Abstract
Activation of the multifunctional Ca2+/calmodulin-dependent protein kinase II (CaMKII) plays a critical role modulating cardiac function in both health and disease. Here, we determined the effect of chronic CaMKII inhibition during an exercise training program in healthy mice. CaMKII was inhibited by KN-93 injections. Mice were randomized to the following groups: sham sedentary, sham exercise, KN-93 sedentary, and KN-93 exercise. Cardiorespiratory function was evaluated by ergospirometry during treadmill running, echocardiography, and cardiomyocyte fractional shortening and calcium handling. The results revealed that KN-93 alone had no effect on exercise capacity or fractional shortening. In sham animals, exercise training increased maximal oxygen uptake by 8% (p < 0.05) compared to a 22% (p < 0.05) increase after exercise in KN-93 treated mice (group difference p < 0.01). In contrast, in vivo fractional shortening evaluated by echocardiography improved after exercise in sham animals only: from 25 to 32% (p < 0.02). In inactive mice, KN-93 reduced rates of diastolic cardiomyocyte re-lengthening (by 25%, p < 0.05) as well as Ca2+ transient decay (by 16%, p < 0.05), whereas no such effect was observed after exercise training. KN-93 blunted exercise training response on cardiomyocyte fractional shortening (63% sham vs. 18% KN-93; p < 0.01 and p < 0.05, respectively). These effects could not be solely explained by the Ca2+ transient amplitude, as KN-93 reduced it by 20% (p < 0.05) and response to exercise training was equal (64% sham and 47% KN-93; both p < 0.01). We concluded that chronic CaMKII inhibition increased time to 50% re-lengthening which were recovered by exercise training, but paradoxically led to a greater increase in maximal oxygen uptake compared to sham mice. Thus, the effect of chronic CaMKII inhibition is multifaceted and of a complex nature.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ubiquitous and multifunctional Ca2+/calmodulin-dependent protein kinase II (CaMKII) regulates a number of intracellular processes related to cellular contractility and nuclear gene expression, thereby controlling the pump function and growth of the heart. Some of the specific targets include the L-type Ca2+ channel, the sarcoplasmic reticulum (SR) Ca2+ release channel (ryanodine receptor 2, RyR2), phospholamban (PLB), Na+ and K+ channels making CaMKII a prominent regulator of excitation–contraction coupling (Couchonnal and Anderson 2008; Hashambhoy et al. 2010; Maier et al. 2007; Maier and Bers 2002). Furthermore, CaMKII can regulate nuclear gene expression on class II histone deacetylase (HDAC), which increases myocyte-enhanced factor 2 (Mef2)-regulated transcription (Erickson and Anderson 2008; Maier and Bers 2002, 2007; Maier et al. 2007; Sag et al. 2009). However, the functional consequences of CaMKII activation are still unclear, since heart failure is associated with increased CaMKII (Anderson 2005; Anderson et al. 1998; Couchonnal and Anderson 2008; Khoo et al. 2006; Vila-Petroff et al. 2007; Zhang et al. 2005); in fact, CaMKII may constitute a molecular switch between cardiac hypertrophy and failure (Zhang et al. 2005), and CaMKII activation may also precede arrhythmic events and contractile dysfunction, mainly because of its effect on the RyR2 (Anderson 2005; Ling et al. 2009; van Oort et al. 2010). On the other hand, improved contractile function after aerobic interval exercise training also associates with activated CaMKII, but in this scenario, the main effect is on the SR Ca2+ uptake due to phosphorylation of PLB. Interestingly, in mice with type-2 diabetes with chronically increased cardiac CaMKII and reduced cardiomyocyte contractile function and Ca2+ handling, aerobic interval exercise training resulted in reduced levels of CaMKII and improved cardiomyocyte contractile function and Ca2+ handling (Stolen et al. 2009). Recent studies have shown that CaMKII negatively regulates calcineurin activity (Khoo et al. 2006; MacDonnell et al. 2009), which in turn regulates mitochondrial respiration, and further complicates the role of CaMKII (Jiang et al. 2010; Wang et al. 2011).
