Abstract
Oligodendroglioma is defined by IDH mutation and 1p/19q codeletion. The latter is mutually exclusive to ATRX immunohistochemical loss and has been recently associated with the loss of H3K27me3 immunostaining. We aimed to assess the diagnostic and prognostic value of H3K27me3 immuno-expression in diffuse gliomas with oligodendroglial or mixed oligoastrocytic morphology. H3K27me3 immunostaining was performed in 69 diffuse gliomas with oligodendroglial (n = 62) or oligoastrocytic (n = 7) morphology. The integration with routinely assessed IDH mutations, ATRX immunostaining, and 1p/19q codeletion classified these cases as 60 oligodendroglial and 9 astrocytic. H3K27me3 was lost in 58/60 oligodendrogliomas with retained (n = 47) or non-conclusive (n = 11) ATRX staining, 3/6 IDH-mutant astrocytomas with ATRX loss, and 3/3 IDH-wt astrocytomas. H3K27me3 was retained in 2/60 oligodendrogliomas with retained ATRX, and in 3/6 IDH-mutant astrocytomas, two of which had lost and one retained ATRX. The combination of H3K27me3 and ATRX immunostainings with IDH mutational status correctly classified 55/69 (80%) cases. In IDH-mutant gliomas, ATRX loss indicates astrocytic phenotype, while ATRX retention and H3K27me3 loss identify oligodendroglial phenotype. Only 14 (20%) IDH-mutant cases with retained ATRX and H3K27me3 or inconclusive ATRX immunostaining would have requested 1p/19q codeletion testing to be classified. Furthermore, H3K27me3 retention was associated with significantly shorter relapse-free survival (P < 0.0001), independently from IDH mutation or 1p/19q codeletion (P < 0.005). Our data suggest that adding H3K27me3 immunostaining to the diagnostic workflow of diffuse gliomas with oligodendroglial or mixed morphology is useful for drastically reducing the number of cases requiring 1p/19q codeletion testing and providing relevant prognostic information.
Similar content being viewed by others
Introduction
The 2016 World Health Organization (WHO) classification of gliomas, by integrating histopathological features with molecular alterations, classifies astrocytic tumours based on the mutational status of IDH1/2 and H3K27M genes, while oligodendrogliomas are defined by the co-occurrence of IDH1/IDH2 mutation and codeletion of whole chromosomal arms 1p and 19q [1]. This classification is prognostically informative, as oligodendrogliomas IDH-mutant and 1p/19q codeleted have the best prognosis among diffuse gliomas, while IDH-wt astrocytic tumours the worst [2]. In addition, diffuse gliomas with 1p/19q codeletion are more likely to respond to chemotherapy [3, 4].
IDH mutations in gliomas occur more frequently at residue p.R132 of IDH1 and residue p.R172 of IDH2 [5]. About 90% are IDH1 R132H mutations that can be detected using a commercially available antibody against the mutant epitope [6], while 10% occur in other sites of IDH1 or IDH2 genes and can be currently identified only by DNA mutational analysis [2].
The WHO classification does not indicate a specific method to test 1p/19q codeletion but recommends that the assay should be able to detect whole-arm chromosomal losses [1], as the codeletion is mediated by a balanced whole-arm translocation of chromosomes 1 and 19 followed by the loss of one of the two derivative chromosomes composed of 1p and 19q [7]. Fluorescent in situ hybridization (FISH) is the most common method to assess 1p/19q codeletion [7]. However, this technique has shortcomings. First, it is unable to discriminate between complete and partial deletions of 1p and 19q because commercial probes hybridize to a minimal part of the chromosome arms, at 1p36 and 19q13 loci [8, 9]. Second, it cannot establish with certainty 1p/19q codeletion in the context of imbalanced aneuploidy, polyploidy, or polysomy [7, 9]. Other molecular methods, such as PCR-based LOH analysis, have higher specificity, but are more labour-intense and require a non-neoplastic control [7]. Therefore, the identification of surrogate markers of 1p/19q codeletion based on immunostaining may facilitate the differential diagnosis between astrocytoma and oligodendroglioma in routine practice.
In this context, it has been reported that the majority of IDH-mutant astrocytomas of all grades harbour truncating mutations in ATRX, which are mutually exclusive to 1p/19q codeletion and can be detected by the immunohistochemical loss of ATRX protein [2, 10, 11]. Thus, ATRX immunostaining has been suggested as an alternative low-cost marker to differentiate IDH-mutant astrocytomas from oligodendrogliomas [2, 10, 11]. Nonetheless, a proportion of IDH-mutant astrocytic tumours retain ATRX immunostaining [2, 12,13,14], and ATRX immunostaining has also been reported as non-conclusive in 11.5% of cases [14].
The immunohistochemical loss of histone 3 trimethylated in lysine 27 (H3K27me3) has been proposed to differentiate astrocytic from oligodendroglial neoplasms: diffuse gliomas can be classified astrocytic if retaining H3K27me3 expression, and oligodendroglial when showing H3K27me3 loss in association with mutated IDH and retained or non-conclusive ATRX staining [14]. This proposal stemmed from the finding of the immunohistochemical loss of H3K27me3 in 25/26 IDH-mutant and 1p/19q codeleted oligodendrogliomas and its retention in 120/135 astrocytomas [14]. A following study on 101 gliomas confirmed the significant association between H3K27me3 loss and 1p/19q codeletion but questioned its sensitivity and specificity [15].
