Abstract
Purpose
Minimally invasive surgery has increasingly gained popularity as a treatment of choice for pancreatectomy with encouraging initial results in robotic distal pancreatectomy (RDP). However, few data are available on the comparison between RDP and laparoscopic distal pancreatectomy (LDP) for pancreatic neuroendocrine tumors (pNETs). Our aim, thus, is to compare perioperative and long-term outcomes as well as total costs of RDP and LDP for pNETs.
Methods
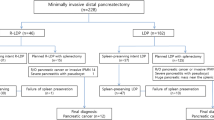
All RDPs and LDPs for pNETs performed in four referral centers from 2008 to 2016 were included. Perioperative outcomes, histopathological results, overall (OS) and disease-free survival (DFS), and total costs were evaluated.
Results
Ninety-six RDPs and 85 LDPs were included. Demographic and clinical characteristics were comparable between the two cohorts. Operative time was 36.5 min longer in the RDP group (p = 0.009) but comparable to LDP after removing the docking time (247.9 vs 233.7 min; p = 0.6). LDP related to a lower spleen preservation rate (44.7% vs 65.3%; p < 0.0001) and higher blood loss (239.7 ± 112 vs 162.5 ± 98 cc; p < 0.0001). Advantages in operative time for RDP were documented in case of the spleen preservation procedures (265 ± 41.52 vs 291 ± 23 min; p = 0.04). Conversion rate, postoperative morbidity, and pancreatic fistula rate were similar between the two groups, as well as histopathological data, OS, and DFS. Significant advantages were evidenced for LDP regarding mean total costs (9235 (± 1935) € vs 11,226 (± 2365) €; p < 0.0001).
Conclusions
Both RDP and LDP are safe and efficacious for pNETs treatment. However, RDP offers advantages with a higher spleen preservation rate and lower blood loss. Costs still remain the main limitation of the robotic approach.


Similar content being viewed by others
References
Hill JS, McPhee JT, McDade TP, Zhou Z, Sullivan ME, Whalen GF, Tseng JF (2009) Pancreatic neuroendocrine tumors: the impact of surgical resection on survival. Cancer 115(4):741–751. https://doi.org/10.1002/cncr.24065
Gagner M, Pomp A, Herrera MF (1996) Early experience with laparoscopic resections of islet cell tumors. Surgery 120(6):1051–1054
Antonakis PT, Ashrafian H, Martinez-Isla A (2015) Pancreatic insulinomas: laparoscopic management. World J Gastrointest Endosc 7(16):1197–1207. https://doi.org/10.4253/wjge.v7.i16.1197
Fernandez-Cruz L, Martinez I, Gilabert R, Cesar-Borges G, Astudillo E, Navarro S (2004) Laparoscopic distal pancreatectomy combined with preservation of the spleen for cystic neoplasms of the pancreas. J Gastrointest Surg 8(4):493–501. https://doi.org/10.1016/j.gassur.2003.11.014
Liu H, Peng C, Zhang S, Wu Y, Fang H, Sheng H, Peng S (2007) Strategy for the surgical management of insulinomas: analysis of 52 cases. Dig Surg 24(6):463–470. https://doi.org/10.1159/000111822
Sa Cunha A, Beau C, Rault A, Catargi B, Collet D, Masson B (2007) Laparoscopic versus open approach for solitary insulinoma. Surg Endosc 21(1):103–108. https://doi.org/10.1007/s00464-006-0021-8
Fernandez Ranvier GG, Shouhed D, Inabnet WB 3rd (2016) Minimally invasive techniques for resection of pancreatic Neuroendocrine tumors. Surg Oncol Clin N Am 25(1):195–215. https://doi.org/10.1016/j.soc.2015.08.009