The exact role of CaMKII activation in the heart remains unclear, as it associates with dysfunction, failure, and propensity for arrhythmias, but also with increased function under different circumstances such as exercise training. Based on the potential clinical value of chronic CaMKII inhibition (Khoo et al. 2006; Sag et al. 2009; Zhang et al. 2005) and the beneficial effect of exercise training on delaying cardiac dysfunction and correcting function after onset of heart disease (Stolen et al. 2009; Wisloff et al. 2002, 2007; Adams et al. 2005; Erbs et al. 2010; Mezzani et al. 2008; Hambrecht et al. 2000; Anderson et al. 1998; Kemi et al. 2007; Zhang et al. 2005) two scenarios that may mutually oppose each other, determining the effect of chronic CaMKII inhibition on the response to exercise training would be of considerable interest. Therefore, we aimed to study the effect of chronic CaMKII inhibition during the course of an exercise training program in healthy mice. We hypothesized that chronic CaMKII inhibition would abolish the normal exercise training response in the hearts.
Materials and methods
Mice and CaMKII inhibition
Eighteen female C57 BL/6J mice (Møllegaard Breeding Center, Lille Skensved, Denmark) 18–20 g, 8 weeks of age at inclusion were randomized into four groups: (1) sham control sedentary, (2) sham control exercise training, (3) KN-93 sedentary, and (4) KN-93 exercise training. KN-93 (2-[N-(2-hydroxyethyl)-N-(4 methoxybenzenesulfonyl)]amino-N-(4-chlorocinnamyl)-N-methylbenzylamine; Alexis-Biochemical, Enzo Life Science, PA, USA) diluted in dimethyl sulfoxide (DMSO, Sigma-Aldrich, St. Louis, MO, USA, 2 mg KN-93/1 mL DMSO, 10 μmol/kg (Zhang et al. 2005)) was intraperitoneally injected daily after the exercise training session (for those that exercise trained), throughout the experimental period. In a previous study, Zhang et al. (2005) observed dose-dependent CaMKII inhibition by KN-93, in which daily injections of 10 μmol/kg KN-93 produced similar effect on left ventricular contraction measurements as the genetically CaMKII-inhibited AC3:I mice (Zhang et al. 2005; Khoo et al. 2006). Sham control mice received similar amounts of DMSO daily. The Norwegian council for Animal Research approved the study, which was in accordance with the Guide for the Care and Use of Laboratory Animals (National Institutes of Health Publications No. 85–23, revised 1996).
Exercise training
Exercise training was performed as aerobic interval training for 6 weeks, 5 days/week, on an inclined (25°) treadmill, each session starting with a 10-min warm-up at 50–60% of maximal oxygen uptake (VO2max), whereupon exercise then alternated between 4- and 2-min intervals at 85–90 and 50–60% of VO2max, respectively for 60 min. VO2max was assessed during a treadmill running test to exhaustion in a metabolic chamber. After a warm-up period of about 10 min, treadmill band velocity was increased by 0.03 m/s for every second minute until mice were not able to maintain the treadmill velocity (Hoydal et al. 2007; Kemi et al. 2002). To maintain the exercise intensity throughout the experimental period, VO2max was tested at the beginning of each week in addition to pre- and post-tests. This exercise protocol has previously been proven efficient for inducing exercise and cardiovascular adaptations in both the clinical and experimental studies (Tjonna et al. 2008; Hoydal et al. 2007; Kemi et al. 2002, 2005; Wisloff et al. 2001; Stolen et al. 2009).
Echocardiography
High-resolution echocardiography (Vevo 770, VisualSonics, Toronto, Canada) using a single-element mechanical transducer with a center frequency of 30 MHz was performed on self-breathing mice exposed to a mixture of 2% isoflurane and 98% oxygen. A two-dimensional long-axis view was used to visualize both ventricles, the ascending aorta, and the right ventricular outflow tract by placing the ultrasound transducer on the left parasternal position, whereas a short-axis view was used to visualize systolic and diastolic movement of both ventricles by placing the transducer horizontally above the heart. Left ventricular end-diastolic diameter (LVEDD), left ventricular end-systolic diameter (LVESD), interventricular septum (IVST) and posterior wall thickness (PWT) were recorded with M-mode echocardiography, which allowed calculation of the fractional shortening (% = [(LVEDD − LVESD)/LVEDD] × [100]) as an index of systolic left ventricular function. The following equation was used to calculate LV mass (mg) = [(LVEDD + IVST + PWT)3 − LVEDD3] × 1.055, where 1.055 (mg/mm3) is the density of myocardium. IVST and PWT were measured at end diastole.
