Abstract
Purpose
The aim of this study was to analyse preoperative risk factors for mortality or intensive care unit admission to describe severe peritonitis.
Methods
This was a single academic centre retrospective study of consecutive adult patients operated for diffuse secondary peritonitis between 2012 and 2013. Patients with appendicitis or cholecystitis were excluded. Independent risk factors were identified using binary and ordinal logistic regression.
Results
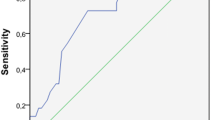
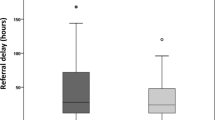
A total of 223 patients were analysed. Overall 30-day mortality was 14.5 %. Postoperatively, 32.3 % of patients were admitted into the intensive care unit (ICU). Independent risk factors for severe peritonitis were septic shock (odds ratio (OR) 37.94, 95 % confidence interval (CI) 14.52–99.13), chronic kidney insufficiency (OR 5.98 (95 % CI 1.56–22.86), severe sepsis (OR 4.80, 95 % CI 2.10–10.65) and cardiovascular disease (OR 2.58, 95 % CI 1.22–5.47). Patients lacking these factors had no mortality. ICU admission was refused in 24 (10.8 %) patients with 70.8 % mortality. In a subgroup of patients without treatment limitations (n = 190), independent risk factors for weighted outcome of ICU admission or mortality were septic shock (OR 11.89, 95 % CI 4.98–28.40), severe sepsis (OR 5.56, 95 % CI 2.39–12.89), metastatic malignant disease or lymphoma (OR 3.11, 95 % CI 1.34–7.20) and corticosteroid use (OR 2.98, 95 % CI 1.18–7.51). When receiving full level of care, patients with preoperative organ dysfunctions in this subgroup had 8.2 % 30-day mortality.
Conclusions
Preoperative organ dysfunctions, chronic kidney insufficiency and cardiovascular disease are the most important risk factors for severe peritonitis. Without these risk factors, patients had no mortality.
Similar content being viewed by others
References
Pieracci FM, Barie PS (2007) Management of severe sepsis of abdominal origin. Scand J Surg 96:184–196
Hynninen M, Wennervirta J, Leppäniemi A, Pettilä V (2008) Organ dysfunction and long term outcome in secondary peritonitis. Langenbecks Arch Surg 393:81–86
Karlsson S, Varpula M, Ruokonen E, Pettilä V, Parviainen I, Ala-Kokko TI, Kolho E, Rintala EM (2007) Incidence, treatment, and outcome of severe sepsis in ICU-treated adults in Finland: the Finnsepsis study. Intensive Care Med 33:435–443
Sartelli M, Catena F, Di Saverio S et al (2014) Current concept of abdominal sepsis: WSES position paper. World J Emerg Surg 9:22
Angus DC, van der Poll T (2013) Severe sepsis and septic shock. N Engl J Med 369:840–851
Mulier S, Penninckx F, Verwaest C, Filez L, Aerts R, Fieuws S, Lauwers P (2003) Factors affecting mortality in generalized postoperative peritonitis: multivariate analysis in 96 patients. World J Surg 27:379–384
Sartelli M, Pierluigi V, Catena F et al (2013) 2013 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg 8:3
Dellinger RP, Levy MM, Rhodes A et al. (2012) Surviving sepsis campaign guidelines committee including the pediatric subgroup: surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock. Critical Care Medicine 41(2013)580–637.
