Abstract
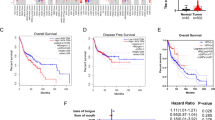
An HPV infection is involved in the etiology of about 25 % of head and neck squamous cell carcinomas (HNSCC). It has been postulated that a strong antitumoral immune response in HPV-positive tumors represents an important underlying mechanism for their good response to therapy. Recently, the Warburg phenomenon has returned to the center of attention because it affects antitumoral immune response and response to therapy. Accumulation of tumor cell-derived lactate inhibits cytotoxic T cells, as these, analogous to cancer cells, depend on glycolysis and lactate secretion for fulfillment of energy needs. Sparse information exists on the Warburg effect in HNSCC. This study aimed to characterize the metabolic and immunological features of HPV-negative and HPV-positive HNSCC. An immunohistochemical analysis of oropharyngeal carcinomas showed an enhanced antitumoral immune response (CD8/CD4 ratio) together with increased levels of proteins involved in transmembranous metabolite transportation (GLUT1 and CD147) and respiratory metabolism (COX5B) in HPV-positive tumors as compared to HPV-negative tumors. mRNA and Western blot analyses of an HPV-positive and HPV-negative HNSCC cell line revealed metabolic characteristics similar to the in vivo situation. Additionally, the HPV-negative cell line showed stronger extracellular lactate accumulation. In contrast, the HPV-positive cell line presented with better adaption to lactic acidosis suggesting an ability to metabolize lactate. Our results indicate that HPV-positive and HPV-negative carcinomas do not only differ in terms of tumor immune microenvironment, but also in terms of tumor metabolism, characterized by an increased glucose and respiratory metabolism together with decreased lactate accumulation in HPV-positive HNSCC. Therefore, targeting metabolic pathways could represent a promising adjunct in the therapy of HPV-positive HNSCC.





Similar content being viewed by others
References
Adelstein DJ, Ridge JA, Gillison ML, Chaturvedi AK, D'Souza G, Gravitt PE, Westra W, Psyrri A, Kast WM, Koutsky LA, Giuliano A, Krosnick S, Trotti A, Schuller DE, Forastiere A, Ullmann CD (2009) Head and neck squamous cell cancer and the human papillomavirus: summary of a National Cancer Institute State of the Science Meeting, November 9–10, 2008, Washington, D.C. Head Neck 31(11):1393–1422. doi:10.1002/hed.21269
Gillison ML, D'Souza G, Westra W, Sugar E, Xiao W, Begum S, Viscidi R (2008) Distinct risk factor profiles for human papillomavirus type 16-positive and human papillomavirus type 16-negative head and neck cancers. J Natl Cancer Inst 100(6):407–420. doi:10.1093/jnci/djn025
Kreimer AR, Clifford GM, Boyle P, Franceschi S (2005) Human papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic review. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology 14 (2):467-475. doi:10.1158/1055-9965.EPI-04-0551
Termine N, Panzarella V, Falaschini S, Russo A, Matranga D, Lo Muzio L, Campisi G (2008) HPV in oral squamous cell carcinoma vs head and neck squamous cell carcinoma biopsies: a meta-analysis (1988–2007). Ann Oncol Off J Eur Soc Med Oncol / ESMO 19(10):1681–1690. doi:10.1093/annonc/mdn372
Hammarstedt L, Lindquist D, Dahlstrand H, Romanitan M, Dahlgren LO, Joneberg J, Creson N, Lindholm J, Ye W, Dalianis T, Munck-Wikland E (2006) Human papillomavirus as a risk factor for the increase in incidence of tonsillar cancer. Int J Cancer J Int du Cancer 119(11):2620–2623. doi:10.1002/ijc.22177