We analysed H3K27me3 immunohistochemical expression in 69 diffuse gliomas with oligodendroglial or mixed oligoastrocytic morphology with the aim to clarify its diagnostic and prognostic potential, by assessing its correlation with 1p/19q codeletion and patients’ recurrence-free survival (RFS).
Materials and methods
Cases
We reviewed all cases operated between January 2014 and March 2020 at the University Hospital of Verona, Italy, and morphologically classified oligodendroglioma (OD), anaplastic oligodendroglioma (AOD), oligoastrocytoma (OAS), anaplastic oligoastrocytoma (AOAS), or glioblastoma with oligodendroglial component (GBM-O). A total of 69 cases, 62 with oligodendroglial (33 ODs and 29 AOs) and 7 with mixed morphology (4 OAS, 3 AOAS), were included in this study. All cases were classified according to WHO 2016 criteria [1]. None of the tumours was H3.3 K27M mutant.
Ethics
The study was approved by the local Ethics Committee (Comitato Etico per la Sperimentazione Clinica delle province di Verona e Rovigo; Prot. n. 11335, 02/26/2019) and performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Clinical data
Information on tumour localization, extent of surgical resection, and development of recurrence was retrieved using clinical records. Recurrence was defined by means of computerized tomography or magnetic resonance imaging as identification of tumour growth at the site of previous surgery, or as a volumetric increase of tumour residue in case of subtotal or partial surgery. RFS was defined as the length of survival to the detection of a recurrent tumour.
Immunohistochemistry
All cases were immunostained using antibodies against IDH1-R132H (clone H09, Dianova, GmbH, Germany; dilution 1:200), P53 (clone DO-7, Leica Biosystems, Newcastle, UK; prediluted), ATRX (Polyclonal; Life Science Sigma, St Louis, MO, USA; dilution 1:750), and H3K27me3 (clone C36B11, Cell Signaling Technology, Danvers, MA, USA; dilution 1:200), by means of an automated immunostainer (Leica Biosystems, Newcastle, UK).
ATRX expression was considered (i) retained, when nuclear staining was observed in both normal (endothelium, neurons) and neoplastic cells; (ii) lost, when staining was absent in neoplastic cells and present in normal cells; and (iii) non-conclusive, when staining was absent in both normal and neoplastic cells.
P53 immunostaining was assessed and scored as previously reported, and only cases with strong staining in at least 10% of neoplastic cells were rated p53 positive [16].
H3K27me3 immunohistochemical expression was classified according to Peckmezci et al. [15]: (i) retained, when nuclear staining was seen in ≥ 5% neoplastic cells; (ii) lost, when staining was absent in > 95% neoplastic cells and present in internal positive controls (endothelium, neurons); and (iii) non-conclusive, when staining was absent in both normal and neoplastic cells.
IDH1/2 mutational analysis
In cases with negative immunostaining for IDH1-R132H, we assessed IDH1/2 mutational status. Briefly, neoplastic cellularity was enriched to at least 70% by manual microdissection of 10 consecutive 4 μm sections. DNA was purified using the QIAamp DNA FFPE Tissue Kit (Qiagen) and qualified as reported [17]. IDH1 and IDH2 were amplified by PCR, and both strands were sequenced using the ABI PRISM 3500 Genetic Analyzer (Applied Biosystems). PCR conditions were (1) denaturation at 95 °C for 5 min; (2) 40 cycles at 95 °C/30 s, 58 °C/30 s, and 72 °C/30 s; and (3) elongation step at 72 °C/5 min. Primers used were IDH1-F CCATCACTGCAGTTGTAGGTT, IDH1-R GCAAAATCACATTATTGCCAAC, IDH2-F TGCAGTGGGACCACTATTATC, and IDH2-R GTGCCCAGGTCAGTGGAT.
Chromosome arms 1p/19q codeletion analysis
FISH was used to assess 1p/19q codeletion. For each case, two consecutive 3-μm sections were processed with LSI 1p36/19q13 Dual-Colour Probe Sets assay (Vysis/Abbott, Molecular Europe, Wiesbaden, Germany), following manufacturer’s protocol. Slides were examined by Olympus BX61 fluorescence microscope equipped with a ×100 oil immersion objective and a triple band pass filter for simultaneous detection of Spectrum Orange, Spectrum Green, and DAPI signals. Two hundred non-overlapping nuclei containing a minimum of 2 reference probe signals were counted.
Cases were classified as (i) 1p/19q codeleted, when showing two reference probe signals (1q and 19p) and one target probe signal (1p and 19q) in at least 50% cells; (ii) non-codeleted, when having two reference probe signals (1q and 19p) and two target probe signals in > 50% cells; and (iii) imbalanced, when > 50% cells had a ratio of reference to probe signal different from 2/2 or 2/1 [18].
