Abstract
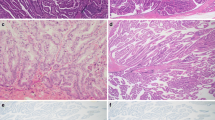
A tumorigenic role of peribiliary glands (PBGs) has been suggested recently. This study was performed to clarify the histological characteristics of PBGs showing cystic and micropapillary epithelial changes. From histological sections of a total of 938 autopsy livers, cases with cystic and micropapillary changes of the epithelial cells of intrahepatic PBGs were collected. PBGs with cystic change that lacked micropapillary epithelial changes were referred to as cystic lesion. Mucin staining and immunohistochemical analysis were performed, and the results were compared between cystic and micropapillary (C-P) lesions and cystic lesions. C-P and cystic lesions were observed in 9 (1 %) and 40 (4 %) , respectively. The atypia of micropapillary epithelium was usually mild, but in a single case, invasive adenocarcinoma accompanied a C-P lesion. Abundant mucin expression was observed in all cases of C-P lesion, which was similar to mucinous acini of normal PBGs rather than serous acini. Immunohistochemical analysis showed that MUC5AC was more frequently expressed in C-P lesions than in cystic lesions. Immunohistochemical expression of cyclin D1 and S100P was characteristically found in C-P lesions. Mean Ki-67 labeling index of C-P lesions was significantly higher than that of cystic lesions. The immunoprofile of C-P lesions was similar to that of the branch-type intraductal papillary mucinous neoplasm of the pancreas. These results suggest that C-P lesions may have neoplastic features and might represent a precursor of biliary epithelial neoplasms, including branch-type intraductal papillary neoplasm of the bile duct as well as mucin-producing cholangiocarcinoma, a concept that we have recently proposed.




Similar content being viewed by others

Abbreviations
- BilIN:
-
biliary intraepithelial neoplasia
- CEA:
-
carcinogenic embryonic antigen
- C-P:
-
cystic and micropapillary
- H&E:
-
hematoxylin and eosin
- IPMN:
-
intraductal papillary mucinous neoplasm
- IPNB:
-
intraductal papillary neoplasm of the bile duct
- PanIN:
-
pancreatic intraepithelial neoplasia
- PBG:
-
peribiliary gland
References
Nakanuma Y, Katayanagi K, Terada T et al (1994) Intrahepatic peribiliary glands of humans. I. Anatomy, development and presumed functions. J Gastroenterol Hepatol 9:75–79
Nakanuma Y, Hoso M, Sanzen T et al (1997) Microstructure and development of the normal and pathologic biliary tract in humans, including blood supply. Microsc Res Tech 38:552–570
Terada T, Nakanuma Y (1990) Pathological observations of intrahepatic peribiliary glands in 1000 consecutive autopsy livers. III. Survey of necroinflammation and cystic dilatation. Hepatology 12:1229–1233
Terada T, Nakanuma Y (1992) Pathologic observations of intrahepatic peribiliary glands in 1,000 consecutive autopsy livers: IV. Hyperplasia of intramural and extramural glands. Hum Pathol 23:483–490
Terada T, Nakanuma Y (1990) Pathological observations of intrahepatic peribiliary glands in 1,000 consecutive autopsy livers. II. A possible source of cholangiocarcinoma. Hepatology 12:92–97
Nakanuma Y, Sasaki M, Terada T et al (1994) Intrahepatic peribiliary glands of humans. II. Pathological spectrum. J Gastroenterol Hepatol 9:80–86
Carpino G, Cardinale V, Onori P et al (2012) Biliary tree stem/progenitor cells in glands of extrahepatic and intraheptic bile ducts: an anatomical in situ study yielding evidence of maturational lineages. J Anat 220:186–199
Cardinale V, Wang Y, Carpino G et al (2012) The biliary tree—a reservoir of multipotent stem cells. Nat Rev Gastroenterol Hepatol 9:231–240
Sutton ME, Op den Dries S, Koster MH et al (2012) Regeneration of human extrahepatic biliary epithelium: the peribiliary glands as progenitor cell compartment. Liver Int 32:554–559