Nasman A, Attner P, Hammarstedt L, Du J, Eriksson M, Giraud G, Ahrlund-Richter S, Marklund L, Romanitan M, Lindquist D, Ramqvist T, Lindholm J, Sparen P, Ye W, Dahlstrand H, Munck-Wikland E, Dalianis T (2009) Incidence of human papillomavirus (HPV) positive tonsillar carcinoma in Stockholm, Sweden: an epidemic of viral-induced carcinoma? Int J Cancer J Int du Cancer 125(2):362–366. doi:10.1002/ijc.24339
Rotnaglova E, Tachezy R, Salakova M, Prochazka B, Kosl'abova E, Vesela E, Ludvikova V, Hamsikova E, Klozar J (2011) HPV involvement in tonsillar cancer: prognostic significance and clinically relevant markers. Int J Cancer J Int du Cancer 129(1):101–110. doi:10.1002/ijc.25889
O'Rorke MA, Ellison MV, Murray LJ, Moran M, James J, Anderson LA (2012) Human papillomavirus related head and neck cancer survival: a systematic review and meta-analysis. Oral Oncol 48(12):1191–1201. doi:10.1016/j.oraloncology.2012.06.019
Fakhry C, Westra WH, Li S, Cmelak A, Ridge JA, Pinto H, Forastiere A, Gillison ML (2008) Improved survival of patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial. J Natl Cancer Inst 100(4):261–269. doi:10.1093/jnci/djn011
Syrjanen S (2010) The role of human papillomavirus infection in head and neck cancers. Ann Oncol Off J Eur Soc Med Oncol / ESMO 21(Suppl 7):vii243–vii245. doi:10.1093/annonc/mdq454
Lewis JS Jr, Chernock RD (2014) Human papillomavirus and Epstein Barr virus in head and neck carcinomas: suggestions for the new WHO classification. Head Neck Pathol 8(1):50–58. doi:10.1007/s12105-014-0528-6
Smith EM, Rubenstein LM, Haugen TH, Pawlita M, Turek LP (2012) Complex etiology underlies risk and survival in head and neck cancer human papillomavirus, tobacco, and alcohol: a case for multifactor disease. J Oncol 2012:571862. doi:10.1155/2012/571862
Isayeva T, Li Y, Maswahu D, Brandwein-Gensler M (2012) Human papillomavirus in non-oropharyngeal head and neck cancers: a systematic literature review. Head Neck Pathol 6(Suppl 1):S104–S120. doi:10.1007/s12105-012-0368-1
Kong CS, Narasimhan B, Cao H, Kwok S, Erickson JP, Koong A, Pourmand N, Le QT (2009) The relationship between human papillomavirus status and other molecular prognostic markers in head and neck squamous cell carcinomas. Int J Radiat Oncol Biol Phys 74(2):553–561. doi:10.1016/j.ijrobp.2009.02.015
Nasman A, Romanitan M, Nordfors C, Grun N, Johansson H, Hammarstedt L, Marklund L, Munck-Wikland E, Dalianis T, Ramqvist T (2012) Tumor infiltrating CD8+ and Foxp3+ lymphocytes correlate to clinical outcome and human papillomavirus (HPV) status in tonsillar cancer. PLoS ONE 7(6):e38711. doi:10.1371/journal.pone.0038711
Russell SMAT, Lechner MG, Liebertz DJ, Correa AJ, Sinja IK, Kokot N, Epstein AL (2013) Immune cell infiltration patterns and survival in head and neck squamous cell carcinoma. Head Neck Oncol 5(11):10
Gottfried E, Kreutz M, Mackensen A (2012) Tumor metabolism as modulator of immune response and tumor progression. Semin Cancer Biol 22(4):335–341. doi:10.1016/j.semcancer.2012.02.009
Warburg O, Wind F, Negelein E (1927) The metabolism of tumors in the body. J Gen Physiol 8(6):519–530
Walenta S, Wetterling M, Lehrke M, Schwickert G, Sundfor K, Rofstad EK, Mueller-Klieser W (2000) High lactate levels predict likelihood of metastases, tumor recurrence, and restricted patient survival in human cervical cancers. Cancer Res 60(4):916–921
Walenta S, Salameh A, Lyng H, Evensen JF, Mitze M, Rofstad EK, Mueller-Klieser W (1997) Correlation of high lactate levels in head and neck tumors with incidence of metastasis. Am J Pathol 150(2):409–415