Melvin WS, Needleman BJ, Krause KR, Schneider C, Wolf RK, Michler RE, Ellison EC (2002) Computer-enhanced robotic telesurgery. Initial experience in foregut surgery. Surg Endosc 16(12):1790–1792. https://doi.org/10.1007/s00464-001-8192-9
Daouadi M, Zureikat AH, Zenati MS, Choudry H, Tsung A, Bartlett DL, Hughes SJ, Lee KK, Moser AJ, Zeh HJ (2013) Robot-assisted minimally invasive distal pancreatectomy is superior to the laparoscopic technique. Ann Surg 257(1):128–132. https://doi.org/10.1097/SLA.0b013e31825fff08
Chen S, Zhan Q, Chen JZ, Jin JB, Deng XX, Chen H, Shen BY, Peng CH, Li HW (2015) Robotic approach improves spleen-preserving rate and shortens postoperative hospital stay of laparoscopic distal pancreatectomy: a matched cohort study. Surg Endosc 29(12):3507–3518. https://doi.org/10.1007/s00464-015-4101-5
Giulianotti PC, Sbrana F, Bianco FM, Elli EF, Shah G, Addeo P, Caravaglios G, Coratti A (2010) Robot-assisted laparoscopic pancreatic surgery: single-surgeon experience. Surg Endosc 24(7):1646–1657. https://doi.org/10.1007/s00464-009-0825-4
Kang CM, Kim DH, Lee WJ, Chi HS (2011) Conventional laparoscopic and robot-assisted spleen-preserving pancreatectomy: does da Vinci have clinical advantages? Surg Endosc 25(6):2004–2009. https://doi.org/10.1007/s00464-010-1504-1
Lai EC, Tang CN (2013) Current status of robot-assisted laparoscopic pancreaticoduodenectomy and distal pancreatectomy: a comprehensive review. Asian J Endosc Surg 6(3):158–164. https://doi.org/10.1111/ases.12040
Lee SY, Allen PJ, Sadot E, D'Angelica MI, DeMatteo RP, Fong Y, Jarnagin WR, Kingham TP (2015) Distal pancreatectomy: a single institution's experience in open, laparoscopic, and robotic approaches. J Am Coll Surg 220(1):18–27. https://doi.org/10.1016/j.jamcollsurg.2014.10.004
Waters JA, Canal DF, Wiebke EA, Dumas RP, Beane JD, Aguilar-Saavedra JR, Ball CG, House MG, Zyromski NJ, Nakeeb A, Pitt HA, Lillemoe KD, Schmidt CM (2010) Robotic distal pancreatectomy: cost effective? Surgery 148(4):814–823. https://doi.org/10.1016/j.surg.2010.07.027
Zureikat AH, Moser AJ, Boone BA, Bartlett DL, Zenati M, Zeh HJ 3rd (2013) 250 robotic pancreatic resections: safety and feasibility. Ann Surg 258(4):554–559; discussion 559-562. https://doi.org/10.1097/SLA.0b013e3182a4e87c
Melvin WS, Needleman BJ, Krause KR, Ellison EC (2003) Robotic resection of pancreatic neuroendocrine tumor. J Laparoendosc Adv Surg Tech A 13(1):33–36. https://doi.org/10.1089/109264203321235449
Falconi M, Plockinger U, Kwekkeboom DJ, Manfredi R, Korner M, Kvols L, Pape UF, Ricke J, Goretzki PE, Wildi S, Steinmuller T, Oberg K, Scoazec JY, Frascati Consensus C, European Neuroendocrine Tumor S (2006) Well-differentiated pancreatic nonfunctioning tumors/carcinoma. Neuroendocrinology 84(3):196–211. https://doi.org/10.1159/000098012
Falconi M, Bartsch DK, Eriksson B, Kloppel G, Lopes JM, O'Connor JM, Salazar R, Taal BG, Vullierme MP, O'Toole D, Conference p BC (2012) ENETS Consensus guidelines for the management of patients with digestive neuroendocrine neoplasms of the digestive system: well-differentiated pancreatic non-functioning tumors. Neuroendocrinology 95(2):120–134. https://doi.org/10.1159/000335587
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M, International Study Group on Pancreatic Fistula D (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138(1):8–13. https://doi.org/10.1016/j.surg.2005.05.001