Cases with imbalanced 1p/19q status or IDH-wt and1p/19q codeleted at FISH analysis were further analysed using loss of heterozygosity (LOH) analysis. In detail, LOH was performed using tumour and normal DNA pairs extracted from paraffin-embedded tissue sections and evaluated by PCR-based LOH assays. Allelic loss analysis was performed using the microsatellite markers D1S508, D1S199, and D1S2734 on chromosome 1p, and D19S412, D19S112, and D19S219 on chromosome 19q. Forward primers were synthesized either with fluorescent tag FAM or HEX. PCR products were subjected to electrophoresis on an Applied Biosystems 310 automated DNA sequencer (Applied Biosystems, Italy) and fluorescent signals analysed using GeneScan software (Applied Biosystems). Allelic imbalance was evaluated by comparing PCR products from tumour and normal DNA. Peak height ratio was calculated, and allelic imbalance resulted from the ratio of normal to tumour signal (N1/N2 over T1/T2). LOH was assigned for values less than or equal to 0.5 and 1.5. Procedures were repeated three times and allelic losses assigned only upon consistency of the findings.
MGMT promoter methylation analysis
The methylation status of O-6-methylguanine-DNA methyltransferase (MGMT) promoter was assessed in all cases. Briefly, 200 ng of DNA was incubated using sodium bisulphate included in EpiTect Plus FFPE Bisulfite Kit (Qiagen) and analysed using pyrosequencing through MGMT Plus kit (Diatech). The assay performs a quantitative analysis of the percentage of methylation of each of the 10 CpG islands located on chr10. Samples were stratified in four groups according to the extension of methylation status that has been related to clinical outcome: unmethylated (< 9%), low (range 9–20%), medium (21–35%), and high level (over 35%) [19].
Statistical analysis
Considering only 66 IDH-mutant tumours, we calculated the sensitivity [true positive/(true positive + false negative)] and specificity [true negative/(true negative + false positive)] of ATRX+ vs ATRX+/H3K27me3−, for the identification of oligodendrogliomas.
Considering all the 69 tumours, we also calculated the sensitivity and specificity of ATRX− vs H3K27me3+ for the identification of astrocytomas.
RFS was assessed by the Kaplan-Meier method, with the date of primary surgery as the entry data and length of survival to the detection of a recurrent tumour as the end point. The Mantel-Cox log-rank test was applied to assess the strength of association between RFS and each of the parameters as a single variable. A probability (P) value less than 0.05 was considered significant. Statistical analyses were performed using MedCalc 12.1.4.0 statistical software (MedCalc Software, Mariakerke, Belgium).
Results
The results are detailed in Fig. 1 and summarized in Supplementary Figure 1.
Clinical-pathological, immunohistochemical, and molecular features of 69 diffuse gliomas with oligodendroglial or mixed oligoastrocytic morphology. M, male; F female; OD, oligodendroglioma; AOD, anaplastic oligodendroglioma; OAS, oligoastrocytoma; AOAS, anaplastic oligoastrocytoma; DA, diffuse astrocytoma; GBM, glioblastoma; Wt, wild type; N.c., non-conclusive
Cases
All tumours were newly diagnosed gliomas with cerebral lobe localization, except for case 56, which was localized in the cerebellum. All neoplasms had gross total resection with the exception of case 15 that had subtotal resection. No patient had been treated with neo-adjuvant therapies. Forty-five patients were males and 24 females with mean age of 45 ± 11.6 years.
IDH mutational status
Sixty-six of the 69 gliomas were IDH-mutant: 61 had IDH1 R132H mutations detected by immunohistochemistry (IHC); 5 had IDH2 mutations detected at sequencing analysis, including 2 ODs and 1 AOD with a R172K mutation and 2 AODs with a R172M mutation.
1p/19q codeletion by FISH and LOH analysis
Sixty of the 66 IDH-mutant gliomas were classified 1p/19q codeleted based on FISH and/or LOH analysis.
At FISH analysis of the 66 IDH-mutant cases, 57 had 1p/19q codeletion in > 50% cells and were classified 1p/19q codeleted; 5 were classified non-codeleted, and 4 cases had imbalanced 1p/19q. Of the 3 IDH-wt gliomas, 1 had imbalanced 1p/19q and 2 had 1p/19q codeletion.
The 7 cases with questionable 1p/19q status at FISH analysis, including 4 IDH-mutant and 3 IDH-wt, were further assessed by molecular LOH analysis (Table 1). Of the 4 IDH-mutant gliomas with imbalanced 1p/19q, 3 were codeleted and 1 non-codeleted. All 3 IDH-wt gliomas resulted non-codeleted.
Integrated diagnosis
Based on the assessment of IDH mutational status and 1p/19q codeletion, the cases were classified as follows: 33 ODs and 27 AODs IDH-mutant and 1p/19q codeleted; 4 diffuse astrocytomas (DAs) IDH-mutant; 2 GBMs IDH-mutant; and 3 GBMs IDH-wt (Fig. 1 and Supplementary Figure 1).
