Abstract
Purpose
Ampullary neuroendocrine neoplasms (NENs) account for < 0.3% of gastrointestinal NENs. Surgical options include transduodenal ampullectomy/tumour excision or pancreaticoduodenectomy (PD). We report the experience of two high-volume pancreatic surgical centres of ampullary NENs.
Methods
Clinical records of patients who underwent surgery for ampullary NENs (January 2007–November 2017) in the study centres were retrieved retrospectively. We evaluated clinical–pathological features, post-operative outcome and follow-up (FU).
Results
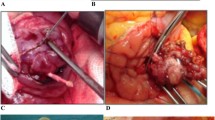
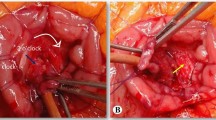
Eighteen patients (9 M/9 F, averaging 62 years) were enrolled. All but one were non-functioning NENs; four (22%) patients presented with jaundice. Seven (39%) of the patients underwent ampullectomy/excision (median tumour size 1.5 cm), and 11 (61%) patients underwent PD (median tumour size 2.4 cm). The median operation time of ampullectomy/excision was 221 min with operative blood loss of 75 ml (vs. 506 min and 425 ml in PD). The median hospital stay was 10 days in both groups. Overall surgical morbidity was 33%, due to four biochemical leaks, one pancreatic fistula and one abdominal haemorrhage. No reoperations were needed. The median tumour size was 1.8 (range 0.5–6.7) cm. All G2–G3 NENs were N1 (vs. 1/7 in G1 NENs). Three (17%) cases were mixed exocrine/G3 NECs. After a median FU of 45 (up to 124) months, recurrence occurred in four G3 NEC (31%) patients (median disease-free survival 14 months) after an R0 PD. Disease-related survival was 93, 77 and 66% at 1, 3 and 5 years, respectively.
Conclusion
Ampullary NENs are mostly G1–G2 neoplasms. Lymph node metastases rarely occur in G1 NENs < 2 cm in size, which may be treated with ampullectomy/excision. Survival is 66% 5 years after surgery.


Similar content being viewed by others
References
Hatzitheoklitos E, Büchler MW, Friess H, Poch B, Ebert M, Mohr W, Imaizumi T, Beger HG (1994) Carcinoid of the ampulla of Vater. Clinical characteristics and morphologic features. Cancer 73(6):1580–1588
Solcia E, Klöppel G, Sobin LH (eds) (2000) Histological typing of endocrine tumours, 2nd edn. Springer, Heidelberg
Ricci JL (1993) Carcinoid of the ampulla of Vater. Local resection or pancreaticoduodenectomy. Cancer 71(3):686–690
Hartel M, Wente MN, Sido B et al (2005) Carcinoid of the ampulla of Vater. J Gastroenterol Hepatol 20(5):676–681
Carter JT, Grenert JP, Rubenstein L, Stewart L, Way LW (2009) Neuroendocrine tumors of the ampulla of Vater: biological behavior and surgical management. Arch Surg 144(6):527–531
De Palma GD, Masone S, Siciliano S et al (2010) Endocrine carcinoma of the major papilla: report of two cases and review of the literature. Surg Oncol 19:235–242
Yang K, Yun SP, Kim S, Shin N, Park DY, Seo HI (2017) Clinicopathological features and surgical outcomes of neuroendocrine tumors of ampulla of Vater. BMC Gastroenterol 17(1):70
Makhlouf HR, Burke AP, Sobin LH (1999) Carcinoid tumors of the ampulla of Vater: a comparison with duodenal carcinoid tumors. Cancer 85:1241–1249
Garbrecht N, Anlauf M, Schmitt A, Henopp T, Sipos B, Raffel A, Eisenberger CF, Knoefel WT, Pavel M, Fottner C, Musholt TJ, Rinke A, Arnold R, Berndt U, Plockinger U, Wiedenmann B, Moch H, Heitz PU, Komminoth P, Perren A, Kloppel G (2008) Somatostatin-producing neuroendocrine tumors of the duodenum and pancreas: incidence, types, biological behavior, association with inherited syndromes, and functional activity. Endocr Relat Cancer 15(1):229–241
Cannon ME, Carpenter SL, Elta GH, Nostrant TT, Kochman ML, Ginsberg GG, Stotland B, Rosato EF, Morris JB, Eckhauser F, Scheiman JM (1999) EUS compared with CT, magnetic resonance imaging, and angiography and the influence of biliary stenting on staging accuracy of ampullary neoplasms. Gastrointest Endosc 50:27–33