Sattler UG, Meyer SS, Quennet V, Hoerner C, Knoerzer H, Fabian C, Yaromina A, Zips D, Walenta S, Baumann M, Mueller-Klieser W (2010) Glycolytic metabolism and tumour response to fractionated irradiation. Radiother Oncol J Eur Soc Ther Radiol Oncol 94(1):102–109. doi:10.1016/j.radonc.2009.11.007
Quennet V, Yaromina A, Zips D, Rosner A, Walenta S, Baumann M, Mueller-Klieser W (2006) Tumor lactate content predicts for response to fractionated irradiation of human squamous cell carcinomas in nude mice. Radiother Oncol J Eur Soc Ther Radiol Oncol 81(2):130–135. doi:10.1016/j.radonc.2006.08.012
Fischer K, Hoffmann P, Voelkl S, Meidenbauer N, Ammer J, Edinger M, Gottfried E, Schwarz S, Rothe G, Hoves S, Renner K, Timischl B, Mackensen A, Kunz-Schughart L, Andreesen R, Krause SW, Kreutz M (2007) Inhibitory effect of tumor cell-derived lactic acid on human T cells. Blood 109(9):3812–3819. doi:10.1182/blood-2006-07-035972
Mendler AN, Hu B, Prinz PU, Kreutz M, Gottfried E, Noessner E (2012) Tumor lactic acidosis suppresses CTL function by inhibition of p38 and JNK/c-Jun activation. Int J Cancer J Int du Cancer 131(3):633–640. doi:10.1002/ijc.26410
Halestrap AP, Wilson MC (2012) The monocarboxylate transporter family–role and regulation. IUBMB Life 64(2):109–119. doi:10.1002/iub.572
Nijtmans LG, Taanman JW, Muijsers AO, Speijer D, Van den Bogert C (1998) Assembly of cytochrome-c oxidase in cultured human cells. Eur J Biochem / FEBS 254(2):389–394
Krupar R, Hartl M, Wirsching K, Dietmaier W, Strutz J, Hofstaedter F (2013) Comparison of HPV prevalence in HNSCC patients with regard to regional and socioeconomic factors. Eur Arch Otorhinolaryngol. doi:10.1007/s00405-013-2693-8
Sotlar K, Diemer D, Dethleffs A, Hack Y, Stubner A, Vollmer N, Menton S, Menton M, Dietz K, Wallwiener D, Kandolf R, Bultmann B (2004) Detection and typing of human papillomavirus by e6 nested multiplex PCR. J Clin Microbiol 42(7):3176–3184. doi:10.1128/JCM.42.7.3176-3184.2004
Simon R, Mirlacher M, Sauter G (2004) Tissue microarrays. Methods Mol Med 97:377–389. doi:10.1385/1-59259-760-2:377
Schiffner S, Zimara N, Schmid R, Bosserhoff AK (2011) p54nrb is a new regulator of progression of malignant melanoma. Carcinogenesis 32(8):1176–1182. doi:10.1093/carcin/bgr103
Canady J, Arndt S, Karrer S, Bosserhoff AK (2013) Increased KGF expression promotes fibroblast activation in a double paracrine manner resulting in cutaneous fibrosis. J Invest Dermatol 133(3):647–657. doi:10.1038/jid.2012.389
Rheinwald JG, Beckett MA (1981) Tumorigenic keratinocyte lines requiring anchorage and fibroblast support cultured from human squamous cell carcinomas. Cancer Res 41(5):1657–1663
Min BM, Baek JH, Shin KH, Gujuluva CN, Cherrick HM, Park NH (1994) Inactivation of the p53 gene by either mutation or HPV infection is extremely frequent in human oral squamous cell carcinoma cell lines. Eur J Cancer B Oral Oncol 30B(5):338–345
Lee JK, Kim MJ, Hong SP, Hong SD (2004) Inactivation patterns of p16/INK4A in oral squamous cell carcinomas. Exp Mol Med 36(2):165–171. doi:10.1038/emm.2004.23
Hoffmann TK, Sonkoly E, Hauser U, van Lierop A, Whiteside TL, Klussmann JP, Hafner D, Schuler P, Friebe-Hoffmann U, Scheckenbach K, Erjala K, Grenman R, Schipper J, Bier H, Balz V (2008) Alterations in the p53 pathway and their association with radio- and chemosensitivity in head and neck squamous cell carcinoma. Oral Oncol 44(12):1100–1109. doi:10.1016/j.oraloncology.2008.02.006
Bosserhoff AK, Ellmann L, Kuphal S (2011) Melanoblasts in culture as an in vitro system to determine molecular changes in melanoma. Exp Dermatol 20(5):435–440. doi:10.1111/j.1600-0625.2011.01271.x