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Buchler MW (2007) Postpancreatectomy hemorrhage (PPH): an international study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142(1):20–25. https://doi.org/10.1016/j.surg.2007.02.001
Bosman FTCF, Hruban RH (2010) WHO classification of tumours of the digestive system. International Agency for Research on Cancer (IARC), Lyon
Kloppel G, Rindi G, Perren A, Komminoth P, Klimstra DS (2010) The ENETS and AJCC/UICC TNM classifications of the neuroendocrine tumors of the gastrointestinal tract and the pancreas: a statement. Virchows Arch 456(6):595–597. https://doi.org/10.1007/s00428-010-0924-6
Ayav A, Bresler L, Brunaud L, Boissel P, Sfcl, Afce (2005) Laparoscopic approach for solitary insulinoma: a multicentre study. Langenbeck's Arch Surg 390(2):134–140. https://doi.org/10.1007/s00423-004-0526-3
Kim SC, Park KT, Hwang JW, Shin HC, Lee SS, Seo DW, Lee SK, Kim MH, Han DJ (2008) Comparative analysis of clinical outcomes for laparoscopic distal pancreatic resection and open distal pancreatic resection at a single institution. Surg Endosc 22(10):2261–2268. https://doi.org/10.1007/s00464-008-9973-1
Warshaw AL (1988) Conservation of the spleen with distal pancreatectomy. Arch Surg 123(5):550–553
Shoup M, Brennan MF, McWhite K, Leung DH, Klimstra D, Conlon KC (2002) The value of splenic preservation with distal pancreatectomy. Arch Surg 137(2):164–168
Baldwin KM, Katz SC, Espat NJ, Somasundar P (2011) Laparoscopic spleen-preserving distal pancreatectomy in elderly subjects: splenic vessel sacrifice may be associated with a higher rate of splenic infarction. HPB (Oxford) 13(9):621–625. https://doi.org/10.1111/j.1477-2574.2011.00341.x
Melotti G, Butturini G, Piccoli M, Casetti L, Bassi C, Mullineris B, Lazzaretti MG, Pederzoli P (2007) Laparoscopic distal pancreatectomy: results on a consecutive series of 58 patients. Ann Surg 246(1):77–82. https://doi.org/10.1097/01.sla.0000258607.17194.2b
Zhou W, Lv R, Wang X, Mou Y, Cai X, Herr I (2010) Stapler vs suture closure of pancreatic remnant after distal pancreatectomy: a meta-analysis. Am J Surg 200(4):529–536. https://doi.org/10.1016/j.amjsurg.2009.12.022
Tamburrino D, Partelli S, Renzi C, Crippa S, Muffatti F, Perali C, Parisi A, Randolph J, Fusai GK, Cirocchi R, Falconi M (2017) Systematic review and meta-analysis on laparoscopic pancreatic resections for neuroendocrine neoplasms (PNENs). Expert Rev Gastroenterol Hepatol 11(1):65–73. https://doi.org/10.1080/17474124.2017.1253473
Strijker M, van Santvoort HC, Besselink MG, van Hillegersberg R, Borel Rinkes IH, Vriens MR, Molenaar IQ (2013) Robot-assisted pancreatic surgery: a systematic review of the literature. HPB (Oxford) 15(1):1–10. https://doi.org/10.1111/j.1477-2574.2012.00589.x
Hwang HK, Kang CM, Chung YE, Kim KA, Choi SH, Lee WJ (2013) Robot-assisted spleen-preserving distal pancreatectomy: a single surgeon's experiences and proposal of clinical application. Surg Endosc 27(3):774–781. https://doi.org/10.1007/s00464-012-2551-6
Gumbs AA, Gres P, Madureira F, Gayet B (2008) Laparoscopic vs open resection of pancreatic endocrine neoplasms: single institution's experience over 14 years. Langenbeck's Arch Surg 393(3):391–395. https://doi.org/10.1007/s00423-007-0255-5
Zhou ZQ, Kim SC, Song KB, Park KM, Lee JH, Lee YJ (2014) Laparoscopic spleen-preserving distal pancreatectomy: comparative study of spleen preservation with splenic vessel resection and splenic vessel preservation. World J Surg 38(11):2973–2979. https://doi.org/10.1007/s00268-014-2671-3