ATRX and p53 immunohistochemistry
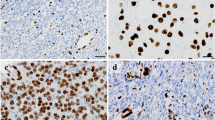
Of the 60 oligodendroglial (1p/19q codeleted) tumours, 49 retained ATRX immunohistochemical expression and 11 had a non-conclusive staining; 57 had a negative and 3 had a positive P53 staining; 58 lost and 2 retained H3K27me3 expression (Figs. 1 and 2; Supplementary Figure 1).
ATRX, p53, and H3K27me3 immunohistochemical expression in one astrocytoma and one oligodendroglioma. The IDH-mutant astrocytoma shows neoplastic nuclei with loss of ATRX, positivity for p53, and retained H3K27me3 immunostainings. The oligodendroglioma IDH-mutant and 1p/19q codeleted shows neoplastic nuclei with retained ATRX, scattered p53-positivity, and loss of H3K27me3 immunostaining
Of the 9 astrocytic tumours, 5 lost ATRX, 3 retained its expression, and 1 had non-conclusive staining; 8 were P53 negative and 1 was positive; 4 lost and 5 retained H3K27me3 expression (Fig. 1 and Supplementary Figure 1).
H3K27me3 immunohistochemistry
H3K27me3 loss was significantly associated with the retention of ATRX immuno-expression (P = 0.025), 1p/19q codeletion (P = 0.0001), and negative P53 (P = 0.0027) (Supplementary Table 1).
MGMT promoter methylation analysis
MGMT promoter was methylated in 58/60 oligodendroglial tumours (5 low, 21 intermediate, and 32 high level), in 4 IDH-mutant astrocytic (2 intermediate and 2 high level), and in 2 IDH-wt (1 low and 1 intermediate level). MGMT promoter methylation was more frequent in gliomas with H3K27me3 loss, but statistical significance was not reached (Supplementary Table 1).
Sensitivity and specificity of ATRX and H3K27me3 immunostaining
In IDH-mutant tumours, ATRX+ was 100% sensitive and 87% specific to oligodendrogliomas, while ATRX+/H3K27me3− was 96% sensitive and 100% specific (Supplementary Table 2).
ATRX immunohistochemical loss was 62% sensitive and 100% specific for astrocytic tumours, while H3K27me3+ was 44% sensitive and 97% specific (Supplementary Table 3).
IDH-mutant tumours with non-conclusive ATRX staining were excluded from the calculation.
Proposed diagnostic algorithm
Based on our results, we propose the diagnostic algorithm illustrated in Fig. 3. IDH1-R132H, ATRX, and H3K27me3 immunostainings should be assessed first. Then, based on the immunohistochemical results, (i) cases with ATRX loss are classified astrocytic; (ii) cases positive for IDH1-R132H with retained ATRX and lost H3K27me3 are classified oligodendroglial; and (iii) cases positive for IDH1-R132H with non-conclusive ATRX or retained ATRX and H3K27me3 should be tested for 1p/19q codeletion. Cases with negative IDH1-R132H staining should be analysed for IDH1/2 mutations to complete the evaluation.
Proposed diagnostic algorithm for diffuse gliomas. Diffuse gliomas are classified starting with the assessment of IDH1 R132H, ATRX, and H3K27me3 immunostainings. Cases with ATRX loss are classified astrocytic, while those positive for IDH1 R132H and with retained ATRX and lost H3K27me3 stain are classified oligodendroglial. Cases with negative IDH1 R132H are tested for other IDH1/2 mutations: the IDH-wt is classified astrocytic, while the IDH-mutant with retained ATRX and lost H3K27me3 is classified oligodendroglial. The assessment of 1p/19q codeletion is reserved to IDH-mutant tumours with retained ATRX and H3K27me3 immunostainings or non-conclusive ATRX. Using this approach in the present study, 55/69 cases would have been classified correctly without 1p/19q codeletion testing, which would have been needed in only 14 cases
Applying this algorithm to our series, 47 (68%) cases would have been classified astrocytic or oligodendroglial using only immunohistochemistry for IDH1-R132H, ATRX, and H3K2727me3, 8 (12%) cases would have been resolved with IDH1/2 molecular testing, while only 14 (20%) of the 69 cases would have requested the assessment of 1p/19q codeletion by FISH or PCR-microsatellite LOH analysis (Supplementary Figure 2).
Recurrence-free survival analysis
Follow-up data were available for 50 patients. Seven patients had a recurrence, with a RFS ranging between 18 and 47 months (median: 30 months; inter-quartile range: 24–41 months). The remaining 43 patients were free of recurrence in a follow-up period ranging between 6 and 80 months (median: 33 months; inter-quartile range: 17.5–44 months) (Fig. 1).
Of the 7 gliomas that relapsed, 5 retained H3K27me3 immunohistochemical expression (P < 0.0001) (Supplementary Table 1).
