Abstract
Background
This systematic review aims to analyse the risk–benefit association of (1) prophylactic drains and/or (2) the time of their removal after pancreatic resection.
Materials and methods
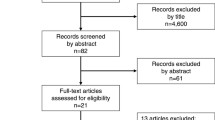
A systematic literature search (Medline, Embase, Biosis, and The Cochrane Library) was performed to identify all types of controlled trials comparing the role of drainage or the time of their removal on postoperative complications following pancreatic surgery. Meta-analysis was performed using a random-effects model.
Results
Four studies, two randomised trials and two prospective cohort studies, were included in the systematic review and meta-analysis. Removal of drains at day 5 or later did not show an influence on mortality, morbidity, re-intervention or hospital stay compared to no insertion of drains. Early (day 3–4) compared to late (≥ day 5) drain removal significantly reduced pancreatic fistulas (odds ratio (OR) 0.13; 95% confidence interval (CI) 0.03–0.32; P = 0.0002), intra-abdominal collections (OR 0.08; 95% CI 0.01–0.67; P = 0.02) and abscesses (OR 0.26; 95% CI 0.07–1.00; P = 0.05). Moreover, hospital stay was significantly reduced after early drain removal (mean difference −2.60 days; 95% CI −4.74 to −0.46; P = 0.02)
Conclusion
Further randomised controlled trials are warranted to clarify whether drains are of any use. In case of drain insertion, early removal seems to be superior to late removal.




Similar content being viewed by others
References
Robinson JO (1986) Surgical drainage: an historical perspective. Br J Surg 73:422–426
Dominguez FE, Post S (2003) Abdominal drainages. Chirurg 74:91–98
Petrowsky H, Demartines N, Rousson V, Clavien PA (2004) Evidence-based value of prophylactic drainage in gastrointestinal surgery: a systematic review and meta-analyses. Ann Surg 240:1074–1084
Dougherty SH, Simmons RL (1992) The biology and practice of surgical drains. Part II. Curr Probl Surg 29:633–730
Schein M (2008) To drain or not to drain? The role of drainage in the contaminated and infected abdomen: an international and personal perspective. World J Surg 32:312–321
Heslin MJ, Harrison LE, Brooks AD, Hochwald SN, Coit DG, Brennan MF (1998) Is intra-abdominal drainage necessary after pancreaticoduodenectomy? J Gastrointest Surg 2:373–378
Conlon KC, Labow D, Leung D, Smith A, Jarnagin W, Coit DG et al (2001) Prospective randomized clinical trial of the value of intraperitoneal drainage after pancreatic resection. Ann Surg 234:487–493
Kawai M, Tani M, Terasawa H, Ina S, Hirono S, Nishioka R et al (2006) Early removal of prophylactic drains reduces the risk of intra-abdominal infections in patients with pancreatic head resection: prospective study for 104 consecutive patients. Ann Surg 244:1–7
Bassi C, Molinari E, Malleo G, Grippa S, Butturini G, Salvia R et al (2010) Early versus late drain removal after standard pancreatic resections—results of a prospective randomized trial. Ann Surg 252:207–214
Büchler MW, Friess H (2006) Evidence forward, drainage on retreat: still we ignore and drain!? Ann Surg 244:8–9
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6:e1000100
Higgins JPT, Green S (2008) Cochrane handbook for systematic reviews of interventions. Wiley, Chichester
Downs SH, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52:377–384
The Nordic Cochrane Centre (2008) Review Manager (RevMan) Version 5.0 The Nordic Cochrane Centre, Copenhagen
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Heslin MJ, Latkany L, Leung D, Brooks AD, Hochwald SN, Pisters PW et al (1997) A prospective, randomized trial of early enteral feeding after resection of upper gastrointestinal malignancy. Ann Surg 226:567–577
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J et al (2005) International Study Group on Pancreatic Fistula Definition. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138:8–13
Funding
This study is funded by the DFG (Deutsche Forschungsgemeinschaft) and the German Ministry of Research and Education (file reference: 01KG0930)
Conflicts of interest
K. Tadjalli-Mehr is employed as a medical director at Baxter Healthcare and was enrolled for an MSc programme in Medical Biometry/Biostatistics at the Heidelberg University.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00423-011-0773-z
Rights and permissions
About this article
Cite this article
Diener, M.K., Mehr, KT., Wente, M.N. et al. Risk–benefit assessment of closed intra-abdominal drains after pancreatic surgery: a systematic review and meta-analysis assessing the current state of evidence. Langenbecks Arch Surg 396, 41–52 (2011). https://doi.org/10.1007/s00423-010-0716-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-010-0716-0