grade 3 as being associated with an increased hazard ratio for tumor recurrence, but not for distant-organ metastasis or tumor-related death; histological grade 3 was the only factor that was found to be associated with increased hazard ratios for tumor recurrence, distant-organ metastasis, and tumor-related death (Table 4). Analysis using model 2 identified ProTBGS grade III as the only factor associated with increased hazard ratios for tumor recurrence, distant-organ metastasis, and tumor-related death. In UICC pTNM stage III cases, analysis using model 1 identified hormone receptor status as the only factor significantly associated with tumor recurrence, distant-organ metastasis, and tumor-related death (Table 4). Analysis using model 1 failed to reveal any association between CTBG grade 3 and tumor recurrence, distant-organ metastasis, or tumor-related death; on the other hand, presence of an FF was associated with increased hazard ratios for distant-organ metastasis and tumor-related death (Table 4). Analysis using model 2 identified hormone receptor status as the only factor significantly associated with tumor recurrence, distant-organ metastasis, and tumor-related death (Table 4). Analysis using model 2 identified ProTBGS grade III as being significantly associated with tumor recurrence and distant-organ metastasis (Table 4).
Table 5 shows the factors that were found by multivariate analyses as being significantly associated with tumor recurrence and/or distant-organ metastasis, according to the intrinsic subtype of the tumor. Multivariate analyses using model 1 identified CTBG grade 3 as being associated with significantly increased hazard ratio for distant-organ metastasis only in cases with the luminal B/HER2-negative subtype of tumor (Table 5); multivariate analyses using model 2 clearly identified ProTBGS grade III as being associated with increased hazard ratios for tumor recurrence and distant-organ metastasis in patients with almost all intrinsic subtypes of tumor, except the basal-like subtype (Table 5).
Table 6 shows the factors that were significantly associated with tumor recurrence, local recurrence, distant-organ metastasis, and/or tumor-related death according to the patient age; in patients aged ≦39 years, analysis using model 1 failed to demonstrate an association of the CTBG with an increased hazard ratio for tumor recurrence or distant-organ metastasis, while histological grade 3 and radiotherapy were associated with significantly increased hazard ratios for tumor recurrence and distant-organ metastasis. Multivariate analysis using model 2 identified only ProTBGS grade III as being significantly associated with tumor recurrence and distant-organ metastasis (Table 6). In patients aged > 39 years, tumor-infiltrating lymphocytes > 19% was associated with significantly increased hazard ratios for tumor recurrence, distant-organ metastasis, and tumor-related death (Table 6). Multivariate analysis using model 1 identified CTBG grade 3 as well as the presence of an FF and a Ki-67 labeling index of ≧20% as being associated with increased hazard ratios for tumor recurrence and distant-organ metastasis (Table 6). Analysis using model 2 identified ProTBGS grade III and tumor-infiltrating lymphocytes (%) as being associated with significantly increased hazard ratios for tumor recurrence, distant-organ metastasis, and tumor-related death (Table 6).
Supplementary Table 3 shows the factors that were found by multivariate analyses as being significantly associated with tumor recurrence, local recurrence, distant-organ metastasis, and/or overall survival, according to the Ki-67 labeling index. In cases with a Ki-67 labeling index ≤ 20%, analysis using model 1 failed to demonstrate any significant association of the CTBG with increased hazard ratios for tumor recurrence or distant-organ metastasis; on the other hand, presence of FF, invasive tumor size > 50 mm, and age ≦39 years were associated with significantly increased hazard ratios for tumor recurrence and distant-organ metastasis (Supplementary Table 3). Multivariate analysis using model 2 identified ProTBGS grade III and invasive tumor size > 50 mm as being associated with increased hazard ratio for tumor recurrence and distant-organ metastasis (Supplementary Table 2). In cases with a Ki-67 labeling index of > 20%, CTBG grade 3 only significantly increased hazard ratio for tumor recurrence, while analysis using model 2 identified ProTBGS grade III as well as the presence of muscle invasion as being associated with increased hazard ratios for tumor recurrence, distant-organ metastasis, and tumor-related death (Supplementary Table 3).
