Abstract
Background and aims
Aim of this study was to define the perioperative risk profile in surgery of patients suffering from Parkinson’s disease (PD) in order to improve treatment options in these patients.
Materials and methods
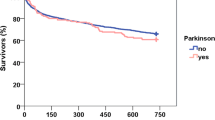
Over a period of 13 years, 51 patients suffering from Parkinson’s disease treated in the departments of general, visceral, thoracic, vascular, and trauma surgery were retrospectively compared using matched-pair analysis with 51 controls not affected by PD. Both groups of patients were assessed regarding morbidity and mortality, length of treatment, and rehabilitation.
Results
Surgical patients suffering from Parkinson’s disease showed an increase in risk of morbidity. Postoperative falls occurred more commonly (entire cohort, p < 0.03). In PD patients treated in the trauma surgery department, postoperative falls (p < 0.04), postoperative stay (p < 0.03), and overall duration of treatment (p < 0.02) were significantly longer than in patients without PD. PD patients of the trauma unit could be discharged home less often for ambulantory rehabilitation after in-patient treatment (p < 0.03).
Conclusions
Concomitant Parkinson’s disease is a significant factor of perioperative morbidity in surgical patients, especially of patients treated in the trauma unit. Perioperative morbidity in PD patients may be influenced by early diagnostic and therapeutic measures.
Similar content being viewed by others
References
Lesnick TG, Papapetropoulos S, Mash DC, Ffrench-Mullen J, Shehadeh L, de Andrade M et al (2007) A genomic pathway approach to a complex disease: axon guidance and Parkinson disease. PLoS Genet 3:1–12 doi:10.1371/journal.pgen.0030098
Lang AE, Lozano AM (1998) Parkinson’s disease: first of two parts. N Engl J Med 339:1036–1053 doi:10.1056/NEJM199810083391504
Lang AE, Lozano AM (1998) Parkinson’s disease: second of two parts. N Engl J Med 339:1130–1143 doi:10.1056/NEJM199810153391607
Betchen SA, Kaplitt M (2003) Future and current surgical therapies in Parkinson’s disease. Curr Opin Neurol 16:487–493 doi:10.1097/00019052-200308000-00008
De Lau LM, Giesbergen PC, de Rijk MC, Hofman A, Koudstaal PJ, Breteler MM (2004) Incidence of parkinsonism and Parkinson disease in a general population: the Rotterdam Study. Neurology 63:1240–1244
Lim E (2005) A walk through the management of Parkinson’s disease. Ann Acad Med Singapore 34:188–195
Bundesinstitut für Bevölkerungsforschung www.bib-demographie.de
Hamrick I, Weiss G, Lippert H, Meyer F (2005) Geriatric problems in the perioperative management of surgical interventions. Zentralbl Chir 130:41–47
Gray H, Wilson S, Sidebottom P (2003) Parkinson’s disease and anaesthesia. Br J Anaesth 90:524 doi:10.1093/bja/aeg549
Easdown LJ, Tessler MJ, Minuk J (1995) Upper airway involvement in Parkinson’s disease resulting in postoperative respiratory failure. Can J Anaesth 42:344–347
Kalenka A, Hinkelbein J (2005) Anaesthesia in patients with Parkinson’s disease. Anaesthesist 54:401–409 doi:10.1007/s00101-005-0840-3
Horner S, Niederkorn K, Ni XS, Fischer R, Fazekas F, Schmidt R et al (1997) Evaluation of cerebrovascular risk factors in Parkinson’s disease. Nervenarzt 68:967–971 doi:10.1007/s001150050224
Jonsson B, Sernbo I, Johnell O (1995) Rehabilitation of hip fracture patients with Parkinson’s Disease. Scand J Rehabil Med 27:227–230
Coughlin L, Templeton J (1980) Hip fractures in patients with Parkinson’s disease. Clin Orthop Relat Res 148:192–195
Mattson JT, Louis DS (1976) Intrapelvic migration of a threaded Steinmann pin in Parkinson’s disease. Clin Orthop Relat Res 121:166–168
Turcotte R, Godin C, Duchesne R, Jodoin A (1990) Hip fractures and Parkinson’s disease. A clinical review of 94 fractures treated surgically. Clin Orthop Relat Res 256:132–136
Gialanella B (2001) Gait in patients with Parkinson’s disease after surgically treated hip fracture. Minerva Med 92:161–166
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mueller, M.C., Jüptner, U., Wuellner, U. et al. Parkinson’s disease influences the perioperative risk profile in surgery. Langenbecks Arch Surg 394, 511–515 (2009). https://doi.org/10.1007/s00423-008-0404-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-008-0404-5