Arndt S, Schmidt J, Wacker E, Karrer S, Bosserhoff AK (2011) Fussel-15, a new player in wound healing, is deregulated in keloid and localized scleroderma. Am J Pathol 178(6):2622–2631. doi:10.1016/j.ajpath.2011.02.009
Fox CJ, Hammerman PS, Thompson CB (2005) Fuel feeds function: energy metabolism and the T-cell response. Nat Rev Immunol 5(11):844–852. doi:10.1038/nri1710
Feder-Mengus C, Ghosh S, Weber WP, Wyler S, Zajac P, Terracciano L, Oertli D, Heberer M, Martin I, Spagnoli GC, Reschner A (2007) Multiple mechanisms underlie defective recognition of melanoma cells cultured in three-dimensional architectures by antigen-specific cytotoxic T lymphocytes. Br J Cancer 96(7):1072–1082. doi:10.1038/sj.bjc.6603664
Wansom D, Light E, Worden F, Prince M, Urba S, Chepeha DB, Cordell K, Eisbruch A, Taylor J, D'Silva N, Moyer J, Bradford CR, Kurnit D, Kumar B, Carey TE, Wolf GT (2010) Correlation of cellular immunity with human papillomavirus 16 status and outcome in patients with advanced oropharyngeal cancer. Arch Otolaryngol Head Neck Surg 136(12):1267–1273. doi:10.1001/archoto.2010.211
Demir L, Yigit S, Ellidokuz H, Erten C, Somali I, Kucukzeybek Y, Alacacioglu A, Cokmert S, Can A, Akyol M, Dirican A, Bayoglu V, Sari AA, Tarhan MO (2013) Predictive and prognostic factors in locally advanced breast cancer: effect of intratumoral FOXP3+ Tregs. Clin Exp Metastasis 30(8):1047–1062. doi:10.1007/s10585-013-9602-9
Huang Y, Wang F, Wang Y, Zhu Z, Gao Y, Ma Z, Xu R, Du Z (2013) Intrahepatic IL-17 T cells and FoxP3 Tregs cooperate to promote development and affect the prognosis of hepatocellular carcinoma. J Gastroenterol Hepatol. doi:10.1111/jgh.12418
Wang L, Yi T, Kortylewski M, Pardoll DM, Zeng D, Yu H (2009) IL-17 can promote tumor growth through an IL-6-Stat3 signaling pathway. J Exp Med 206(7):1457–1464. doi:10.1084/jem.20090207
Numasaki M, Fukushi J, Ono M, Narula SK, Zavodny PJ, Kudo T, Robbins PD, Tahara H, Lotze MT (2003) Interleukin-17 promotes angiogenesis and tumor growth. Blood 101(7):2620–2627. doi:10.1182/blood-2002-05-1461
Chen WC, Lai YH, Chen HY, Guo HR, Su IJ, Chen HH (2013) Interleukin-17-producing cell infiltration in the breast cancer tumour microenvironment is a poor prognostic factor. Histopathology 63(2):225–233. doi:10.1111/his.12156
Tosolini M, Kirilovsky A, Mlecnik B, Fredriksen T, Mauger S, Bindea G, Berger A, Bruneval P, Fridman WH, Pages F, Galon J (2011) Clinical impact of different classes of infiltrating T cytotoxic and helper cells (Th1, th2, treg, th17) in patients with colorectal cancer. Cancer Res 71(4):1263–1271. doi:10.1158/0008-5472.CAN-10-2907
Yabu M, Shime H, Hara H, Saito T, Matsumoto M, Seya T, Akazawa T, Inoue N (2011) IL-23-dependent and -independent enhancement pathways of IL-17A production by lactic acid. Int Immunol 23(1):29–41. doi:10.1093/intimm/dxq455
Michalek RD, Gerriets VA, Jacobs SR, Macintyre AN, MacIver NJ, Mason EF, Sullivan SA, Nichols AG, Rathmell JC (2011) Cutting edge: distinct glycolytic and lipid oxidative metabolic programs are essential for effector and regulatory CD4+ T cell subsets. J Immunol 186(6):3299–3303. doi:10.4049/jimmunol.1003613
Rademakers SE, Lok J, van der Kogel AJ, Bussink J, Kaanders JH (2011) Metabolic markers in relation to hypoxia; staining patterns and colocalization of pimonidazole, HIF-1alpha, CAIX, LDH-5, GLUT-1, MCT1 and MCT4. BMC Cancer 11:167. doi:10.1186/1471-2407-11-167
Rieckmann T, Tribius S, Grob TJ, Meyer F, Busch CJ, Petersen C, Dikomey E, Kriegs M (2013) HNSCC cell lines positive for HPV and p16 possess higher cellular radiosensitivity due to an impaired DSB repair capacity. Radiother Oncol J Eur Soc Ther Radiol Oncol 107(2):242–246. doi:10.1016/j.radonc.2013.03.013
