Abstract
Purpose
Preoperative diagnosis of thyroid nodules with “follicular neoplasm” (FN) based on fine-needle aspiration cytology (FNAC) forces thyroidectomy to exclude malignancy. This study explores if 18F-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG-PET/CT) provides information enough to prevent unnecessary thyroidectomies in this clinical setting.
Methods
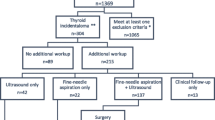
This is a prospective study involving 46 consecutive patients scheduled for thyroidectomy due to follicular neoplasm diagnosis in FNAC (36 follicular, 10 Hürthle cell neoplasms, Bethesda classification) since January 2009 until April 2012. All patients underwent preoperative 18F-FDG-PET/CT. Abnormal 18F-FDG thyroid uptake was assessed visually and by measuring the maximum standard uptake value (SUVmax). Results were compared with definitive pathology reports.
Results
Thirteen out of 46 patients (28.3 %) were finally diagnosed with thyroid cancer. Focal uptake correlated with a greater risk of malignancy (p = 0.009). 18F-FDG-PET/CT focal uptake showed sensitivity, specificity, positive and negative predictive values and overall accuracy of 92.3, 48.5, 41.4, 94.1 and 60.9 %, respectively. The optimal threshold SUVmax to discriminate malignancy was 4.2 with an area under receiver-operating characteristic curve of 0.76 (95 % confidence interval, 0.60–0.90). Use of 18F-FDG-PET/CT could reduce by 13–25 % the number of thyroidectomies performed for definitive benign nodules. However, it has demonstrated worse predictive ability in the subgroup of patients with diffuse uptake, oncocytic pattern in FNAC and lesions smaller than 2.
Conclusions
18F-FDG-PET/CT can play a role in the management of thyroid nodules larger than 2 cm cytologically reported as follicular neoplasm without oncocytic differentiation, allowing the avoidance of a significant number of thyroidectomies for definitive benign lesions.



Similar content being viewed by others
References
Gharib H, Papini E (2007) Thyroid nodules: clinical importance, assessment, and treatment. Endocrinol Metab Clin N Am 36:707–735
Pacini F, Schlumberger M, Dralle H, Elisei R, Smit JWA, Wiersinga W, The European Thyroid Cancer Taskforce Consensus Statement (2006) European consensus for the management of patients with differentiated thyroid carcinoma of the follicular epithelium. Eur J Endocrinol 154:787–803
Cooper DS, Doherty GM, Haugen BR et al (2009) Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. The American Thyroid Association (ATA) guidelines taskforce on thyroid nodules and differentiated thyroid cancer. Thyroid 19:1167–1214
Cibas ES, Ali SZ (2009) The Bethesda system for reporting thyroid cytopathology. Am J Clin Pathol 132:658–665
Greaves TS, Olvera M, Florentine BD et al (2000) Follicular lesions of thyroid: a 5-year fine-needle aspiration experience. Cancer 90:335–341
Baloch ZW, LiVolsi VA, Asa SL et al (2008) Diagnostic terminology and morphologic criteria for cytologic diagnosis of thyroid lesions: a synopsis of the National Cancer Institute Thyroid fine-needle aspiration state of the science conference. Diagn Cytopathol 36:425–443
British Thyroid Association, Royal College of Physicians (2007) Guidelines for the management of thyroid cancer. In: Perros P (ed) Report of the Thyroid Cancer Guidelines Update Group, 2nd edn. Royal College of Physicians, London
Layfield LJ, Abrams J, Cochand-Priollet B et al (2008) Post-thyroid FNA testing and treatment options: a synopsis of the National Cancer Institute Thyroid fine needle aspiration state of the science conference. Diagn Cytopathol 36:442–448
Musholt TJ, Clerici T, Dralle H, Frilling A, Goretzki PE et al (2011) German Association of Endocrine Surgeons practice guidelines for the surgical treatment of benign thyroid disease. Langenbecks Arch Surg 396:639–649. doi:10.1007/s00423-011-0774-y
