Abstract
Introduction
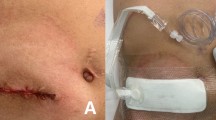
Surgical site infections (SSIs) are frequent complications in colorectal surgery and may lead to burst abdomen, incisional hernia, and increased perioperative costs. Plastic wound ring drapes (RD) were introduced some decades ago to protect the abdominal wound from bacteria and reduce SSIs. There have been no controlled trials examining the benefit of RD in laparoscopic colorectal surgery. The Reduction of wound infections in laparoscopic assisted colorectal resections by plastic wound ring drapes (REDWIL) trial was thus designed to assess their effectiveness in preventing SSIs after elective laparoscopic colorectal resections.
Materials/methods
REDWIL is a randomized controlled monocenter trial with two parallel groups (experimental group with RD and control group without RD). Patients undergoing elective laparoscopic colorectal resection were included. The primary endpoint was SSIs. Secondary outcomes were colonization of the abdominal wall with bacteria, reoperations/readmissions, early/late postoperative complications, and cost of hospital stay. The duration of follow-up was 6 months.
Results
Between January 2008 and October 2010, 109 patients were randomly assigned to the experimental or control group (with or without RD). Forty-six patients in the RD group and 47 patients in the control group completed follow-up. SSIs developed in ten patients with RD (21.7 %) and six patients without RD (12.8 %) (p = 0.28). An intraoperative swab taken from the abdominal wall was positive in 66.7 % of patients with RD and 57.5 % without RD (p = 0.46). The number of species cultured within one swab was significantly higher in those without RD (p = 0.03). The median total inpatient costs including emergency readmissions were 3,402 ± 4,038 € in the RD group and 3,563 ± 1,735 € in the control group (p = 0.869).
Conclusions
RD do not reduce the rate of SSIs in laparoscopic colorectal surgery. The inpatient costs are similar with and without RD.


Similar content being viewed by others
References
Hawn MT, Vick CC, Richman J, Holman W, Deierhoi RJ, Graham LA, Henderson WG, Itani KM (2011) Surgical site infection prevention: time to move beyond the surgical care improvement program. Ann Surg 254:494–501
Konishi T, Watanabe T, Kishimoto J, Nagawa H (2006) Elective colon and rectal surgery differ in risk factors for wound infection: results of prospective surveillance. Ann Surg 244:758–63
Degrate L, Garancini M, Misani M, Poli S, Nobili C, Romano F, Giordano L, Motta V, Uggeri F (2011) Right colon, left colon, and rectal surgeries are not similar for surgical site infection development. Analysis of 277 elective and urgent colorectal resections. Int J Color Dis 26:61–9
Niggebrugge AH, Hansen BE, Trimbos JB, van de Velde CJ, Zwaveling A (1995) Mechanical factors influencing the incidence of burst abdomen. Eur J Surg 161:655–61
Murray BW, Cipher DJ, Pham T, Anthony T (2011) The impact of surgical site infection on the development of incisional hernia and small bowel obstruction in colorectal surgery. Am J Surg 202:558–60
Nyström PO, Broome A, Höjer H, Ling L (1984) A controlled trial of a plastic wound ring drape to prevent contamination and infection in colorectal surgery. Dis Colon Rectum 27:451–3
Psaila JV, Wheeler MH, Crosby DL (1977) The role of plastic wound drapes in the prevention of wound infection following abdominal surgery. Br J Surg 64:729–32
Nyström PO, Bröte L (1980) Effects of a plastic wound drape on contamination with enterobacteria and on infection after appendicectomy. Acta Chir Scand 146:65–70
Sookhai S, Redmond HP, Deasy JM (1999) Impervious wound-edge protector to reduce postoperative wound infection: a randomised, controlled trial. Lancet 353:1585
Eggert A, Eckardt K, Seidel H, Teichmann W (1980) Prevention of surgical wound infections by means of ring drapes. Chirurg 51:39–42
Stübs P, Schmidt C, Lippert H, Tautenhahn J (2004) Inzidenz und Einteilung postoperativer Wundinfektionen in der Viszeralchirurgie. Viszeralchirurgie 39:166–9
Kiran RP, El-Gazzaz GH, Vogel JD, Remzi FH (2010) Laparoscopic approach significantly reduces surgical site infections after colorectal surgery: data from national surgical quality improvement program. J Am Coll Surg 211:232–8
Galal I, El-Hindawy K (2011) Impact of using triclosan-antibacterial sutures on incidence of surgical site infection. Am J Surg 202:133–8
Justinger C, Moussavian MR, Schlueter C, Kopp B, Kollmar O, Schilling MK (2009) Antibacterial [corrected] coating of abdominal closure sutures and wound infection. Surgery 145:330–4
Baracs J, Huszár O, Sajjadi SG, Horváth OP (2011) Surgical site infections after abdominal closure in colorectal surgery using triclosan-coated absorbable suture (PDS Plus) vs. uncoated sutures (PDS II): a randomized multicenter study. Surg Infect (Larchmt) 12:483–9
Sørensen LT, Toft BG, Rygaard J, Ladelund S, Paddon M, James T, Taylor R, Gottrup F (2010) Effect of smoking, smoking cessation, and nicotine patch on wound dimension, vitamin C, and systemic markers of collagen metabolism. Surgery 148:982–90
Watanabe A, Kohnoe S, Shimabukuro R, Yamanaka T, Iso Y, Baba H, Higashi H, Orita H, Emi Y, Takahashi I, Korenaga D, Maehara Y (2008) Risk factors associated with surgical site infection in upper and lower gastrointestinal surgery. Surg Today 38:404–12
Kurmann A, Vorburger SA, Candinas D, Beldi G (2011) Operation time and body mass index are significant risk factors for surgical site infection in laparoscopic sigmoid resection: a multicenter study. Surg Endosc 25:3531–4
Llaguna OH, Avgerinos DV, Lugo JZ, Matatov T, Abbadessa B, Martz JE, Leitman IM (2010) Incidence and risk factors for the development of incisional hernia following elective laparoscopic versus open colon resections. Am J Surg 200:265–9
Vlug MS, Wind J, Hollmann MW, Ubbink DT, Cense HA, Engel AF, Gerhards MF, van Wagensveld BA, van der Zaag ES, van Geloven AAW, Sprangers MAG, Cuesta MA, Bemelman WA (2011) Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study). Ann Surg 254:868–75
Hackert T, Uhl W, Büchler MW (2002) Specimen retrieval in laparoscopic colon surgery. Dig Surg 19:502–6
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lauscher, J.C., Grittner, F., Stroux, A. et al. Reduction of wound infections in laparoscopic-assisted colorectal resections by plastic wound ring drapes (REDWIL)?—a randomized controlled trial. Langenbecks Arch Surg 397, 1079–1085 (2012). https://doi.org/10.1007/s00423-012-0954-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-012-0954-4