Supplementary Table 4 shows the factors that were found by multivariate analyses as being significantly associated with tumor recurrence, local recurrence, distant-organ metastasis, and/or tumor-related death, according to histological grade. Multivariate analysis using model 1 failed to demonstrate any significant association of CTBG with tumor recurrence, local recurrence, distant-organ metastasis, or tumor-related death in histological grade 1, 2, and 3 group. Multivariate analysis using model 2 identified ProTBGS grade III as showing no significant association with tumor recurrence in cases with histological grade 1 tumors. In cases with histological grade 2 tumors, analysis using model 2 identified ProTBGS grade III as well as presence of muscle invasion and invasive tumor size > 50 mm as being associated with increased hazard ratios for tumor recurrence and distant-organ metastasis. In cases with histological grade 3 tumors, analysis using model 2 identified ProTBGS grade III as being associated with increased hazard ratio only for tumor-related death (Supplementary Table 4).
Discussion
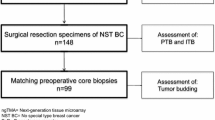
ProTBGS, which additionally incorporated the TBG in an FF, where present, as compared to CTBG, was clearly demonstrated to show superior ability for accurately predicting the outcomes in patients with ICNST of the breast (Table 7). As an FF is composed of cancer-associated fibroblasts, thus, ProTBGS also incorporates the aspect of tumor cell–stromal cell interaction within the FF [32,33,34], which have been reported as playing an important role in accelerating tumor progression in carcinomas of various organs [35,36,37]. We and others have previously reported that the FF is a very important prognostic parameter in patients with ICNST of the breast [8,9,10,11,12,13,14,15,16,17,18], and recently, tumor cell–stromal cell interactions have also been identified as playing important roles in colorectal carcinoma and pancreatic carcinoma [37,38,39]. In addition, in the present study, assessment by the ProTBGS was demonstrated to show superior power to that by the presence/absence of an FF alone for accurately predicting the outcome in patients with ICNST (Table 7); this probably indicates that assessment according to ProTBGS is superior to that by the presence/absence of an FF alone for accurate assessment of the characteristics of the tumor cells and tumor–stromal cell interaction in patients with ICNST. Thus, incorporation of tumor cell–stromal cell interactions in the evaluation is probably the reason why the outcome-predictive power of ProTBGS was found to be superior. Table 7 clearly demonstrates that the ProTBGS grade III was highly powerful for accurately predicting the clinical outcomes in patients with ICNSTs. Salhia et al. reported that intratumor budding (ITB) as well as peripheral tumor budding (PTB; equal to CTBG) were important prognostic factors in patients with invasive breast carcinoma, and that cases should be examined for both ITB and PTB [6]; we also investigated the prognostic power of ITB as well as PTB, and concluded that both tumor budding had almost similar prognostic power each other (Supplementary Table 5). Although ITB is probably an important prognostic indicator as well as PTB, ITB cannot reflect degree of tumor–stromal cell interaction in ICNST; in contrast, TBG in the FF can more accurately reflect degree of tumor–stromal cell interaction in ICNST than ITB. Therefore, we conducted to make a more powerful TB grading system than CTBG using TBG in the FF, and the results of the present study clearly revealed that ProTBGS was a superior TBG system to CTBG in patients with ICNST. Therefore, we concluded that the ProTBGS is the most reliable histological grading system for accurately predicting the outcomes in patients with ICNSTs of the breast. In the case of colorectal carcinoma, tumor budding is known as an independent predictor of survival in UICC stage II colorectal cancer patients [26]; ProTBGS grade III clearly demonstrated an excellent outcome-predictive power in patients with ICNST of the breast, independent of UICC pTNM stage, which strongly suggests that the incorporation of the tumor cell–stromal cell interactions enhance the outcome-predictive power of ProTBGS. Therefore, evaluation of the tumor budding grade in fibrotic tumor stroma, corresponding to the TBG in an FF in ICNSTs, in cases of colorectal cancer, pancreatic cancer, and other cancers may be very useful to analyze tumor cell nests and interactions of the tumor cells–stroma cells surrounding the tumor cell nests in colorectal cancer and other cancers [40,41,42,43,44].
