Abstract
Background and aim
At times, the diagnosis of acute appendicitis may be difficult. However, for minimum morbidity to be obtained, early and accurate diagnosis is essential. This study aimed to validate a scoring system proposed by Eskelinen et al. as an aid in making the diagnosis of appendicitis.
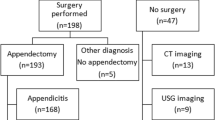
Patients and methods
The prospectively documented data of a consecutive series of 2,359 patients admitted for suspicion of appendicitis were used for validation. Accuracy and positive predictive value were defined as the main overall performance parameters, as was the rate of unnecessary operations to assess changes of patient management. Overall performance was assessed by receiver–operator characteristics (ROC) analysis.
Results
Of 2,359 patients, 662 were proven to have acute appendicitis (prevalence of 28%). The overall sensitivity, specificity, positive and negative predictive value, and accuracy of the score were 0.79, 0.85, 0.68, 0.91 and 0.835 at a cut-off value of 55. Calibration of the score’s cut-off value to 57 yielded more favourable results (0.72, 0.91, 0.76, 0.9 and 0.86), and the rate of unnecessary operations declined from 26.6% to 15.4% (P<0.05, χ2). ROC analysis revealed an area index of 0.91.
Conclusion
The Eskelinen score delivered acceptable clinical results only after calibration to a cut-off value of 57. The data from this study suggest the investigation of whether a calibrated score might be particularly instrumental in the pre-admission evaluation of the patient in whom appendicitis is suspected.

Similar content being viewed by others
References
Alvarado A (1986) A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med 15:577–580
Arnbjörnson E (1985) Scoring systems for computer aided diagnosis of acute appendicitis. Ann Chir Gynaecol 74:159-162
Christian F, Christian GP (1992) A simple scoring system to reduce the negative appendectomy rate. Ann R Coll Surg Engl 74:281–284
Clarke JR, Hayward CZ (1990) A scientific basis for surgical reasoning I. Sensitivity, specificity, prevalence and predictive values. Theor Surg 5:129–132
Clarke JR, Hayward CZ (1990) A scientific basis for surgical reasoning II. Probability revision-odds ratios, likelihood ratios and Bayes’ theorem. Theor Surg 5:206–210
deDombal FT, Staniland JR, Clamp SE (1981) Geographical variation in disease-presentation. Does it constitute a problem and can information science help? Med Decis Making 1:59–61
deDombal FT, de Baere H, van Elk PF, Fingerhut A (1993) Objective medical decision making in acute abdominal pain. In: Beneken JW, Thevenin V (eds) Advances in biomedical engineering. IOS Press, Amsterdam, p 122
Dudley HAF, Paterson Brown S, Thompson JM, Eckersley JR (1989) Prospective scenarios: a method of evaluation of new decision tools. World J Surg 12:277–280
Erikson S (1996) Acute appendicitis—ways to improve diagnostic accuracy. Eur J Surg 162:435–442
Eskelinen M, Ikonen J, Lipponen P (1992) A computer-based diagnostic score to aid in diagnosis of acute appendicitis. Theor Surg 7:86–90
Franke K, Verreet P, Ohmann C, Böhner H, Röher HD (1996) Klinische Standardisierung bei akuten Bauchschmerzen. Langenbecks Arch Chir 381:65–72
Hanley JA, McNeil BJ (1982) The meaning and use of the area under the receiver operating characteristics (ROC) curve. Radiology 143:26–29
Itzbicki JR, Knoefel WT, Wilker DR, Mandelkow HK, Müller K, Siebeck M, Schweiberer L (1992) Accurate diagnosis of acute appendicitis. A retrospective and prospective analysis of 686 patients. Eur J Surg 158:227–231