Patients harbouring a tumour with retained H3K27me3, IDH-wt, lack of 1p/19q codeletion, or grade IV had significantly shorter RFS (Fig. 4; Supplementary Table 4). Multivariate analysis, including IDH mutational status, 1p/19q codeletion, histological grade, and H3K27me3 staining as covariates, showed H3K27me3 immunohistochemical expression as the only significant and independent predictor of RFS (hazard ratio: 38; confidence interval: 2.9.1–513; P = 0.005) (Supplementary Table 4).
Discussion
The diagnosis of oligodendroglioma requires the coexistence of IDH1/2 mutation and 1p/19q codeletion [1]. This latter is assessed in most pathology laboratories by FISH, which is time and expertise demanding [7]. Thus, finding surrogate immunohistochemical markers of 1p/19q codeletion could avoid expensive and unnecessary tests [20].
The results of our study suggest that this can be achieved applying an algorithm that starts with the assessment of IDH mutations associated with ATRX and H3K27me3 immunostainings. This approach would reserve 1p/19q codeletion testing only to IDH-mutant gliomas with retention of both ATRX and H3K27me3 or non-conclusive ATRX immunostainings.
The proposed algorithm is based on our observation that ATRX loss was 100% specific to the astrocytic phenotype, which confirms the data repeatedly reported in the literature [2, 13, 21], and that the co-occurrence of retained ATRX and loss of H3K27me3 in IDH-mutant gliomas was 100% specific to oligodendroglial phenotype.
The utility of H3K27me3 immunostaining in the differential diagnosis between oligodendroglioma and astrocytoma was first reported by Filipski et al. [14], who suggested that H3K27me3 retention indicates astrocytic (non-codeleted) tumours with a predicted probability of 0.9995, while its loss in IDH-mutant gliomas with retained or non-conclusive ATRX stain is 100% specific for oligodendrogliomas [14].
Although the association between the loss of H3K27me3 immuno-expression and 1p/19q codeletion was confirmed in three independent studies [15, 22, 23], Peckmezci et al. found retained H3K27me3 in 7/28 (25%) oligodendrogliomas, and the co-occurrence of H3K27me3 loss and retained or non-conclusive ATRX staining in 7/74 (10%) IDH-mutant astrocytomas [15]. This latter study therefore questioned the assumptions of Filipski et al. that H3K27me3 retention can be used as the sole evidence against 1p/19q codeletion, and that the co-occurrence of H3K27me3 loss and retained or non-conclusive ATRX in IDH-mutant gliomas is specific to oligodendrogliomas [15]. The discrepancy between the results of Peckmezci et al. [15] and those of Filipski et al. [14] could be partially explained by the use of different working dilutions of the same anti-H3K27me3 antibody (clone C36 B11) they used (1:50 vs 1:200). Indeed, Kitahama et al. demonstrated that the higher the antibody dilution, the higher the specificity in recognizing oligodendrogliomas [23].
In the present study, we performed H3K27me3 immunostaining using the same antibody clone of Filipski et al. [14] and Peckmezci et al. [15] at the 1:200 working dilution used by Filipski et al. [14]. Our data confirm that H3K27me3 loss is significantly related to both 1p/19q codeletion and ATRX retention.
The protocol that we suggest differs from that of Filipski et al. in that the latter classifies all tumours with retained H3K27me3 as astrocytic, with no additional tests [14], while cases with H3K27me3 loss are tested for ATRX and IDH mutations, and those IDH-mutant with retained or non-conclusive ATRX are considered oligodendroglial [14]. Using the protocol of Filipski et al. on our series, 2 AODs would have been misclassified as astrocytomas as they retained H3K27me3, while using our proposed diagnostic flowchart, we would have correctly diagnosed as oligodendroglial or astrocytic all cases. In particular, 47 of 69 (68%) cases would have been solved with immunostaining for IDH1-R132H, ATRX, and H3K2727me3. Mutational analysis of IDH1-negative cases would have solved 8 (12%) additional cases; thus, 1p/19q codeletion analysis would have been limited to only 14 (20%) of the 69 diffuse gliomas with oligodendroglial or mixed morphology. Noteworthy, all our IDH2-mutant gliomas resulted oligodendroglial, reinforcing the reported association between IDH2 mutations and 1p/19q codeletion in diffuse gliomas [24, 25].
In this respect, it is important to note that our study was limited to diffuse gliomas with oligodendroglial or mixed oligoastrocytic morphology, because IDH-mutant astrocytic-appearing tumours with ATRX loss can be confidently diagnosed as astrocytic without the need for 1p/19q codeletion testing [21]. Furthermore, the key role of morphology in guiding immunostaining and molecular tests is also highlighted by our study in which the morphological diagnosis was confirmed by the molecular data in 58/69 (84%) cases, while it was modified in 11 (16%) cases.
Reducing the need for 1p/19q testing reduces not only costs but also the pitfalls associated with it. The widely used FISH analysis has difficulties of interpretation in the case of imbalanced 1p/19q status and the impossibility to discriminate between complete and partial loss of chromosomal arms [7]. Despite high concordance with other molecular techniques, such as PCR-microsatellite LOH analysis, FISH has not only a lower sensitivity in detecting whole-arm 1p/19q losses [7] but also a lower specificity due to false positive astrocytomas with partial chromosomal losses [26, 27].
