Abstract
Background and aims
The optimal treatment of patients with malignant colorectal polyps is unsettled. The surgical dilemma following polypectomy is selecting between watchful waiting (WW) and subsequent bowel resection (SBR), but the long-term survival outcomes have not been established yet. This nationwide study compared survival of patients after WW or SBR.
Methods
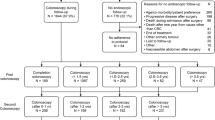
Danish nationwide study with 100% follow-up of all patients with malignant colorectal polyps (the Danish Colorectal Cancer Group database) in a 10-year period from 2001 to 2011. All patients’ charts and histological reports were individually reviewed. Survival rates were calculated with Cox proportional hazard model after propensity score matching.
Results
A total of 692 patients were included (WW, 424 (61.3%), SBR, 268 (38.7%)) with a mean follow-up of 7.5 years (3–188 months). Following propensity score matching, there was no significant difference in overall or disease-free survival (p = 0.344 and p = 0.184) or rate of local recurrence (WW, 7.2%, SBR, 2%, p = 0.052) or distant metastases (WW, 3.3%, SBR, 4.6%, p = 0.77). In the SBR group, there was no residual tumor or lymph node metastases in the resected specimen in 82.5% of the patients.
Conclusion
Subsequent bowel resection may not be superior to endoscopic polypectomy and watchful waiting with regard to overall and disease-free survival in patients with malignant colorectal polyps.




Similar content being viewed by others
Abbreviations
- WW:
-
Watchful waiting
- SBR:
-
Subsequent bowel resection
- TRUS:
-
Transanal endoscopic ultrasound
- MRI:
-
Magnetic resonance imaging
- pT:
-
Pathological T-stage of tumor
- SD:
-
Standard deviation
- ASA-score:
-
American Society of Anesthesiologists’ score
- BMI:
-
Body mass index (kg/m2)
- CCI:
-
Charlson comorbidity index
- OS:
-
Overall survival
- DFS:
-
Disease-free survival
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
J. Ferley, I. Soerjomataram, M. Ervik, GLOBOCAN 2012 v1.0, Cancer incidence and mortality worldwide: IARC CancerBase no. 11. Lyon, France: International Agency for Research on Cancer; 2013. (2013). http://globocan.iarc.fr (accessed April 25, 2017)
Reggiani-Bonetti L, Di Gregorio C, Pedroni M et al (2013) Incidence trend of malignant polyps through the data of a specialized colorectal cancer registry: clinical features and effect of screening. Scand J Gastroenterol 48:1294–1301. https://doi.org/10.3109/00365521.2013.838301
Chantereau MJ, Faivre J, Boutron MC, Piard F, Arveux P, Bedenne L, Hillon P (1992) Epidemiology, management, and prognosis of malignant large bowel polyps within a defined population. Gut 33:259–263 http://www.ncbi.nlm.nih.gov/pubmed/1541423 (accessed May 29, 2017)
N. Wasif, D. Etzioni, M.A. Maggard, J.S. et al. Trends, patterns, and outcomes in the management of malignant colonic polyps in the general population of the United States. Cancer. 117 (2011) 931–7. doi:https://doi.org/10.1002/cncr.25657
Richards CH, Ventham NT, Mansouri D, Wilson M, Ramsay G, Mackay CD, Parnaby CN, Smith D, On J, Speake D, McFarlane G, Neo YN, Aitken E, Forrest C, Knight K, McKay A, Nair H, Mulholland C, Robertson JH, Carey FA, Steele RJC (2016) An evidence-based treatment algorithm for colorectal polyp cancers: results from the Scottish Screen-detected Polyp Cancer Study (SSPoCS). Gut 67:299–306. https://doi.org/10.1136/gutjnl-2016-312201
Cooper GS, Xu F, Barnholtz Sloan JS, Koroukian SM, Schluchter MD (2012) Management of malignant colonic polyps: a population-based analysis of colonoscopic polypectomy versus surgery. Cancer 118:651–659. https://doi.org/10.1002/cncr.26340
Ingeholm P, Gögenür I, Iversen L (2016) Danish colorectal cancer group database. Clin Epidemiol Volume 8:465–468. https://doi.org/10.2147/CLEP.S99481
Haggitt RC, Glotzbach RE, Soffer EE, Wruble LD (1985) Prognostic factors in colorectal carcinomas arising in adenomas: implications for lesions removed by endoscopic polypectomy. Gastroenterology 89:328–336 http://www.ncbi.nlm.nih.gov/pubmed/4007423 (accessed May 29, 2017)
