Abstract
Background
Patients with neuroendocrine neoplasms (NEN) develop hepatic metastases in 50–95 %. The aims of this study were to evaluate the outcome/prognosis of patients following hepatic surgery and to identify predictive factors for the selection of patient that benefit from hepatic tumor resection.
Patients and methods
In a retrospective single-center study (1990 to 2014), 204 patients with hepatic metastasis of NEN were included. Ninety-four were subjected to various forms of liver resection. According to the overall survival, the influence of several prognostic factors like the Ki-67 index, stage of disease, and resection status was evaluated.
Results
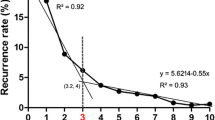
The primary tumor was located in the small intestine (n = 73), pancreas (n = 58), colon (n = 26), esophagus or stomach (n = 9) and in 38 patients the primary site was unknown. The Ki-67 index was associated with significant different overall survival. Patients with an R0 resection (n = 38) of their hepatic metastasis had a very good 10-year survival of 90.4 %. Patients in whom an R1 (n = 23) or R2 (n = 33) resection of their hepatic metastasis could be achieved had a 10-year survival of 53.4 and 51.4 %, respectively. The majority of the patients (53.9 %) could not be resected and had a poor 10-year survival rate of 19.4 %. Partial or complete control of endocrine-related symptoms was achieved in all patients with functioning tumors following surgery. The overall 5- and 10-year survival rates were 77.9 and 65.2 %, respectively.
Conclusion
Surgical resection of hepatic NEN metastases can reduce symptoms and improve the survival in selected patients with a Ki-67 index less than 20 %. The expected outcome has to be compared to the outcome of alternative treatment strategies. An R0 situation should be the aim of hepatic surgery, but also patients with R1 or R2 resection show a good survival benefit.








Similar content being viewed by others
References
Franko J, Feng W, Yip L, Genovese E, Moser AJ (2010) Non-functional neuroendocrine carcinoma of the pancreas: incidence, tumor biology, and outcomes in 2,158 patients. J Gastrointest Surg 14(3):541–548
Frilling A, Sotiropoulos GC, Li J, Kornasiewicz O, Plockinger U (2010) Multimodal management of neuroendocrine liver metastases. HPB (Oxford) 12(6):361–379
Cheung TT, Chok KS, Chan AC, Tsang S, Dai JW, Lang BH, Yau T, Chan SC, Poon RT, Fan ST, Lo CM (2014) Long term survival analysis of hepatectomy for neuroendocrine tumour liver metastases. ScientificWorldJournal 2014:524045
Frilling A, Clift AK (2014) Therapeutic strategies for neuroendocrine liver metastases. Cancer. doi:10.1002/cncr.28760
Lesurtel M, Nagorney DM, Mazzaferro V, Jensen RT, Poston GJ (2015) When should a liver resection be performed in patients with liver metastases from neuroendocrine tumours? A systematic review with practice recommendations. HPB (Oxford) 17(1):17–22
Steinmuller T, Kianmanesh R, Falconi M, Scarpa A, Taal B, Kwekkeboom DJ, Lopes JM, Perren A, Nikou G, Yao J, Delle Fave GF, O'Toole D (2008) Consensus guidelines for the management of patients with liver metastases from digestive (neuro)endocrine tumors: foregut, midgut, hindgut, and unknown primary. Neuroendocrinology 87(1):47–62
Ramage JK, Davies AH, Ardill J, Bax N, Caplin M, Grossman A, Hawkins R, McNicol AM, Reed N, Sutton R, Thakker R, Aylwin S, Breen D, Britton K, Buchanan K, Corrie P, Gillams A, Lewington V, McCance D, Meeran K, Watkinson A (2005) Guidelines for the management of gastroenteropancreatic neuroendocrine (including carcinoid) tumours. Gut 54(Suppl 4):iv1–iv16