Histological grade is the histological predictor of the outcome in patients with ICNST of the breast that is accepted worldwide [45]; the present study clearly demonstrated that assessment by the ProTBGS was superior to that of the histological grade for predicting the outcomes of patients with ICNST of the breast, and that the ProTBGS is also useful to accurately predict the outcomes of patients with ICNST of the breast of different histological grade. Thus, ProTBGS showed the best power among all histological parameters for predicting the outcomes in patients with ICNST; furthermore, use of the ProTBGS even allowed identification of patients with high-grade malignancy separately among patients classified as histological grade 1, 2, and 3. In addition, since ProTBGS is also a very useful outcome predictor in patients with ICNSTs independent of intrinsic subtype, patient age, or Ki-67 labeling index, we can conclude that ProTBGS is a very useful outcome predictor in patients with ICNNSTs, independent of the biological characteristics of the tumor/patients. Thus, we encourage pathologists to report ProTBGS in the routine pathological report of surgical material of ICNSTs of the breast, and in biopsy material [46], we suggest that the pathologist examine the TBG in the FF (resembling a fibrotic scar region within the fibrotic tumor stroma), if present within the ICNST, in addition to examining the CTB.
In conclusion, this study demonstrated that use of the ProTBGS is superior to that of CTBG, assessment of the histological grade, and assessment of the presence/absence of an FF for accurate prediction of the outcomes in patients with ICNST; therefore, ProTBGS is probably the most reliable histological grading system at present for predicting the prognosis in patients with ICNST of the breast. ProTBGS additionally incorporates assessment of TB in an FF, as compared to CTBG; this strongly suggests that the integrated actions of tumor-stromal fibroblasts forming an FF and tumor budding cells in the FF probably heighten the malignant potential of ICNSTs with an FF. Thus, factors that are produced by tumor cell–tumor stromal cell interactions should be investigated for the development of targeted therapies for patients with ICNST; ProTBGS may be very useful for histological selection of patients with ICNST for therapy targeted at tumor–stromal cell–tumor cell interactions.
Change history
29 December 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00428-022-03486-2
References
Ueno H, Murphy J, Jass JR, Mochizuki H, Talbot IC (2002) Tumor budding as an index to estimate the potential aggressiveness in rectal cancer. Histopathology 40:127–132
Wang LM, Kevans D, Mulcahy H, O’Sullivan J, Fennelly D, Hyland J et al (2008) Tumor budding is a strong and reproducible prognostic marker in T3N0 colorectal cancer. Am J Surg Pathol 33:134–141
Karamitopoulou E, Zlobec I, Kölzer V, Kondi-Pafiti A, Patsouris ES, Gennatas K et al (2013) Proposal for a 10-high-power-fields scoring method for the assessment of tumor budding in colorectal cancer. Mod Pathol 26:295–301
Koelzer VH, Zlobec I, Berger MD, Cathomas G, Dawson H, Dirschmid K et al (2015) Tumor budding in colorectal cancer revisited: results of a multicenter interobserver study. Virchows Arch 466:485–493
Liang F, Cao W, Wang Y, Li L, Zhang G, Wang Z (2013) The prognostic value of tumor budding in invasive breast cancer. Pathol Res Pract 209:269–275
Salhia B, Trippel M, Pfaltz K, Cihoric N, Grogg A, Lädrach G et al (2015) High tumor budding stratifies breast cancer with metastatic properties. Breast Cancer Res Treat 150:363–371