Cardinale V, Wang Y, Carpino G et al (2012) Mucin-producing cholangiocarcinoma might derive from biliary tree stem/progenitor cells located in peribiliary glands. Hepatology 55:2041–2042
Somer L, Andrejić B, Milošević P (2012) Origin and pathological characteristics of Klatskin tumor: a case report and literature review. Pol J Pathol 63:65–70
Terada T, Sasaki M, Nakanuma Y et al (1992) Hilar cholangiocarcinoma (Klatskin tumor) arising from intrahepatic peribiliary glands. J Clin Gastroenterol 15:79–81
Nakanuma Y, Sasaki M, Sato Y et al (2009) Multistep carcinogenesis of perihilar cholangiocarcinoma arising in the intrahepatic large bile ducts. World J Hepatol 1:35–42
Nakanuma Y, Sato Y (2012) Cystic and papillary neoplasm involving peribiliary glands: a biliary counterpart of branch-type intraductal papillary mucinous neoplasm? Hepatology 55:2040–2041
Zen Y, Sasaki M, Fujii T et al (2006) Different expression patterns of mucin core proteins and cytokeratins during intrahepatic cholangiocarcinogenesis from biliary intraepithelial neoplasia and intraductal papillary neoplasm of the bile duct--an immunohistochemical study of 110 cases of hepatolithiasi. J Hepatol 44:350–358
Nakanishi Y, Zen Y, Kondo S et al (2008) Expression of cell cycle-related molecules in biliary premalignant lesions: biliary intraepithelial neoplasia and biliary intraductal papillary neoplasm. Hum Pathol 39:1153–1161
Aishima S, Fujita N, Mano Y et al (2011) Different roles of S100P overexpression in intrahepatic cholangiocarcinoma: carcinogenesis of perihilar type and aggressive behavior of peripheral type. Am J Surg Pathol 35:590–598
Nakanishi Y, Zen Y, Hirano S et al (2009) Intraductal oncocytic papillary neoplasm of the bile duct: the first case of peribiliary gland origin. J Hepatobiliary Pancreat Surg 16:869–873
Nakanishi Y, Nakanuma Y, Ohara M et al (2011) Intraductal papillary neoplasm arising from peribiliary glands connecting with the inferior branch of the bile duct of the anterior segment of the liver. Pathol Int 61:773–777
Adsay NV, Fukushima N, Furukawa T et al (2010) Intraductal neoplasms of the pancreas. In: Bosman FT, Carneiro F, Hruban RH, Theise ND (eds) WHO classification of tumors of the digestive system; World Health Organization of Tumors, 4th edn. IARC, Lyon, pp 304–313
Biankin AV, Kench JG, Biankin SA et al (2004) Pancreatic intraepithelial neoplasia in association with intraductal papillary mucinous neoplasms of the pancreas: implications for disease progression and recurrence. Am J Surg Pathol 28:1184–1192
Nakata K, Nagai E, Ohuchida K et al (2010) S100P is a novel marker to identify intraductal papillary mucinous neoplasms. Hum Pathol 41:824–831
Seguchi T, Akiyama Y, Itoh H et al (2004) Multiple hepatic peribiliary cysts with cirrhosis. J Gastroenterol 39:384–390
Fujioka Y, Kawamura N, Tanaka S et al (1997) Multiple hilar cysts of the liver in patients with alcoholic cirrhosis: report of three cases. J Gastroenterol Hepatol 12:137–143
Matsubara T, Sato Y, Igarashi S et al. (2013) Alcohol-related injury to peribiliary glands is a cause of peribiliary cysts: based on analysis of clinical and autopsy cases. J Clin Gastroenterol
Acknowledgment
This study was supported by Hepatolithiasis Subdivision of Intractable Hepatobiliary Diseases Study Group of Japan (Chairman, Hirohito Tsubouchi; Department of Internal Medicine, Kagoshima University Graduate School of Medicine, Kagoshima, Japan)
Conflict of interest
None of the authors has any conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sato, Y., Harada, K., Sasaki, M. et al. Cystic and micropapillary epithelial changes of peribiliary glands might represent a precursor lesion of biliary epithelial neoplasms. Virchows Arch 464, 157–163 (2014). https://doi.org/10.1007/s00428-014-1537-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-014-1537-2