The limitations of FISH were also evident in our study, where its results were deceiving in 7/69 (10%) cases, including the interpretation of five cases with imbalanced 1p/19q and two IDH-wt false positive gliomas. The five gliomas with imbalanced 1p/19q status resulted codeleted (3 cases) or non-codeleted (2 cases) at PCR-microsatellite LOH analysis. Noteworthy, our protocol would have correctly identified 4 of these 5 cases with imbalanced 1p/19q using ATRX and H3K27me3 immunostainings, and only one case would have requested 1p/19q testing. The false positive results in the two IDH-wt gliomas are easily avoided as IDH-wt gliomas are diagnosed as astrocytic without further testing [1].
H3K27me3 stain also proved to be prognostically informative. Namely, retention of H3K27me3 was significantly associated with the development of recurrent disease and with a shorter RFS, independently from IDH mutational status and 1p/19q codeletion. Indeed, all 5 gliomas with retained H3K27me3 and only 2/45 with H3K27me3 loss recurred. This corroborates the previously reported association between H3K27me3 loss and a longer survival in 58 patients with diffuse gliomas [14], and demonstrates that in these tumours, H3K27me3 has a prognostic significance opposite to that found in meningiomas or ependymomas, where its retention associates with a better prognosis [28, 29].
In conclusion, the present study shows that the introduction of H3K27me3 immunohistochemistry to the diagnostic algorithm of diffuse gliomas with oligodendroglial morphology may be useful to predict 1p/19q codeletion status and provide relevant prognostic information. Our study strongly suggests that in IDH-mutant gliomas, ATRX loss indicates astrocytic phenotype, ATRX retention, and H3K27me3 loss indicate oligodendroglial phenotype, while retained or non-conclusive ATRX and retained H3K27me3 mandate for 1p/19q codeletion testing. Finally, the loss of H3K27me3 is associated with a significantly better prognosis, independently from 1p/19q codeletion and IDH mutational status.
Data availability
Data will be available upon request to the corresponding author.
References
Louis DN, Ohgaki H, Wisteler OD, Cavenee WK, Ellison DW, Figarella-Branger D, Perry A, Refeinberger G, von Deimling A (2016) WHO classification of tumors of the central nervous system. IARC, Lyon
Reuss DE, Sahm F, Schrimpf D, Wiestler B, Capper D, Koelsche C, Schweizer L, Korshunov A, Jones DT, Hovestadt V, Mittelbronn M, Schittenhelm J, Herold-Mende C, Unterberg A, Platten M, Weller M, Wick W, Pfister SM, von Deimling A (2015) ATRX and IDH1-R132H immunohistochemistry with subsequent copy number analysis and IDH sequencing as a basis for an “integrated” diagnostic approach for adult astrocytoma, oligodendroglioma and glioblastoma. Acta Neuropathol 129:133–146. https://doi.org/10.1007/s00401-014-1370-3
Cairncross G, Wang M, Shaw E, Jenkins R, Brachman D, Buckner J, Fink K, Souhami L, Laperriere N, Curran W, Mehta M (2013) Phase III trial of chemoradiotherapy for anaplastic oligodendroglioma: long-term results of RTOG 9402. J Clin Oncol 31:337–343. https://doi.org/10.1200/JCO.2012.43.2674
van den Bent MJ, Brandes AA, Taphoorn MJ, Kros JM, Kouwenhoven MC, Delattre JY, Bernsen HJ, Frenay M, Tijssen CC, Grisold W, Sipos L, Enting RH, French PJ, Dinjens WN, Vecht CJ, Allgeier A, Lacombe D, Gorlia T, Hoang-Xuan K (2013) Adjuvant procarbazine, lomustine, and vincristine chemotherapy in newly diagnosed anaplastic oligodendroglioma: long-term follow-up of EORTC brain tumor group study 26951. J Clin Oncol 31:344–350. https://doi.org/10.1200/JCO.2012.43.2229
Park JW, Turcan S (2019) Epigenetic reprogramming for targeting IDH-mutant malignant gliomas. Cancers (Basel) 11. https://doi.org/10.3390/cancers11101616
Capper D, Weissert S, Balss J, Habel A, Meyer J, Jager D, Ackermann U, Tessmer C, Korshunov A, Zentgraf H, Hartmann C, von Deimling A (2010) Characterization of R132H mutation-specific IDH1 antibody binding in brain tumors. Brain Pathol 20:245–254. https://doi.org/10.1111/j.1750-3639.2009.00352.x
Woehrer A, Hainfellner JA (2015) Molecular diagnostics: techniques and recommendations for 1p/19q assessment. CNS Oncol 4:295–306. https://doi.org/10.2217/cns.15.28