Li X, Wei B, Sonmez C, Li Z, Peng L (2017) High tumor budding count is associated with adverse clinicopathological features and poor prognosis in breast carcinoma. Hum Pathol 66:222–229
Hasebe T, Tsuda H, Tsubono Y, Imoto S, Mukai K (1997) Fibrotic focus in invasive ductal carcinoma: a histopathological prognostic parameter for tumor recurrence and tumor death within three years after the initial operation. Jpn J Cancer Res 88:590–599
Hasebe T, Sasaki S, Imoto S, Mukai K, Yokose T, Ochiai A (2002) Prognostic significance of fibrotic focus in invasive ductal carcinoma of the breast: a prospective observational study. Mod Pathol 15:502–516
Colpaert C, Vermeulen P, van Beest P, Goovaerts G, Weyler J, Dam PV et al (2001) Intratumoral hypoxia resulting in the presence of a fibrotic focus is an independent predictor of early distant relapse in lymph node-negative breast cancer patients. Histopathology 39:416–425
Baak JP, Colpaert CG, van Diest PJ, Janssen E, van Diermen B, Albernaz E et al (2005) Multivariate prognostic evaluation of the mitotic activity index and fibrotic focus in node-negative invasive breast cancers. Eur J Cancer 41:2093–2101
Van den Eynden GG, Smid M, Van Laere SJ, Colpaert CG, Van der Auwera I, Bich TX et al (2008) Gene expression profiles associated with the presence of a fibrotic focus and the growth pattern in lymph node-negative breast cancer. Clin Cancer Res 14:2944–2952
Maiorano E, Regan MM, Viale G, Mastropasqua MG, Colleoni M, Castiglione-Gertsch M et al (2010) Prognostic and predictive impact of central necrosis and fibrosis in early breast cancer: results from two International Breast Cancer Study Group randomized trials of chemoendocrine adjuvant therapy. Breast Cancer Res Treat 121:211–218
Kornegoor R, Verschuur-Maes AH, Buerger H, Hogenes MCH, de Bruin PC, Oudejans JJ et al (2012) Fibrotic focus and hypoxia in male breast cancer. Mod Pathol 25:1397–1404
Muitaba SS, Ni YB, Tsang JY, Chan SK, Yamaguchi R, Tanaka M et al (2013) Fibrotic focus in breast carcinomas: relationship with prognostic parameters and biomarkers. Ann Surg Oncol 20:2842–2849
Vermeulen MA, Slaets L, Cardoso F, Giordano SH, Tryfonidis K, van Diest PJ et al (2017) Pathological characterisation of male breast cancer: results of the EORTC 10085/TBCRC/BIG/NABCG International Male Breast Cancer Program. Eur J Cancer 82:219–227
Jeong YJ, Park SH, Mun SH, Kwak SG, Lee SJ, Oh HK et al (2018) Association between lysyl oxidase and fibrotic focus in relation with inflammation in breast cancer. Oncol Lett 15:2431–2440
Li Y, Wei Y, Tang W, Luo J, Wang M, Lin H et al (2019) Association between the degree of fibrosis in fibrotic focus and the unfavorable clinicopathological prognostic features of breast cancer. Peer J 7(1–18):e8067
Hasebe T, Iwasaki M, Akashi-Tanaka S, Hojo T, Shibata T, Sasajima Y et al (2010) p53 expression in tumor-stromal fibroblasts forming and not forming fibrotic foci in invasive ductal carcinoma of the breast. Mod Pathol 23:662–672
Jitsuiki Y, Hasebe T, Tsuda H, Imoto S, Tsubono Y, Sasaki S et al (1999) Optimizing microvessel counts according to tumor zone in invasive ductal carcinoma of the breast. Mod Pathol 12:492–498
Colpaert CG, Vermeulen PB, Fox SB, Harris AL, Dirix LY, Van Marc EA (2003) The presence of a fibrotic focus in invasive breast carcinoma correlates with the expression of carbonic anhydrase IX and is a marker of hypoxia and poor prognosis. Breast Cancer Res Treat 81:137–147
Brierley JD, Gospodarowicz MK (2017) Wittekind Ch: Union for International Cancer Control. TNM classification of malignant tumours. Eighth edition. UK, John Wiley & Sons, Ltd., 151–157