Hauser U, Balz V, Carey TE, Grenman R, Van Lierop A, Scheckenbach K, Bier H (2002) Reliable detection of p53 aberrations in squamous cell carcinomas of the head and neck requires transcript analysis of the entire coding region. Head Neck 24(9):868–873. doi:10.1002/hed.10128
St John LS, Sauter ER, Herlyn M, Litwin S, Adler-Storthz K (2000) Endogenous p53 gene status predicts the response of human squamous cell carcinomas to wild-type p53. Cancer Gene Ther 7(5):749–756. doi:10.1038/sj.cgt.7700166
Weichselbaum RR, Dahlberg W, Beckett M, Karrison T, Miller D, Clark J, Ervin TJ (1986) Radiation-resistant and repair-proficient human tumor cells may be associated with radiotherapy failure in head- and neck-cancer patients. Proc Natl Acad Sci USA 83(8):2684–2688
Curry JM, Tuluc M, Whitaker-Menezes D, Ames JA, Anantharaman A, Butera A, Leiby B, Cognetti DM, Sotgia F, Lisanti MP, Martinez-Outschoorn UE (2013) Cancer metabolism, stemness and tumor recurrence: MCT1 and MCT4 are functional biomarkers of metabolic symbiosis in head and neck cancer. Cell Cycle 12(9):1371–1384. doi:10.4161/cc.24092
Sonveaux P, Vegran F, Schroeder T, Wergin MC, Verrax J, Rabbani ZN, De Saedeleer CJ, Kennedy KM, Diepart C, Jordan BF, Kelley MJ, Gallez B, Wahl ML, Feron O, Dewhirst MW (2008) Targeting lactate-fueled respiration selectively kills hypoxic tumor cells in mice. J Clin Invest 118(12):3930–3942. doi:10.1172/JCI36843
Sawayama H, Ishimoto T, Watanabe M, Yoshida N, Baba Y, Sugihara H, Izumi D, Kurashige J, Baba H (2013) High expression of glucose transporter 1 on primary lesions of esophageal squamous cell carcinoma is associated with hematogenous recurrence. Ann Surg Oncol. doi:10.1245/s10434-013-3371-1
Singer K, Kastenberger M, Gottfried E, Hammerschmied CG, Buttner M, Aigner M, Seliger B, Walter B, Schlosser H, Hartmann A, Andreesen R, Mackensen A, Kreutz M (2011) Warburg phenotype in renal cell carcinoma: high expression of glucose-transporter 1 (GLUT-1) correlates with low CD8(+) T-cell infiltration in the tumor. Int J Cancer J Int du Cancer 128(9):2085–2095. doi:10.1002/ijc.25543
Lechner M, Frampton GM, Fenton T, Feber A, Palmer G, Jay A, Pillay N, Forster M, Cronin MT, Lipson D, Miller VA, Brennan TA, Henderson S, Vaz F, O'Flynn P, Kalavrezos N, Yelensky R, Beck S, Stephens PJ, Boshoff C (2013) Targeted next-generation sequencing of head and neck squamous cell carcinoma identifies novel genetic alterations in HPV + and HPV- tumors. Genome Med 5(5):49. doi:10.1186/gm453
Gaykalova DA, Mambo E, Choudhary A, Houghton J, Buddavarapu K, Sanford T, Darden W, Adai A, Hadd A, Latham G, Danilova LV, Bishop J, Li RJ, Westra WH, Hennessey P, Koch WM, Ochs MF, Califano JA, Sun W (2014) Novel insight into mutational landscape of head and neck squamous cell carcinoma. PLoS ONE 9(3):e93102. doi:10.1371/journal.pone.0093102
Acknowledgments
This work was supported by funding from the German Research Foundation (KFO262) and a grant from the Foundation Tumor Research Head and Neck (Stiftung Tumorforschung Kopf Hals). The cell line UD-SCC-2 was a generous gift from Prof. Thomas Hoffmann.
Conflict of interest
None to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krupar, R., Robold, K., Gaag, D. et al. Immunologic and metabolic characteristics of HPV-negative and HPV-positive head and neck squamous cell carcinomas are strikingly different. Virchows Arch 465, 299–312 (2014). https://doi.org/10.1007/s00428-014-1630-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-014-1630-6