Buck DL, Vester-Andersen M, Møller MH (2013) Surgical delay is a critical determinant of survival in perforated peptic ulcer. Br J Surg 100:1045–1049
Azuhata T, Kinoshita K, Kawano D, Komatsu T, Sakurai A, Chiba Y, Tanjho K (2014) Time from admission to initiation of surgery for source control is a critical determinant of survival in patients with gastrointestinal perforation with associated septic shock. Crit Care 18:R87
Hecker A, Uhle F, Schwandner T, Padberg W, Weigand MA (2013) Diagnostics, therapy and outcome prediction in abdominal sepsis: current standards and future perspectives. Langenbecks Arch Surg 399:11–22
Mulari K, Leppäniemi A (2004) Severe secondary peritonitis following gastrointestinal tract perforation. Scand J Surg 93:204–208
Gauzit R, Péan Y, Barth X, Mistretta F, Lalaude O (2009) Top Study Team: epidemiology, management, and prognosis of secondary non-postoperative peritonitis: a French prospective observational multicenter study. Surg Infect 10:119–127
Wacha H, Hau T, Dittmer R, Ohmann C (1999) Risk factors associated with intraabdominal infections: a prospective multicenter study. Peritonitis Study Group. Langenbecks Arch Surg 384:24–32
Sallinen VJ, Leppäniemi AK, Mentula PJ (2015) Staging of acute diverticulitis based on clinical, radiologic, and physiologic parameters. J Trauma Acute Care Surg 78:543–551
Gutt CN, Encke J, Köninger J et al (2013) Acute cholecystitis: early versus delayed cholecystectomy, a multicenter randomized trial (ACDC study, NCT00447304). Ann Surg 258:385–393
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Linder MM, Wacha H, Feldmann U, Wesch G, Streifensand RA, Gundlach E (1987) The Mannheim peritonitis index. An instrument for the intraoperative prognosis of peritonitis. Chirurg 58:84–92
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22(199):707–710
Seymour CW, Liu VX, Iwashyna TJ et al (2016) Assessment of Clinical Criteria for Sepsis For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315:762–774
Sartelli M, Catena F, Ansaloni L et al (2012) Complicated intra-abdominal infections in Europe: a comprehensive review of the CIAO study. World J Emerg Surg 7:36
Kaukonen K-M, Bailey M, Suzuki S, Pilcher D, Bellomo R (2014) Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000–2012. JAMA 311:1308–1316
Sinuff T, Kahnamoui K, Cook DJ, Luce JM (2004) Values ethics and rationing in critical care task force: rationing critical care beds: a systematic review. Crit Care Med 32:1588–1597
Zhang Q, Raoof M, Chen Y, Sumi Y, Sursal T, Junger W, Brohi K, Itagaki K, Hauser CJ (2010) Circulating mitochondrial DAMPs cause inflammatory responses to injury. Nature 464:104–107
Seok J, Warren HS, Cuenca AG et al (2013) Genomic responses in mouse models poorly mimic human inflammatory diseases. Proc Natl Acad Sci U S A 110:3507–3512
Acknowledgments
We would like to thank Juho Mattila and Tomi Eronen for providing us with the data on emergency department and ICU patients, respectively.
Authors’ contributions
MT had full access to the data in the study and takes responsibility for the acquisition and integrity of the data and the accuracy of the data analysis. MT drafted the manuscript with the help of VS and PM. All authors (MT, VS, PM, AL) have been involved in study conception and design, analysis and interpretation of the data and revising the manuscript. All authors have read and approved the final manuscript and agree to be accountable for all aspects of the work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was financially supported by the Martti I. Turunen Foundation and Helsinki University Central Hospital Research Funds (Government Research Funds). The study was merely observational, and neither informed consent nor ethics committee’s approval was needed. Study design was approved by institutional review board (Helsinki University Central Hospital) on June 13, 2013.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
This study was presented at National Operative Days Conference, 25 November 2015, Helsinki, Finland
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 78 kb)
Rights and permissions
About this article
Cite this article
Tolonen, M., Sallinen, V., Mentula, P. et al. Preoperative prognostic factors for severe diffuse secondary peritonitis: a retrospective study. Langenbecks Arch Surg 401, 611–617 (2016). https://doi.org/10.1007/s00423-016-1454-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-016-1454-8