Idbaih A, Kouwenhoven M, Jeuken J, Carpentier C, Gorlia T, Kros JM, French P, Teepen JL, Delattre O, Delattre JY, van den Bent M, Hoang-Xuan K (2008) Chromosome 1p loss evaluation in anaplastic oligodendrogliomas. Neuropathology 28:440–443. https://doi.org/10.1111/j.1440-1789.2008.00863.x
Pinkham MB, Telford N, Whitfield GA, Colaco RJ, O'Neill F, McBain CA (2015) FISHing tips: what every clinician should know about 1p19q analysis in gliomas using fluorescence in situ hybridisation. Clin Oncol (R Coll Radiol) 27:445–453. https://doi.org/10.1016/j.clon.2015.04.008
Ikemura M, Shibahara J, Mukasa A, Takayanagi S, Aihara K, Saito N, Aburatani H, Fukayama M (2016) Utility of ATRX immunohistochemistry in diagnosis of adult diffuse gliomas. Histopathology 69:260–267. https://doi.org/10.1111/his.12927
Kannan K, Inagaki A, Silber J, Gorovets D, Zhang J, Kastenhuber ER, Heguy A, Petrini JH, Chan TA, Huse JT (2012) Whole-exome sequencing identifies ATRX mutation as a key molecular determinant in lower-grade glioma. Oncotarget 3:1194–1203. https://doi.org/10.18632/oncotarget.689
Barresi V, Eccher A, Simbolo M, Cappellini R, Ricciardi GK, Calabria F, Cancedda M, Mazzarotto R, Bonetti B, Pinna G, Sala F, Ghimenton C, Scarpa A (2020) Diffuse gliomas in patients aged 55 years or over: a suggestion for IDH mutation testing. Neuropathology 40:68–74. https://doi.org/10.1111/neup.12608
Leeper HE, Caron AA, Decker PA, Jenkins RB, Lachance DH, Giannini C (2015) IDH mutation, 1p19q codeletion and ATRX loss in WHO grade II gliomas. Oncotarget 6:30295–30305. https://doi.org/10.18632/oncotarget.4497
Filipski K, Braun Y, Zinke J, Roller B, Baumgarten P, Wagner M, Senft C, Zeiner PS, Ronellenfitsch MW, Steinbach JP, Plate KH, Gasparoni G, Mittelbronn M, Capper D, Harter PN (2019) Lack of H3K27 trimethylation is associated with 1p/19q codeletion in diffuse gliomas. Acta Neuropathol 138:331–334. https://doi.org/10.1007/s00401-019-02025-9
Pekmezci M, Phillips JJ, Dirilenoglu F, Atasever-Rezanko T, Tihan T, Solomon D, Bollen A, Perry A (2020) Loss of H3K27 trimethylation by immunohistochemistry is frequent in oligodendroglioma, IDH-mutant and 1p/19q-codeleted, but is neither a sensitive nor a specific marker. Acta Neuropathol 139:597–600. https://doi.org/10.1007/s00401-019-02123-8
Takami H, Yoshida A, Fukushima S, Arita H, Matsushita Y, Nakamura T, Ohno M, Miyakita Y, Shibui S, Narita Y, Ichimura K (2015) Revisiting TP53 mutations and immunohistochemistry--a comparative study in 157 Diffuse Gliomas. Brain Pathol 25:256–265. https://doi.org/10.1111/bpa.12173
Simbolo M, Gottardi M, Corbo V, Fassan M, Mafficini A, Malpeli G, Lawlor RT, Scarpa A (2013) DNA qualification workflow for next generation sequencing of histopathological samples. PLoS One 8:e62692. https://doi.org/10.1371/journal.pone.0062692
Woehrer A, Sander P, Haberler C, Kern S, Maier H, Preusser M, Hartmann C, Kros JM, Hainfellner JA, Research Committee of the European Confederation of Neuropathological S (2011) FISH-based detection of 1p 19q codeletion in oligodendroglial tumors: procedures and protocols for neuropathological practice - a publication under the auspices of the Research Committee of the European Confederation of Neuropathological Societies (Euro-CNS). Clin Neuropathol 30:47–55. https://doi.org/10.5414/npp30047
Dunn J, Baborie A, Alam F, Joyce K, Moxham M, Sibson R, Crooks D, Husband D, Shenoy A, Brodbelt A, Wong H, Liloglou T, Haylock B, Walker C (2009) Extent of MGMT promoter methylation correlates with outcome in glioblastomas given temozolomide and radiotherapy. Br J Cancer 101:124–131. https://doi.org/10.1038/sj.bjc.6605127
Barresi V, Mondello S, Branca G, Rajan TS, Vitarelli E, Tuccari G (2015) p-CREB expression in human gliomas: potential use in the differential diagnosis between astrocytoma and oligodendroglioma. Hum Pathol 46:231–238. https://doi.org/10.1016/j.humpath.2014.10.011
Louis DN, Giannini C, Capper D, Paulus W, Figarella-Branger D, Lopes MB, Batchelor TT, Cairncross JG, van den Bent M, Wick W, Wesseling P (2018) cIMPACT-NOW update 2: diagnostic clarifications for diffuse midline glioma, H3 K27M-mutant and diffuse astrocytoma/anaplastic astrocytoma, IDH-mutant. Acta Neuropathol 135:639–642. https://doi.org/10.1007/s00401-018-1826-y