Hu M, Zhao G, Luo Y, Liu R (2011) Laparoscopic versus open treatment for benign pancreatic insulinomas: an analysis of 89 cases. Surg Endosc 25(12):3831–3837. https://doi.org/10.1007/s00464-011-1800-4
Haugvik SP, Marangos IP, Rosok BI, Pomianowska E, Gladhaug IP, Mathisen O, Edwin B (2013) Long-term outcome of laparoscopic surgery for pancreatic neuroendocrine tumors. World J Surg 37(3):582–590. https://doi.org/10.1007/s00268-012-1893-5
Qu L, Zhiming Z, Xianglong T, Yuanxing G, Yong X, Rong L, Yee LW (2018) Short-and mid-term outcomes of robotic versus laparoscopic distal pancreatosplenectomy for pancreatic ductal adenocarcinoma: a retrospective propensity score-matched study. Int J Surg 55:81–86
Guerrini GP, Lauretta A, Belluco C, Olivieri M, Forlin M, Basso S, Breda B, Bertola G, Di Benedetto F (2017) Robotic versus laparoscopic distal pancreatectomy: an up-to-date meta-analysis. BMC Surg 17(1):105
Lo CY, Chan WF, Lo CM, Fan ST, Tam PK (2004) Surgical treatment of pancreatic insulinomas in the era of laparoscopy. Surg Endosc 18(2):297–302. https://doi.org/10.1007/s00464-003-8156-3
Butturini G, Damoli I, Crepaz L, Malleo G, Marchegiani G, Daskalaki D, Esposito A, Cingarlini S, Salvia R, Bassi C (2015) A prospective non-randomised single-center study comparing laparoscopic and robotic distal pancreatectomy. Surg Endosc 29(11):3163–3170. https://doi.org/10.1007/s00464-014-4043-3
Magge D, Gooding W, Choudry H, Steve J, Steel J, Zureikat A, Krasinskas A, Daouadi M, Lee KK, Hughes SJ, Zeh HJ 3rd, Moser AJ (2013) Comparative effectiveness of minimally invasive and open distal pancreatectomy for ductal adenocarcinoma. JAMA Surg 148(6):525–531. https://doi.org/10.1001/jamasurg.2013.1673
Han SH, Han IW, Heo JS, Choi SH, Choi DW, Han S, You YH (2017) Laparoscopic versus open distal pancreatectomy for nonfunctioning pancreatic neuroendocrine tumors: a large single-center study. Surg Endosc 32:443–449. https://doi.org/10.1007/s00464-017-5702-y
Xourafas D, Tavakkoli A, Clancy TE, Ashley SW (2015) Distal pancreatic resection for neuroendocrine tumors: is laparoscopic really better than open? J Gastrointest Surg 19(5):831–840. https://doi.org/10.1007/s11605-015-2788-1
Phan GQ, Yeo CJ, Hruban RH, Lillemoe KD, Pitt HA, Cameron JL (1998) Surgical experience with pancreatic and peripancreatic neuroendocrine tumors: review of 125 patients. J Gastrointest Surg 2(5):472–482
Acknowledgments
Authors would like to thank Iana Shutrova for the assistance in proofreading the manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
Study conception and design: SA, GB, UB, AP, and LM. Acquisition of data: FV, ID, GQ, AE, and LL. Analysis and interpretation of data: AP, CF, LP, MR, NDL, and GDF. Drafting of the manuscript: GQ, FR, and RM. Critical revision of the manuscript: SA, GB, GBD, UB, and AP.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alfieri, S., Butturini, G., Boggi, U. et al. Short-term and long-term outcomes after robot-assisted versus laparoscopic distal pancreatectomy for pancreatic neuroendocrine tumors (pNETs): a multicenter comparative study. Langenbecks Arch Surg 404, 459–468 (2019). https://doi.org/10.1007/s00423-019-01786-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-019-01786-x