Cardiomyocyte isolation, contractile function, Ca2+ measurements and cell size
Left ventricular cardiomyocytes were isolated as previously described using a Hepes-based solution (Mitra and Morad 1981; Guatimosim et al. 2001). Exercised hearts were excised 24 h after the last exercise session. A mixture of 3–4% isoflurane and 96–97% oxygen were used to anesthetize the mice, whereupon the heart was heparinized and removed. Until it was connected to the aortic cannula on a standard Langendorff retrograde perfusion system, the hearts were kept on ice cold Hepes solution. The hearts were cleaned with a Hepes solution containing EGTA (Sigma-Aldrich Corp., Missouri, USA) before the perfusion was switched to Hepes solution with collagenase (Worthington, Lakewood, USA), and perfusion was continued for approximately 10 min (3.5 ml/min). After the hearts were taken down, left ventricles were carefully cut off and gently shaken for 2 min before the non-digested tissue was filtered out (nylon mesh, 250 μm). Further, cells were stepwise exposed to increasing Ca2+ levels (initially 0.05 mM). The isolated cells were centrifuged (30 s, 600 rpm) before solution was switched to 1.2 mM Hepes-based solution. Fura-2/AM-loaded (2 μmol/l, Molecular Probes, Eugene, OR, USA) cardiomyocytes were field stimulated by bipolar electrical pulse at 1 Hz, on an inverted epifluorescence microscope (Nikon TE-2000E, Tokyo, Japan), whereupon cell shortening was recorded by video-based myocyte sarcomere spacing (SarcLen™, IonOptix, Milton, MA, USA) and intracellular Ca2+ concentration was measured by fluorescence after excitation by alternating 340 and 380 nm wavelengths (F 340/380 ratio) (Optoscan, Cairn Research, Kent, UK). Cells with a clear visual intracellular structure that were able to follow stimulation frequency were included for the experiment. The total number of cardiomyocytes included for all analysis in the different groups was: sham sedentary 8, sham exercise 20, KN-93 sedentary 5, and in KN-93 exercise 9. During the stimulation protocol, cells were kept in 1.2 mM Ca2+ HEPES-based solution at 37°C. Cell size was measured with Nikon Eclipse E400 Microscope with a DSFil camera (Nikon NIS-Elements Basic Research Version 3.00 software, Nikon Instruments Inc., Melville, NY, USA). Cardiomyocyte size was measured on 80–120 cardiomyocytes per group.
Statistics
A one-way ANOVA with LSD post hoc test was used to detect significant differences between groups. For within-group differences from pre- to post-test, a paired sample T test was used. Statistical significance level was set to p < 0.05.
Results
VO2max and exercise capacity
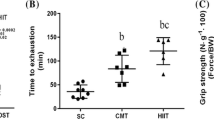
In sedentary mice, daily intraperitoneal injections of the CaMKII-selective inhibitor KN-93 did not affect VO2max, running speed at VO2max, or body mass (Fig. 1). However, while chronic CaMKII inhibition had no effect in sedentary mice, it did affect the response to exercise training. Whereas exercise training increased VO2max by 8% (p < 0.05) in sham, the effect was 22% (p < 0.01) in KN-93 mice after the exercise training period (magnitude of response difference p < 0.01, Fig. 1a). KN-93 tended to suppress the growth in body mass (Fig. 1c), which made it necessary to normalize VO2max according to correct scaling procedures, which involves the correct normalization of a physiological variable (here VO2max) to a body dimension (here body mass). It is well established that cardiorespiratory capacity in lighter individuals will be overestimated compared to heavier ones when VO2max is expressed in direct relation to body mass (i.e., ml/kg/min) and that VO2max should be expressed with body mass raised to the power of 0.75 (i.e., ml/kg0.75/min) when comparing individuals that differ in body mass (Taylor et al. 1981). Hence, VO2max was divided by body mass raised to the power of 0.75 as an exponent in the present study in order not to overestimate the effect of KN-93 on VO2max. In line with a larger increase in VO2max after exercise training in KN-93 mice, we observed that running speed at VO2max also increased twice as much compared to that observed in sham mice 32% (p < 0.01), and 61% (p < 0.01) in KN-93 mice.
Cardiac remodeling
KN-93 injections did not significantly change LVEDD, LVESD, PWT, or IVST (Table 1). However, there was a trend for decreased LV mass, and LVEDD in sedentary KN-93 treated mice compared to sham sedentary.
