Abstract
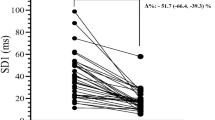
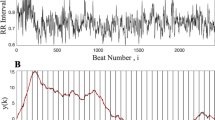
The time necessary to obtain a steady state for an accurate and reliable assessment of resting \( \dot{V}{\text{O}}_{2} \) remains unclear and was the purpose of this study. Thirty healthy men, aged 17–28 years, visited the laboratory twice for the assessment of resting \( \dot{V}{\text{O}}_{2} \), which was assessed as follows: (a) 24 h abstention from physical exercise, alcohol, soft drinks and caffeine, (b) fasting for at least 8 h, (c) an acclimation period of 10 min, and (d) 60 min assessment in a supine position. Resting \( \dot{V}{\text{O}}_{2} \) significantly changed during the 60 min (F = 37.4, P < 0.001), exhibiting a monoexponential decrease before reaching an asymptote. Post hoc pairwise comparisons showed that significant differences existed between consecutive means until the 30 min time point, after which there were no significant differences. The \( \dot{V}{\text{O}}_{2} \) response across trials exhibited high test–retest reliability, with within-subject coefficients of variations at each time point ranging from 2.8 to 7.0 % and intraclass correlation coefficients ranging from 0.90 to 0.99. The reliability was higher from the 25 min time point onwards. Based on these findings, the following recommendations are made to promote accurate assessment of resting \( \dot{V}{\text{O}}_{2} \): (a) initiate the resting \( \dot{V}{\text{O}}_{2} \) measurement with 10 min of acclimation to the assessment apparatus, (b) determine resting \( \dot{V}{\text{O}}_{2} \) for a minimum of 30 min, until an apparent \( \dot{V}{\text{O}}_{2} \) steady state has been achieved; and (c) determine resting \( \dot{V}{\text{O}}_{2} \) for a further 5 min, with the average of this last 5 min of data being regarding as the resting \( \dot{V}{\text{O}}_{2} \).

Similar content being viewed by others
References
ACSM (2009) ACSM’s guidelines for exercise testing and prescription. Lippincott Williams & Wilkins, Baltimore
Berke EM, Gardner AW, Goran MI, Poehlman ET (1992) Resting metabolic rate and the influence of the pretesting environment. Am J Clin Nutr 55:626–629
Bullough RC, Melby CL (1993) Effect of inpatient versus outpatient measurement protocol on resting metabolic rate and respiratory exchange ratio. Ann Nutr Metab 37:24–32
Byard AD, Dengel DR (2002) Validity of a portable metabolic measurement system. Med Sci Sports Exerc 34:S149
Byrne NM, Hills AP, Hunter GR, Weinsier RL, Schutz Y (2005) Metabolic equivalent: one size does not fit all. J Appl Physiol 99:1112–1119
Colberg SR, Swain DP, Vinik AI (2003) Use of heart rate reserve and rating of perceived exertion to prescribe exercise intensity in diabetic autonomic neuropathy. Diabetes Care 26:986–990
Compher C, Frankenfield D, Keim N, Roth-Yousey L (2006) Best practice methods to apply to measurement of resting metabolic rate in adults: a systematic review. J Am Diet Assoc 106:881–903
Cunha FA, Midgley AW, Monteiro WD, Farinatti PT (2010) Influence of cardiopulmonary exercise testing protocol and resting VO(2) assessment on %HR(max), %HRR, %VO(2max) and %VO(2)R relationships. Int J Sports Med 31:319–326
Cunha FA, Midgley AW, Monteiro WD, Campos FK, Farinatti PT (2011) The relationship between oxygen uptake reserve and heart rate reserve is affected by intensity and duration during aerobic exercise at constant work rate. Appl Physiol Nutr Metab 36:839–847
da Cunha FA, Farinatti Pde T, Midgley AW (2011) Methodological and practical application issues in exercise prescription using the heart rate reserve and oxygen uptake reserve methods. J Sci Med Sport 14:46–57