Pacini F, Burroni L, Ciuoli C, Di Cairano G, Guarino E (2004) Management of thyroid nodules: a clinicopathological, evidence-based approach. Eur J Nucl Med Mol Imaging 31:1443–1449. doi:10.1007/s00259-004-1680-0
Rohren EM, Turkington TG, Coleman E (2004) Clinical applications of PET in oncology. Radiology 231:305–332
Wang W, Steven ML, Fazzari M et al (2000) Prognostic value of [18F]fluorodeoxyglucose positron emission tomographic scanning in patients with thyroid cancer. J Clin Endocrinol Metab 85:1107–1113
Esteva D, Muros MA, Llamas-Elvira JM et al (2009) Clinical and pathological factors related to 18F-FDG-PET positivity in the diagnosis of recurrence and/or metastasis in patients with differentiated thyroid cancer. Ann Surg Oncol 16:2006–2013
Kang KW, Kim SK, Kang HS et al (2003) Prevalence and risk of cancer of focal thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography for metastasis evaluation and cancer screening in healthy subjects. J Clin Endocrinol Metab 88:4100–4104
Cohen MS, Arslan N, Dehdashti F et al (2001) Risk of malignancy in thyroid incidentalomas identified by fluorodeoxyglucose-positron emission tomography. Surgery 130:941–946
Kim TY, Kim WB, Ryu JS, Gong G, Hong SJ, Shong YK (2005) 18F-Fluorodeoxyglucose uptake in thyroid from positron emission tomogram (PET) for evaluation in cancer patients: high prevalence of malignancy in thyroid PET incidentaloma. Laryngoscope 115:1074–1078
Chen YK, Ding HJ, Chen KT et al (2005) Prevalence and risk of cancer of focal thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography for cancer screening in healthy Subjects. Anticancer Res 25:1421–1426
Bogsrud TV, Karantanis D, Nathan MA et al (2007) The value of quantifying 18F-FDG uptake in thyroid nodules found incidentally on whole-body PET-CT. Nucl Med Commun 28:373–381
Are C, Hsu JF, Ghossein RA et al (2007) Histological aggressiveness of fluorodeoxyglucose positron-emission tomogram (FDG-PET)-detected incidental thyroid carcinomas. Ann Surg Oncol 14:3210–3215
Choi JW, Yoon YH, Kim SM, Koo BS (2011) Characteristics of primary papillary thyroid carcinoma with false-negative findings on initial (18)F-FDG PET/CT. Ann Surg Oncol 18:1306–1311
Heston TF, Wahl RL (2010) Molecular imaging in thyroid cancer. Cancer imaging 20:1–7
Kresnik E, Gallowitsch HJ, Mikosch P et al (2003) Fluorine-18-fluorodeoxyglucose positron emission tomography in the preoperative assessment of thyroid nodules in an endemic goitre area. Surgery 133:294–299
Kim JM, Riu JS, Kim TK et al (2007) 18F-Fluorodeoxyglucose positron emission tomography does not predict malignancy in thyroid nodules cytologically diagnosed as follicular neoplasm. J Clin Endocrinol Metab 92:1630–1634
Traugott AL, Dehdashti F, Trinkaus K et al (2010) Moley exclusion of malignancy in thyroid nodules with indeterminate fine-needle aspiration cytology after negative 18F-fluorodeoxyglucose positron emission tomography: interim analysis. World J Surg 34:1247–1253. doi:10.1007/s00268-010-0398-3
De Lellis RA, Lloyd RV, Heitz PU, Eng C (2004) World health classification of tumours. Pathology and genetics of tumours of endocrine organs. IARC, Lyon
Giammarile F, Hafdi Z, Bournaud C et al (2003) Is (18F)-2-fluoro-2-deoxy-d-glucose (FDG) scintigraphy with non-dedicated positron emission tomography useful in the diagnostic management of suspected metastatic thyroid carcinoma in patients with no detectable radioiodine uptake? Eur J Endocrinol 149:293–300
Freudenberg LS, Antoch G, Frilling A et al (2008) Combined metabolic and morphologic imaging in thyroid carcinoma patients with elevated serum thyroglobulin and negative cervical ultrasonography: role of 124I-PET/CT and FDG-PET. Eur J Nucl Med Mol Imaging 35:950–957