Denkert C, Loibl S, Noske A, Roller M, MüLLer BM, Komor M et al (2010) Tumor-associated lymphocytes as an independent predictor of response to neoadjuvant chemotherapy in breast cancer. J Clin Oncol 28:105–113
Denkert C, Wienert S, Poterie A, Loibl S, Budczies J, Badve S et al (2016) Standardized evaluation of tumor-infiltrating lymphocytes in breast cancer: results of the ring studies of the international immune-oncology biomarker working group. Mod Pathol 29:1155–1164
Hendry S, Salgado R, Gevaert T, Russell PA, John T, Thapa B et al (2017) Assessing tumor-infiltrating lymphocytes in solid tumors: a practical review for pathologists and proposal for a standardized method from the international immunooncology Biomarkers Working Group: Part 1: assessing the host immune response, TILs in invasive breast carcinoma and ductal carcinoma in situ, metastatic tumor deposits and areas for further research. Adv Anat Pathol 24:235–251
Lugli A, Kirsch R, Ajioka Y, Bosman F, Cathomas G, Dawson H et al (2016) Recommendations for reporting tumor budding in colorectal cancer based on the international tumor budding consensus conference (ITBCC). Mod Pahol 30:1299–1311
Allison KH, Hammond EH, Dowsett M, Mckernin SE, Carey LA, Fitzgibbons PL et al (2020) Estrogen and progesterone receptor testing in breast cancer: ASCO/CAP guideline update. J Clin Oncol 38:1346–1366
Wolff AC, Hammond EH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS et al (2018) Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline focused update. J Clin Oncol 36:2105–2122
Farshid G, Dhatrak D, Gilhotra A, Koszyca B, Nolan J (2020) The impact of 2018 ASCO-CAP HER2 testing guidelines on breast cancer HER2 results. An audit of 2132 consecutive cases evaluated by immunohistochemistry and in situ hybridization. Mod Pathol 33:1783–1790
Li A, Bai Q, Kong H, Zhou S, Hong Lv, Zhong S et al (2020) Impact of the updated 2018 American Society of Clinical Oncology/College of American Pathologists Guideline for human epidermal growth factor receptor 2 testing in breast cancer. Arch Pathol Lab Med 144:1097–1107
Bustero S, Osella-Abate S, Cassoni P, Donadio M, Airoldi M, Pedani F et al (2016) Optimal Ki67 cut-off for luminal breast cancer prognostic evaluation: a large cases series study with a long-term follow-up. Breast Cancer Res Treat 157:363–371
Vangagelt KMH, van Pelt GW, Engels CC, Putter H, Leifers GJ, Smit VTHBM et al (2018) Prognostic value of tumor–stroma ratio combined with the immune status of tumors in invasive breast carcinoma. Breast Cancer Res Treat 168:601–612
Strell C, Paulsson J, Jin SB, Tobin NP, Mezheyeuski A, Roswall P et al (2019) Impact of epithelial–stromal interactions on peritumoral fibroblasts in ductal carcinoma in situ. J Natl Cancer Inst 111:983–995
Vangangelt KMH, Green AR, Heemskerk I, Cohen D, van Pelt GW, Sobral-Leite M et al (2020) The prognostic value of the tumor–stroma ratio is most discriminative in patients with grade III or triple-negative breast cancer. Int J Cancer 146:2296–2304
Makino Y, Hikita H, Kodama T, Shigekawa M, Yamada R, Sakamori R et al (2018) CTGF mediates tumor-stroma interaction between hepatoma cells and hepatic stellate cells to accelerate HCC progression. Cancer Res 78:4902–4914
Costanza B, Rademaker G, Assia T, De Tullio P, Leenders J, Blomme A et al (2019) Transforming growth factor beta-induced, an extracellular matrix interacting protein, enhances glycolysis and promotes pancreatic cancer cell migration. Int J Cancer 145:1570–1584
Ouahoud S, Voomeveld PW, van der Burg LRA, de Jonge-Muller ESM, Schoonderwoerd MJA, Paauwe M et al (2020) Bidirectional tumor/stroma crosstalk promotes metastasis in mesenchymal colorectal cancer. Oncogene 39:2453–2466