Kikuchi R, Takano M, Takagi K, Fujimoto N, Nozaki R, Fujiyoshi T, Uchida Y (1995) Management of early invasive colorectal cancer. Risk of recurrence and clinical guidelines. Dis Colon Rectum 38:1286–1295 http://www.ncbi.nlm.nih.gov/pubmed/7497841 (accessed June 7, 2017)
M.B. Amin, S.B. Edge. American Joint Committee on Cancer, AJCC cancer staging manual, n.d. http://www.springer.com/br/book/9783319406176 (accessed May 29, 2017)
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213 http://www.ncbi.nlm.nih.gov/pubmed/15273542 (accessed May 29, 2017)
Austin PC (2008) A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat Med 27:2037–2049. https://doi.org/10.1002/sim.3150
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 46:399–424. https://doi.org/10.1080/00273171.2011.568786
Austin PC (2011) Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat 10:150–161. https://doi.org/10.1002/pst.433
Danish Colorectal Cancer Group (DCCG) Annual report (2015), 2015. http://www.dccg.dk/pdf/Aarsrapport_2015.pdf (accessed May 29, 2017)
E.J.A. Morris, E.F. Taylor, J.D.P.Thomas, et al. Thirty-day postoperative mortality after colorectal cancer surgery in England. Gut. 60 (2011) 806–813. doi:https://doi.org/10.1136/gut.2010.232181
Pucciarelli S, Zorzi M, Gennaro N, Gagliardi G, Restivo A, Saugo M, Barina A, Rugge M, Zuin M, Maretto I, Nitti D (2017) In-hospital mortality, 30-day readmission, and length of hospital stay after surgery for primary colorectal cancer: a national population-based study. Eur J Surg Oncol 43:1312–1323. https://doi.org/10.1016/j.ejso.2017.03.003
Schneider EB, Hyder O, Brooke BS, Efron J, Cameron JL, Edil BH, Schulick RD, Choti MA, Wolfgang CL, Pawlik TM (2012) Patient readmission and mortality after colorectal surgery for colon cancer: impact of length of stay relative to other clinical factors. J Am Coll Surg 214:390–398; discussion 398-9. https://doi.org/10.1016/j.jamcollsurg.2011.12.025
Feddern M-L, Jensen TS, Laurberg S (2015) Chronic pain in the pelvic area or lower extremities after rectal cancer treatment and its impact on quality of life. Pain 156:1765–1771. https://doi.org/10.1097/j.pain.0000000000000237
Negoi I, Hostiuc S, Paun S, Negoi RI, Beuran M (2016) Extralevator vs conventional abdominoperineal resection for rectal cancer-a systematic review and meta-analysis. Am J Surg 212:511–526. https://doi.org/10.1016/j.amjsurg.2016.02.022
Paun BC, Cassie S, MacLean AR, Dixon E, Buie WD (2010) Postoperative complications following surgery for rectal cancer. Ann Surg 251:807–818. https://doi.org/10.1097/SLA.0b013e3181dae4ed
Yamauchi H, Togashi K, Kawamura YJ, Horie H, Sasaki J, Tsujinaka S, Yasuda Y, Konishi F (2008) Pathological predictors for lymph node metastasis in T1 colorectal cancer. Surg Today 38:905–910. https://doi.org/10.1007/s00595-007-3751-x
Butte JM, Tang P, Gonen M, Shia J, Schattner M, Nash GM, Temple LKF, Weiser MR (2012) Rate of residual disease after complete endoscopic resection of malignant colonic polyp. Dis Colon Rectum 55:122–127. https://doi.org/10.1097/DCR.0b013e3182336c38
Benizri EI, Bereder J-M, Rahili A, Bernard JL, Vanbiervliet G, Filippi J, Hébuterne X, Benchimol D (2012) Additional colectomy after colonoscopic polypectomy for T1 colon cancer: a fine balance between oncologic benefit and operative risk. Int J Color Dis 27:1473–1478. https://doi.org/10.1007/s00384-012-1464-0
Brown IS, Bettington ML, Bettington A, Miller G, Rosty C (2016) Adverse histological features in malignant colorectal polyps: a contemporary series of 239 cases. J Clin Pathol 69:292–299. https://doi.org/10.1136/jclinpath-2015-203203
Fischer J, Dobbs B, Dixon L, Eglinton TW, Wakeman CJ, Frizelle FA, on behalf of the New Zealand Malignant Polyp Study (NZ MAPS) group (2017) Management of malignant colorectal polyps in New Zealand. ANZ J Surg 87:350–355. https://doi.org/10.1111/ans.13502
Fasoli R, Nienstedt R, De Carli N et al (2015) The management of malignant polyps in colorectal cancer screening programmes: a retrospective Italian multi-centre study. Dig Liver Dis 47:715–719. https://doi.org/10.1016/j.dld.2015.04.011
Jung E-J, Ryu C-G, Paik JH et al (2015) Undetermined margins after colonoscopic polypectomy for malignant polyps: the need for radical resection. Anticancer Res 35:6887–6891 http://www.ncbi.nlm.nih.gov/pubmed/26637912 (accessed May 29, 2017)