Jess P, Bierregaard B, Brynitz S, Holst-Christensen J, Kalaja E, Lund-Kristensen J (1981) Acute appendicitis. Prospective trial concerning diagnostic accuracy and complications. Am J Surg 141:232–234
Levelle SM, Kanagaratoam B (1990) The information value of clinical data. Int J Biomed Comput 26:203–209
Lewis FR, Holcroft JW, Boey J, Dunphry JE (1975) Appendicitis. A critical review of diagnosis and treatment in 1000 cases. Arch Surg 110:677–679
MacCartney FJ (1987) Diagnostic logic. BMJ 295:1325–1331
Ohmann C, Kraemer M, Jäger S, Sitter H, Pohl C, Stadelmeyer B, Viettmeier P, Wickers J, Latzke L, Koch B, Thon K (1992) Akuter Bauchschmerz—standardisierte Befunderhebung als Diagnoseunterstützung. Chirurg 63:113–123
Ohmann C, Yang Q, Franke, K and the Abdominal Pain Study Group (1995) Diagnostic scores for acute appendicitis. Eur J Surg 161:273–276
Ohmann C, Franke, K, Yang Q, Margulies M, Röher HD (1995) Diagnosescore für akute Appendizitis. Chirurg 66:135–138
Paterson-Brown S, Vipond MN (1990) Modern aids to clinical decision-making in the acute abdomen. Br J Surg 77:13–18
Pieper R, Kager L, Nösman P (1982) Acute appendicitis. A clinical study of 1018 cases of emergency appendectomy. Acta Chir Scand 148:51–55
Teicher IRA, Landa B, Cohen M, Kabnick LS, Wise L (1993) Scoring system to aid in the diagnosis of appendicitis. Ann Surg 198:753–739
Zielke A, Malewski UA, Lindlar R, Foerster R, Klotter HJ, Rüschoff J, Sitter H, Rothmund M (1991) Sonographie bei Verdacht auf akute Appendizitis. Möglichkeit oder Notwendigkeit für den Chirurgen? Chirurg 62:743–749
Zielke A, Hasse C, Sitter H, Kisker O, Rothmund M (1997) Surgical ultrasound in suspective acute appendicitis. Surg Endosc 11:362–365
Zielke A, Hasse C, Sitter H, Rothmund M (1998) Ultrasound and clinical decision making in acute appendicitis: a prospective study. Eur J Surgery 164:201–209
Acknowledgement
This work was in part supported by a grant from the German Ministry of Education, Science, Research and Technology within the MEDWIS-2-Project on ‘Direkte Entscheidungsunterstützung bei akuten Bauchschmerzen’.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Clinical parameters and their weights by the Eskelinen score
For each of the listed symptoms/signs one or two points are given whenever the respective criterion is fulfilled, then multiplied by the respective factor and added to give a final sum (i.e. score value). The cut-off point (COP) for the diagnosis of acute appendicitis is 55.
Symptom/sign | Criterion, points | Factor |
|---|---|---|
Tenderness | 2 = RLQ, 1 = any other location | 11.41 |
Rigidity | 2 = Yes, 1 = no | 6.62 |
Leucocyte count | 2 = ≥10,000 G/l, 1 = <10,000 G/l | 5.88 |
Rebound tenderness | 2 = Yes, 1 = no | 4.25 |
Pain at presentation | 2 = RLQ, 1 = any other location | 3.51 |
Duration of pain | 2 = <48 h, 1 =≥ 48 h | 2.13 |
where RLQ is right lower abdominal quadrant.
Example (points given in parentheses): a patient of 25 years of age is admitted to the emergency department with abdominal pain of 24-h duration (2×2.13) that was first noticed around the umbilicus but has since moved to the right lower abdominal quadrant (RLQ pain at presentation = 2×3.51). Micturition is reported to be not painful. During physical examination a tenderness in the RLQ is found (2×11.41), with rigidity (2×6.62) and rebound tenderness (2×4.25). The leucocyte count is 15,000 G/l (2×5.58). Total number of points: 67.0. Score diagnosis: acute appendicitis.
Rights and permissions
About this article
Cite this article
Sitter, H., Hoffmann, S., Hassan, I. et al. Diagnostic score in appendicitis. Langenbecks Arch Surg 389, 213–218 (2004). https://doi.org/10.1007/s00423-003-0436-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-003-0436-9