Davenport MH, Charlesworth S, Vanderspank D, Sopper MM, Mottola MF (2008) Development and validation of exercise target heart rate zones for overweight and obese pregnant women. Appl Physiol Nutr Metab 33:984–989
Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP (2011) Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc 43:1334–1359
Gunn SM, Brooks AG, Withers RT, Gore CJ, Owen N, Booth ML, Bauman AE (2002) Determining energy expenditure during some household and garden tasks. Med Sci Sports Exerc 34:895–902
Gunn SM, van der Ploeg GE, Withers RT, Gore CJ, Owen N, Bauman AE, Cormack J (2004) Measurement and prediction of energy expenditure in males during household and garden tasks. Eur J Appl Physiol 91:61–70
Isbell TR, Klesges RC, Meyers AW, Klesges LM (1991) Measurement reliability and reactivity using repeated measurements of resting energy expenditure with a face mask, mouthpiece, and ventilated canopy. JPEN J Parenter Enteral Nutr 15:165–168
Jette M, Sidney K, Blumchen G (1990) Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clin Cardiol 13:555–565
McClave SA, Spain DA, Skolnick JL, Lowen CC, Kieber MJ, Wickerham PS, Vogt JR, Looney SW (2003) Achievement of steady state optimizes results when performing indirect calorimetry. JPEN J Parenter Enteral Nutr 27:16–20
Mezzani A, Corra U, Giordano A, Cafagna M, Adriano EP, Giannuzzi P (2007) Unreliability of the %VO2 reserve versus %heart rate reserve relationship for aerobic effort relative intensity assessment in chronic heart failure patients on or off beta-blocking therapy. Eur J Cardiovasc Prev Rehabil 14:92–98
Olson TP, Tracy JE, Dengel DR (2003) Validity of a low-flow pneumotach and portable metabolic system for measurement of basal metabolic rate. Med Sci Sports Exerc 35:S143
Rotstein A, Meckel Y (2000) Estimation of %VO2 reserve from heart rate during arm exercise and running. Eur J Appl Physiol 83:545–550
Savage PD, Toth MJ, Ades PA (2007) A re-examination of the metabolic equivalent concept in individuals with coronary heart disease. J Cardiopulm Rehabil Prev 27:143–148
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86:420–428
Swain DP (2000) Energy cost calculations for exercise prescription: an update. Sports Med 30:17–22
Swain DP, Leutholtz BC (1997) Heart rate reserve is equivalent to %VO2 reserve, not to %VO2max. Med Sci Sports Exerc 29:410–414
Swain DP, Leutholtz BC, King ME, Haas LA, Branch JD (1998) Relationship between %heart rate reserve and %VO2 reserve in treadmill exercise. Med Sci Sports Exerc 30:318–321
Turley KR, McBride PJ, Wilmore JH (1993) Resting metabolic rate measured after subjects spent the night at home vs at a clinic. Am J Clin Nutr 58:141–144
Wahrlich V, Anjos LA, Going SB, Lohman TG (2006) Validation of the VO2000 calorimeter for measuring resting metabolic rate. Clin Nutr 25:687–692
Weir JB (1949) New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol 109:1–9
Acknowledgments
This study was partially supported by the Carlos Chagas Filho Foundation for the Research Support in Rio de Janeiro (FAPERJ, process E-26/102.545/2010) and by the Brazilian Council for the Research Development (CNPq, process 305729/2006-3).
Conflict of interest
The authors have no conflict of interest that is directly relevant to the content of this paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Klaas R Westerterp.
Rights and permissions
About this article
Cite this article
Cunha, F.A., Midgley, A.W., Monteiro, W. et al. How long does it take to achieve steady state for an accurate assessment of resting \( \dot{\text{V}}{\text{O}}_{2} \) in healthy men?. Eur J Appl Physiol 113, 1441–1447 (2013). https://doi.org/10.1007/s00421-012-2571-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-012-2571-x