Backes Y, de Vos tot Nederveen Cappel WH, van Bergeijk J et al (2017) Risk for incomplete resection after macroscopic radical endoscopic resection of T1 colorectal cancer: a multicenter cohort study. Am. J. Gastroenterol 112:785–796. https://doi.org/10.1038/ajg.2017.58
McDermott FD, Heeney A, Kelly ME, Steele RJ, Carlson GL, Winter DC (2015) Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg 102:462–479. https://doi.org/10.1002/bjs.9697
Rutegård M, Kverneng Hultberg D, Angenete E, Lydrup ML (2017) Substantial underreporting of anastomotic leakage after anterior resection for rectal cancer in the Swedish Colorectal Cancer Registry. Acta Oncol 56:1741–1745. https://doi.org/10.1080/0284186X.2017.1332423
Gill MD, Rutter MD, Holtham SJ (2013) Management and short-term outcome of malignant colorectal polyps in the north of England. Color Dis 15:169–176
T.D.G. Belderbos, F.N. van Erning, I.H.J.T. de Hingh et al. Long-term recurrence-free survival after standard endoscopic resection versus surgical resection of submucosal invasive colorectal cancer: a population-based study. Clin. Gastroenterol. Hepatol. 15 (2017) 403–411.e1. doi:https://doi.org/10.1016/j.cgh.2016.08.041
Levic K, Kjær M, Bulut O et al (2015) Watchful waiting versus colorectal resection after polypectomy for malignant colorectal polyps. Dan Med J 62(1):A4996
R. Steele, C. Pox, E. Kuipers et al. European guidelines for quality assurance in colorectal cancer screening and diagnosis. First edition – management of lesions detected in colorectal cancer screening. Endoscopy. 2012 Sep;44 Suppl 3:SE140–50. doi:https://doi.org/10.1055/s-0032-1309802
Watanabe T, Muro K, Ajioka Y et al (2017) Japanese Society for Cancer of the Colon and Rectum, Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer. Int J Clin Oncol 23:1–34. https://doi.org/10.1007/s10147-017-1101-6
Choi JY, Jung S-A, Shim K-N, Cho WY, Keum B, Byeon JS, Huh KC, Jang BI, Chang DK, Jung HY, Kong KA, The Korean ESD Study Group (2015) Meta-analysis of predictive clinicopathologic factors for lymph node metastasis in patients with early colorectal carcinoma. J Korean Med Sci 30:398–406. https://doi.org/10.3346/jkms.2015.30.4.398
Bosch SL, Teerenstra S, de Wilt JHW et al (2013) Predicting lymph node metastasis in pT1 colorectal cancer: a systematic review of risk factors providing rationale for therapy decisions. Endoscopy 45:827–834. https://doi.org/10.1055/s-0033-1344238
Toh E-W, Brown P, Morris E, Botterill I, Quirke P (2015) Area of submucosal invasion and width of invasion predicts lymph node metastasis in pT1 colorectal cancers. Dis Colon Rectum 58:393–400. https://doi.org/10.1097/DCR.0000000000000315
Koelzer VH, Lugli A, Dawson H, Hädrich M, Berger MD, Borner M, Mallaev M, Galván JA, Amsler J, Schnüriger B, Zlobec I, Inderbitzin D (2014) CD8/CD45RO T-cell infiltration in endoscopic biopsies of colorectal cancer predicts nodal metastasis and survival. J Transl Med 12:81. https://doi.org/10.1186/1479-5876-12-81
Lugli A, Kirsch R, Ajioka Y, Bosman F, Cathomas G, Dawson H, el Zimaity H, Fléjou JF, Hansen TP, Hartmann A, Kakar S, Langner C, Nagtegaal I, Puppa G, Riddell R, Ristimäki A, Sheahan K, Smyrk T, Sugihara K, Terris B, Ueno H, Vieth M, Zlobec I, Quirke P (2017) Recommendations for reporting tumor budding in colorectal cancer based on the international tumor budding consensus conference (ITBCC) 2016. Mod Pathol 30:1299–1311. https://doi.org/10.1038/modpathol.2017.46
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors (retrospective study). The study was approved by the National Committee on Health Research and reported to Danish Data Protection Agency.
Additional information
Tine Plato Hansen and Ismail Gögenur are part of the Danish Colorectal Cancer Group
Rights and permissions
About this article
Cite this article
Levic, K., Bulut, O., Hansen, T.P. et al. Malignant colorectal polyps: endoscopic polypectomy and watchful waiting is not inferior to subsequent bowel resection. A nationwide propensity score-based analysis. Langenbecks Arch Surg 404, 231–242 (2019). https://doi.org/10.1007/s00423-018-1706-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-018-1706-x