Oberg K, Astrup L, Eriksson B, Falkmer SE, Falkmer UG, Gustafsen J, Haglund C, Knigge U, Vatn MH, Valimaki M (2004) Guidelines for the management of gastroenteropancreatic neuroendocrine tumours (including bronchopulmonary and thymic neoplasms). Part I—general overview. Acta Oncol 43(7):617–625
Gurusamy KS, Ramamoorthy R, Sharma D, Davidson BR (2009) Liver resection versus other treatments for neuroendocrine tumours in patients with resectable liver metastases. Cochrane Database Syst Rev 2, CD007060
Pavel M, Baudin E, Couvelard A, Krenning E, Oberg K, Steinmuller T, Anlauf M, Wiedenmann B, Salazar R (2012) ENETS Consensus Guidelines for the management of patients with liver and other distant metastases from neuroendocrine neoplasms of foregut, midgut, hindgut, and unknown primary. Neuroendocrinology 95(2):157–176
Frilling A, Modlin IM, Kidd M, Russell C, Breitenstein S, Salem R, Kwekkeboom D, Lau WY, Klersy C, Vilgrain V, Davidson B, Siegler M, Caplin M, Solcia E, Schilsky R (2014) Recommendations for management of patients with neuroendocrine liver metastases. Lancet Oncol 15(1):e8–e21
Arigoni S, Ignjatovic S, Sager P, Betschart J, Buerge T, Scherrer E, Wachtl J, Tschuor C, Limani P, Puhan MA, Lesurtel M, Raptis DA, Breitenstein S (2014) Diagnosis and prediction of neuroendocrine liver metastases: a protocol of six systematic reviews. JMIR Res Protoc 3(2):e25
Bacchetti S, Bertozzi S, Londero AP, Uzzau A, Pasqual EM (2013) Surgical treatment and survival in patients with liver metastases from neuroendocrine tumors: a meta-analysis of observational studies. Int J Hepatol 2013:235040
Chen H, Hardacre JM, Uzar A, Cameron JL, Choti MA (1998) Isolated liver metastases from neuroendocrine tumors: does resection prolong survival? J Am Coll Surg 187(1):88–92, discussion 92-83
Grazi GL, Cescon M, Pierangeli F, Ercolani G, Gardini A, Cavallari A, Mazziotti A (2000) Highly aggressive policy of hepatic resections for neuroendocrine liver metastases. Hepatogastroenterology 47(32):481–486
Ahmed A, Turner G, King B, Jones L, Culliford D, McCance D, Ardill J, Johnston BT, Poston G, Rees M, Buxton-Thomas M, Caplin M, Ramage JK (2009) Midgut neuroendocrine tumours with liver metastases: results of the UKINETS study. Endocr Relat Cancer 16(3):885–894
Salama A, Badawy O, Mokhtar N (2014) Ki-67 is a powerful tool for grading neuroendocrine tumors among Egyptian patients: a 10-year experience. J Cancer Res Clin Oncol 140(4):653–661
Miller HC, Drymousis P, Flora R, Goldin R, Spalding D, Frilling A (2014) Role of Ki-67 proliferation index in the assessment of patients with neuroendocrine neoplasias regarding the stage of disease. World J Surg 38(6):1353–1361
Chi YH, Jiang WC, Du F, Sun YK, Song Y, Yang L, Zhou AP, Wang JW (2013) Neuroendocrine tumors: analysis of 252 cases. Zhonghua Zhong Liu Za Zhi 35(1):67–70
Foltyn W, Zajecki W, Marek B, Kajdaniuk D, Sieminska L, Zemczak A, Kos-Kudla B (2012) The value of the Ki-67 proliferation marker as a prognostic factor in gastroenteropancreatic neuroendocrine tumours. Endokrynol Pol 63(5):362–366
Musholt TJ, Lang H (2009) Indications and operative procedures for neuroendocrine liver metastases. Chirurg 80(2):113–121
Acknowledgments
We thank Novartis for sponsoring the development of the database Software MaDoc.
Conflicts of interest
No potential conflicts of interest to be announced.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Watzka, F.M., Fottner, C., Miederer, M. et al. Surgical therapy of neuroendocrine neoplasm with hepatic metastasis: patient selection and prognosis. Langenbecks Arch Surg 400, 349–358 (2015). https://doi.org/10.1007/s00423-015-1277-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-015-1277-z