Abstract
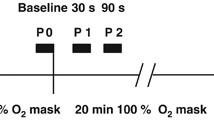
It is commonly believed that during hyperbaric oxygen (HBO) treatment, in spite of the vasoconstriction induced by the increased O2 content in the breathing gas, the elevated carrying capacity of O2 in the arterial blood results in augmented O2 delivery to tissues. The experiments described here tested the hypothesis that HBO treatment would be more efficient in delivering O2 to poorly perfused tissues if the vasoconstriction induced by elevated O2 could be abolished or attenuated by adding CO2 to the breathing gas. Organ blood flow (Q˙ OBF), systemic hemodynamics, and arterial blood gases were measured before, during and after exposure to either 300 kPa O2 (group 1) or 300 kPa O2 with 2 kPa CO2 (group 2), in awake, instrumented rats. During the HBO exposure the respiratory frequency (f b) fell (4 breaths · min−1 · 100 kPa O2 −1), with no changes in arterial CO2 tension (P aCO2), but when CO2 was added, f b and P aCO2 increased. The left ventricular pressure (LVP) and the systolic arterial pressure (SBP) increased. The maximum velocity of LVP (+dP/dt) rose linearly with LVP whether CO2 was added or not (r 2 = 0.72 and 0.75 respectively). Similarly, the cardiac output (Q˙ c) and heart rate (f c) fell, while the stroke volume (SV) was unaltered, independent of P aCO2. There was a general vasoconstriction in most organs in both groups, with the exception of the central nervous system (CNS), eyes, and respiratory muscles. HBO reduced the blood flow to the CNS by 30%, but this vasoconstriction was diminished or eliminated when CO2 was added. In group 2, the blood flow to the CNS rose linearly with increased P aCO2 and decreased pH. After decompression f c and SBP stayed high, while Q˙ c returned to control values by reducing the SV; CNS blood flow remained markedly elevated in group 2, while in group 1, it returned to control levels. We conclude that the changes in f c, Q˙ c, LVP, dP/dt, SBP and most Q˙ OBF values induced by HBO were not changed by hypercapnia. Blood flow to the CNS decreased during HBO treatment at a constant P aCO2. Hypercapnia prevented this decline. Elevated P aCO2 augmented O2 delivery to the CNS and eyes, but increased the susceptibility to O2 poisoning. A prolonged suppression of O2 supply to the CNS occurred during the HBO exposure and in air following the decompression in the absence of CO2. This suppression was offset by the addition of CO2 to the breathing gas.
Similar content being viewed by others
Author information
Authors and Affiliations
Additional information
Accepted: 8 April 1999
Rights and permissions
About this article
Cite this article
Bergø, G., Tyssebotn, I. Cardiovascular effects of hyperbaric oxygen with and without addition of carbon dioxide. Eur J Appl Physiol 80, 264–275 (1999). https://doi.org/10.1007/s004210050592
Issue Date:
DOI: https://doi.org/10.1007/s004210050592