Zunder SM, van Pelt GW, Gelderblom HJ, Mancao C, Putter H, Tollenaar RA et al (2018) Predictive potential of tumor-stroma ratio on benefit from adjuvant bevacizumab in high risk stage II and stage III colon cancer. Br J Cancer 119:164–169
Puleo F, Nicolle R, Blum Y, Cross J, Marisa L, Demetter P et al (2018) Stratification of pancreatic ductal adenocarcinoma based on tumor and microenvironment features. Gastroenterology 155:1999–2013
Kemi N, Eskuri M, Ikäläinen J, Karttunen T, Kauppila JH (2019) Tumor budding and prognosis in gastric adenocarcinoma. Am J Surg Pathol 43:229–234
Karamitopoulou E, Esposito I, Zlobec I, Isilla AC, Wartenberg M, Schaeffer DF et al (2021) Reproducibility of tumor budding assessment in pancreatic cancer based on a multicenter interobserver study. Vrichows Archiv 478:719–726
Kawamura K, Miyai K, Asakuma J, Sato K, Matsukuma S, Tsuda H, Ito K (2021) Tumor budding in upper urinary tract urothelial carcinoma: a putative prognostic factor for extraurothelial recurrence and overall survival. Virchows Arch 479:45–55
Kim HN, Lee SY, Kim BH, Kim CY, Kim A, Kim H (2021) Prognostic value of tumor budding in gallbladder cancer: application of the International Tumor Budding Consensus Conference scoring system. Virchows Arch 478:1071–1078
Lohneis P, Hieggelke L, Gebauer F, Ball M, Bruns C, Büttner R et al (2021) Tumor budding assessed according to the criteria of the International Tumor Budding Consensus Conference determines prognosis in resected esophageal adenocarcinoma. Virchows Arch 478:393–400
Rakha EA, Allison KH, Ellis IO, Horii R, Masuda S, Penault-Llorca F, Tsuda H, Vincent-Salomon A (2019) WHO classification of tumours. Breast tumours. Fifth edition. Lyon, International Agency for Research on Cancer, Ltd., 87–88
Almangush A, Youssef O, Pirinen M, Sundström J, Leivo I, Mäkitie AA (2019) Does evaluation of tumour budding in diagnostic biopsies have a clinical relevance? A systematic review. Histopathology 74:536–544
Acknowledgements
Naoe Akimoto provided technical assistance with the immunohistochemistry analyses in this study.
Funding
The present study was supported by the Hidaka Research Project from Saitama Medical University International Medical Center.
Author information
Authors and Affiliations
Contributions
M.H., T.H., and T.S. collected the clinical data, examined histopathological findings, performed the experiments, analyzed the data, participated in the study design, and wrote the manuscript. Y.I., A.S., A.F., N.A., N.W., M.Y., A.N., H.S., H.Y., K.M., T.H., and A.O. assisted in clinical data acquisition and revised the manuscript. S.S. and M.H. analyzed the data and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Compliance with ethical standards
All patients gave informed consent for retention and anonymous analysis of their tissue for research purpose in accordance with the requirements of the ethical committee of Saitama Medial University International Medical Center (Approval No. 18–314).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: the data "January 2007 and December 2015” (p. 162; seven line) was corrected to “April 2007 and December 2015".
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hiratsuka, M., Hasebe, T., Ichinose, Y. et al. Tumor budding and fibrotic focus—proposed grading system for tumor budding in invasive carcinoma no special type of the breast. Virchows Arch 481, 161–190 (2022). https://doi.org/10.1007/s00428-022-03337-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-022-03337-0