Feller C, Felix M, Weiss T, Herold-Mende C, Zhang F, Kockmann T, Sahm F, Aebersold R, von Deimling A, Reuss DE (2020) Histone epiproteomic profiling distinguishes oligodendroglioma, IDH-mutant and 1p/19q co-deleted from IDH-mutant astrocytoma and reveals less tri-methylation of H3K27 in oligodendrogliomas. Acta Neuropathol 139:211–213. https://doi.org/10.1007/s00401-019-02096-8
Kitahama K, Iijima S, Sumiishi A, Hayashi A, Nagahama K, Saito K, Sasaki N, Kobayashi K, Shimizu S, Nagane M, Shibahara J (2021) Reduced H3K27me3 levels in diffuse gliomas: association with 1p/19q codeletion and difference from H3K27me3 loss in malignant peripheral nerve sheath tumors. Brain Tumor Pathol 38:23–29. https://doi.org/10.1007/s10014-020-00382-y
Appay R, Tabouret E, Macagno N, Touat M, Carpentier C, Colin C, Ducray F, Idbaih A, Mokhtari K, Uro-Coste E, Dehais C, Figarella-Branger D, Network P (2018) IDH2 mutations are commonly associated with 1p/19q codeletion in diffuse adult gliomas. Neuro-Oncology 20:716–718. https://doi.org/10.1093/neuonc/noy014
Visani M, Acquaviva G, Marucci G, Paccapelo A, Mura A, Franceschi E, Grifoni D, Pession A, Tallini G, Brandes AA, de Biase D (2017) Non-canonical IDH1 and IDH2 mutations: a clonal and relevant event in an Italian cohort of gliomas classified according to the 2016 World Health Organization (WHO) criteria. J Neuro-Oncol 135:245–254. https://doi.org/10.1007/s11060-017-2571-0
Ball MK, Kollmeyer TM, Praska CE, McKenna ML, Giannini C, Raghunathan A, Jentoft ME, Lachance DH, Kipp BR, Jenkins RB, Ida CM (2020) Frequency of false-positive FISH 1p/19q codeletion in adult diffuse astrocytic gliomas. Neurooncol Adv 2:vdaa109. https://doi.org/10.1093/noajnl/vdaa109
Alnahhas I, Rayi A, Thomas D, Ong S, Giglio P, Puduvalli V (2020) False-positive 1p/19q testing results in gliomas: clinical and research consequences. Am J Clin Oncol 43:802–805. https://doi.org/10.1097/COC.0000000000000755
Bayliss J, Mukherjee P, Lu C, Jain SU, Chung C, Martinez D, Sabari B, Margol AS, Panwalkar P, Parolia A, Pekmezci M, McEachin RC, Cieslik M, Tamrazi B, Garcia BA, La Rocca G, Santi M, Lewis PW, Hawkins C, Melnick A, David Allis C, Thompson CB, Chinnaiyan AM, Judkins AR, Venneti S (2016) Lowered H3K27me3 and DNA hypomethylation define poorly prognostic pediatric posterior fossa ependymomas. Sci Transl Med 8:366ra161. https://doi.org/10.1126/scitranslmed.aah6904
Katz LM, Hielscher T, Liechty B, Silverman J, Zagzag D, Sen R, Wu P, Golfinos JG, Reuss D, Neidert MC, Wirsching HG, Baumgarten P, Herold-Mende C, Wick W, Harter PN, Weller M, von Deimling A, Snuderl M, Sen C, Sahm F (2018) Loss of histone H3K27me3 identifies a subset of meningiomas with increased risk of recurrence. Acta Neuropathol 135:955–963. https://doi.org/10.1007/s00401-018-1844-9
Funding
Open access funding provided by Università degli Studi di Verona within the CRUI-CARE Agreement. FUR 2019, University of Verona, Italy, to VB; Associazione Italiana Ricerca sul Cancro (AIRC n. 12182) to AS.
Author information
Authors and Affiliations
Contributions
S.A: revision of histological slides, data collection, interpretation of the results, and original draft writing. N.C.: revision of histological slides, data collection, interpretation of the results, and draft revision. M.S., M.L.P.: molecular analyses and draft revision. M.B.: FISH analysis, interpretation of the results, and draft revision. P.L.P.: LOH analysis, interpretation of the results, and draft revision. G.P. and F.S.: collection of clinical data and draft revision. C.G.: data collection and draft revision. A.S.: interpretation of the results, supervision, funding acquisition, and reviewing and editing. V.B.: conceptualization, revision of the histological slides, interpretation of the results, statistical analyses, funding acquisition, and reviewing and editing.
Corresponding author
Ethics declarations
Ethics approval
Comitato Etico per la Sperimentazione Clinica delle province di Verona e Rovigo (protocol n. 11335, 2019/02/26.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Aldo Scarpa and Valeria Barresi shared last authorship.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ammendola, S., Caldonazzi, N., Simbolo, M. et al. H3K27me3 immunostaining is diagnostic and prognostic in diffuse gliomas with oligodendroglial or mixed oligoastrocytic morphology. Virchows Arch 479, 987–996 (2021). https://doi.org/10.1007/s00428-021-03134-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-021-03134-1