Gabriel M, Decristoforo C, Kendler D, Dobrozemsky G, Heute D, Uprimny C, Kovacs P, von Guggenberg E, Bale R, Virgolini IJ (2007) 68Ga-DOTA-Tyr3-octreotide PET in neuroendocrine tumors: comparison with somatostatin receptor scintigraphy and CT. J Nucl Med 48:508–518
Gilani N, Ramirez FC (2007) Endoscopic resection of an ampullary carcinoid presenting with upper gastrointestinal bleeding: a case report and review of the literature. World J Gastroenterol 13(8):1268–1270
Odabasi M, Yildiz KM, Cengiz E, Hasan AH, Gunay E, Ozkan E, Aktekin A, Kaya B, Muftuoglu TM (2013) Treatment of ampullary neuroendocrine tumor by endoscopic snare papillectomy. Am J Case Rep 14:439–443
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Büchler MW (2007) Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142(1):20–25
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG, Conlon K, del Chiaro M, Falconi M, Fernandez-Cruz L, Fernandez-del Castillo C, Fingerhut A, Friess H, Gouma DJ, Hackert T, Izbicki J, Lillemoe KD, Neoptolemos JP, Olah A, Schulick R, Shrikhande SV, Takada T, Takaori K, Traverso W, Vollmer CR, Wolfgang CL, Yeo CJ, Salvia R, Buchler M, International Study Group on Pancreatic Surgery (ISGPS) (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery 161(3):584–591
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, Yeo CJ, Büchler MW (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142(5):761–768
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Bosman FT, Carneiro F, Hruban RH, Theise ND (eds) (2010) WHO classification of tumors of the digestive system, 4th edn. International Agency for Research on Cancer (IARC), Lyon, pp 322–326
Rindi G, Klöppel G, Ahlman H et al (2006) TNM staging of foregut (neuro)endocrine tumors: a consensus proposal including a grading system. Virchows Arch 449:395–401
La Rosa S, Sessa F, Uccella S (2016) Mixed neuroendocrine-nonneuroendocrine neoplasms (MiNENs): unifying the concept of a heterogeneous group of neoplasms. Endocr Pathol 27(4):284–311
Albores-Saavedra J, Hart A, Chable-Montero F et al Carcinoid and high-grade neuroendocrine carcinoma of the ampulla of Vater: a comparative analysis of 139 cases from surveillance, epidemiology, and end results program—a population based study. Arch Pathol Lab Med 134(11):1692–1696
Kalogeraki A, Papadakis GZ, Tamiolakis D, Karvela-Kalogeraki I, Karvelas-Kalogerakis M, Segredakis J, Papadakis M, Moustou E, Datseri G, Tzardi M (2016) EUS - fine- needle aspiration biopsy (FNAB) in the diagnosis of pancreatic adenocarcinoma: a review. Rom J Intern Med 54(1):24–30
Rattner DW, Fernandez-del Castillo C, Brugge WR, Warshaw AL (1996) Defining the criteria for local resection of ampullary neoplasms. Arch Surg 131(4):366–371
Larghi A, Fuccio L, Chiarello G, Attili F, Vanella G, Paliani GB, Napoleone M, Rindi G, Larocca LM, Costamagna G, Ricci R (2014) Fine-needle tissue acquisition from subepithelial lesions using a forward-viewing linear echoendoscope. Endoscopy 46(1):39–45
Delle Fave G, O’Toole D, Sundin A et al (2016) ENETS consensus guidelines update for gastroduodenal neuroendocrine neoplasms. Neuroendocrinology 103(2):119–124
Dumitrascu T, Dima S, Herlea V, Tomulescu V, Ionescu M, Popescu I (2012) Neuroendocrine tumors of the ampulla of Vater: clinico-pathological features, surgical approach and assessment of prognosis. Langenbeck’s Arch Surg 397:933–943
Baptiste GG, Postlewait LM, Ethun CG, le N, Russell MC, Kooby DA, Staley CA, Maithel SK, Cardona K (2016) Is there an optimal surgical approach to neuroendocrine tumors of the ampulla? A single institution experience over 15 years. Am Surg 82(7):637–643