Dong MJ, Liu ZF, Zhao K et al (2009) Value of 18F-FDG-PET/PET-CT in differentiated thyroid carcinoma with radioiodine-negative whole-body scan: a meta-analysis. Nucl Med Commun 30:639–650
Mitchell JC, Grant F, Evenson AR et al (2005) Preoperative evaluation of thyroid nodules with 18F-FDG-PET/CT. Surgery 138:1166–1175
Pagano L, Samá MT, Moriani F et al (2011) Thyroid incidentaloma identified by 18F-fluorodeoxiyglucose positron emission tomography with CT (FDG-PET/PET-CT): clinical and pathological relevance. Clin Endocrinol 75(4):528–534. doi:10.1111/j.1365-2265.2011.04107.x
de Geus-Oei LF, Pieters GF, Bonenkamp JJ et al (2006) 18F-FDG PET reduces unnecessary hemithyroidectomies for thyroid nodules with inconclusive cytologic results. J Nucl Med 47:770–775
Sebastianes FM, Cerci JJ, Zanoni PH et al (2007) Role of 18F-fluorodeoxyglucose positron emission tomography in preoperative assessment of cytologically indeterminate thyroid nodules. J Clin Endocrinol Metab 92:4485–4488
Vriens D, de Wilt JHW, Van del Wilt GJ, Netea-Maier RT, Oyen WJG, de Geus-Oei LF (2011) The role of [18F]-2-fluoro-2-deoxy-d-glucose-positron emission tomography in thyroid nodules with indeterminate fine-needle aspiration biopsy. Systematic review and meta-analysis of the literature. Cancer 117:4582–4594
Hales NW, Krempl GA, Medina JE (2008) Is there a role for fluorodeoxyglucose positron emission tomography/computed tomography in cytologically indeterminate thyroid nodules? Am J Otolaryngol 29:113–118
Smith RB, Robinson RA, Hoffman HT, Graham MM (2008) Preoperative FDG-PET imaging to assess the malignant potential of follicular neoplasms of the thyroid. Otolaryngol Head Neck Surg 138:101–106
Shie P, Cardarelli R, Sprawls K et al (2009) Systematic review: prevalence of malignant incidental thyroid nodules identified on flurine-18 fluorodeoxyglucose positron emission tomography. Nucl Med Commun 30:742–748
Yasuda S, Shohtsu A, Ide M et al (1998) Chronic thyroiditis: diffuse uptake of FDG at PET. Radiology 207:775–778
Uematsu H, Sadato N, Ohtsubo T et al (1998) Fluorine-18-fluorodeoxyglucose PET versus thallium-201 scintigraphy evaluation of thyroid tumors. J Nuc Med 39:453–459
Karantanis D, Bogsrud TV, Wiseman GA et al (2007) Clinical significance of diffusely increased 18F-FDG uptake in the thyroid gland. J Nucl Med 48:896–901
Rosen J, He M, Umbricht C et al (2005) A six-gene model for differentiating benign from malignant thyroid tumors on the basis of gene expression. Surgery 138:1050–1057
Haber RS, Weiser KR, Pritsker A et al (1997) GLUT1 glucose transporter expression in benign and malignant thyroid nodules. Thyroid 7:363–367
Schonberger J, Ruschoff J, Grimm D et al (2002) Glucose transporter 1 gene expression is related to thyroid neoplasms with an unfavourable prognosis: an immunohistochemical study. Thyroid 12:747–754
Acknowledgments
This study received financial support from the Secretariat General on Quality and Modernization (Counselling of Health) of the Andalusian Regional Government through the Research Project 0057/2007 “Study of gene expression profile for the diagnostic and prognostic evaluation of patients with thyroid nodular lesions”.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was presented at the ESES Congress, Gothenburg, on May 25–26, 2012.
Rights and permissions
About this article
Cite this article
Muñoz Pérez, N., Villar del Moral, J.M., Muros Fuentes, M.A. et al. Could 18F-FDG-PET/CT avoid unnecessary thyroidectomies in patients with cytological diagnosis of follicular neoplasm?. Langenbecks Arch Surg 398, 709–716 (2013). https://doi.org/10.1007/s00423-013-1070-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-013-1070-9