Pedicone R, Adham M, Hervieu V, Lombard-Bohas C, Guibal A, Scoazec JY, Chayvialle JA, Partensky C (2009) Long-term survival after pancreaticoduodenectomy for endocrine tumors of the ampulla of Vater and minor papilla. Pancreas 38:638–643
Gincul R, Ponchon T, Napoleon B, Scoazec JY, Guillaud O, Saurin JC, Ciocirlan M, Lepilliez V, Pioche M, Lefort C, Adham M, Pialat J, Chayvialle JA, Walter T (2016) Endoscopic treatment of sporadic small duodenal and ampullary neuroendocrine tumors. Endoscopy 48(11):979–986
Iwasaki T, Nara S, Kishi Y, Esaki M, Shimada K, Hiraoka N (2017) Surgical treatment of neuroendocrine tumors in the second portion of the duodenum: a single center experience and systematic review of the literature. Langenbeck’s Arch Surg 402(6):925–933
Salmi S, Ezzedine S, Vitton V, Ménard C, Gonzales JM, Desjeux A, Grimaud JC, Barthet M (2012) Can papillary carcinomas be treated by endoscopic ampullectomy? Surg Endosc 26(4):920–925
Clements WM, Martin SP, Stemmerman G, Lowy AM (2003) Ampullary carcinoid tumors: rationale for an aggressive surgical approach. J Gastrointest Surg 7(6):773–776
Randle RW, Ahmed S, Newman NA, Clark CJ (2014) Clinical outcomes for neuroendocrine tumors of the duodenum and ampulla of Vater: a population-based study. J Gastrointest Surg 18(2):354–362
Schneider L, Contin P, Fritz S, Strobel O, Büchler MW, Hackert T (2016) Surgical ampullectomy: an underestimated operation in the era of endoscopy. HPB (Oxford) 18(1):65–71
Vanoli A, La Rosa S, Klersy C et al (2017) Four neuroendocrine tumor types and neuroendocrine carcinoma of the duodenum: analysis of 203 cases. Neuroendocrinology 104:112–125
Nassar H, Albores-Saavedra J, Klimstra DS (2005) High-grade neuroendocrine carcinoma of the ampulla of Vater. A clinicopathologic and immunohistochemical analysis of 14 cases. Am J Surg Pathol 29:588–594
Mahansaria SS, Agrawal N, Arora A, Bihari C, Appukuttan M, Chattopadhyay TK (2017) Ampullary mixed adenoneuroendocrine carcinoma: surprise histology, familiar management. Int J Surg Pathol 25(7):585–591
Klein F, Jacob D, Bahra M et al (2014) Prognostic factors for long-term survival in patients with ampullary carcinoma: the results of a 15-year observation period after pancreaticoduodenectomy. HPB Surg 2014:970234
Ostojic SM, Knezevic DR, Perisic M, Jurisic V, Knezevic SM (2015) The importance of choice of resection procedures in T1 and T2 stage of carcinoma of the ampulla of Vater. J BUON 20(5):1206–1214
Korse CM, Taal BG, van Velthuysen ML et al (2013) Incidence and survival of neuroendocrine tumours in the Netherlands according to histological grade: experience of two decades of cancer registry. Eur J Cancer 49(8):1975–1983
Author information
Authors and Affiliations
Contributions
Study conception and design: Milanetto A.C., Pasquali C., Zerbi A. Acquisition of the data: Milanetto A.C., Da Broi M., Brambilla T., Capretti G. Analysis and interpretation of the data: Milanetto A.C., Da Broi M., Brambilla T., Capretti G. Drafting of the manuscript: Milanetto A.C. Critical revision of the manuscript: Pasquali C., Zerbi A.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The research ethics committee of Humanitas Research Hospital (Rozzano, Milan, Italy) approved the retrospective study (15/2018).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
This paper was partially (series from the University of Padua) presented as an abstract at the European Pancreatic Club (EPC) Meeting in 2017.
Rights and permissions
About this article
Cite this article
Milanetto, A.C., Pasquali, C., Da Broi, M. et al. Ampullary neuroendocrine neoplasms: surgical experience of a rare and challenging entity. Langenbecks Arch Surg 403, 581–589 (2018). https://doi.org/10.1007/s00423-018-1695-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-018-1695-9