Also, CaMKII inhibition by KN-93 injections did not affect cardiomyocyte size in sedentary mice, measured as cell length and width in isolated cardiomyocytes, but it did blunt the exercise training-induced hypertrophy of the cardiomyocytes. Exercise-induced cardiomyocyte hypertrophy was observed in both sham and KN-93 mice, but the effect was larger in sham mice. Exercise training increased cardiomyocyte length and width by 13% (p < 0.05) and 30% (p < 0.05) in sham mice, and by 8% (p < 0.05) and 14% (p < 0.05) in KN-93 mice, respectively (group differences p < 0.05, Fig. 2a, b). Thus, the cardiomyocyte hypertrophy response to exercise in KN-93 mice was approximately half of that in sham mice.
Cardiac contractile function
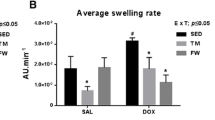
According to the measurements of in vivo cardiac function with echocardiography, KN-93 injections did not significantly affect heart rate, stroke volume (SV), cardiac output or fractional shortening (Table 1; Fig. 3). In contrast to VO2max and exercise capacity, left ventricular fractional shortening improved from 25 to 32% after exercise training in sham mice (28% training response, p < 0.02). Cardiac contractile function is largely dependent on Ca2+ handling properties. Systolic Ca2+ and diastolic Ca2+ level were significantly increased by KN-93 injections (Fig. 4a, b, p < 0.01). Only sham exercise increased systolic Ca2+ levels (Fig. 4a, p < 0.05), and decreased diastolic Ca2+ level (Fig. 4b, p < 0.01).
Cardiomyocyte systolic Ca2+ level (a), diastolic Ca2+ level (b), time to 50% diastolic re-lengthening (c), Ca2+ transient decay time (d), intracellular Ca2+ transient amplitude (e), and fractional shortening (f), presented as mean values ± SD. *p < 0.05 versus sedentary; **p < 0.01 versus sedentary; # p < 0.05 versus KN-93 exercise; ## p < 0.01 versus KN-93 exercise; § p < 0.05 versus sham sedentary; §§ p < 0.01 versus sham sedentary
Chronic CaMKII inhibition by KN-93 injections induced a reduction of the cardiomyocyte ability to re-lengthen (25% increased time to 50% re-lengthening; Fig. 4c, p < 0.05) after twitch contractions. This was at least partly explained by the 16% increase in the Ca2+ transient decay time (Fig. 4d, p < 0.05). Exercise training normalized cardiomyocyte re-lengthening and Ca2+ transient decay times to levels comparable to sedentary sham mice, and the response to exercise training was not different between sham and KN-93 mice. In particular, exercise training decreased the re-lengthening time by 12% (p < 0.05) and 16% (p < 0.05) in sham and KN-93 mice, respectively, which was linked to comparable exercise training-induced changes in the Ca2+ transient decay times (Fig. 4c, d).
In contrast to the above, the observed effects of KN-93 and exercise training on cardiomyocyte fractional shortening (amplitude of the contraction) and the associated Ca2+ transient amplitude showed a more complex nature. First, KN-93 reduced the Ca2+ transient amplitude by 20% (Fig. 4e, p < 0.05), but this did not translate into a comparable reduction in the fractional shortening, as no effect was observed. Second, fractional shortening improved by exercise training, but the response was blunted in KN-93 mice compared to sham mice. Exercise training in sham mice increased fractional shortening by 63% (p < 0.01), but only by 18% (p < 0.05) in KN-93 mice (magnitude of response difference p < 0.05, Fig. 4f). This could not be solely explained by changes to the Ca2+ transient amplitude, as the exercise training response did not differ between sham and KN-93 mice; sham increased by 64% (p < 0.01), and KN-93 by 47% (p < 0.01) in response to exercise training (Fig. 4e). Table 2 provides an overview of the effects of CaMKII inhibition on whole-body and cardiac, and cardiomyocyte exercise training response.
Discussion
Given that (1) experimental trials (Anderson 2005; Zhang et al. 2005; Grimm and Brown 2010) have raised the possibility that systemic CaMKII inhibition may be a viable and effective strategy for the treatment of heart disease, and (2) exercise training in both experimental (Rose et al. 2007; Wisloff et al. 2002; Stolen et al. 2009) and clinical (Adams et al. 2005; Erbs et al. 2010; Hambrecht et al. 2000; Mezzani et al. 2008; Wisloff et al. 2007) trials show improved heart function in similar scenarios of heart disease, we aimed to test the potential value of combining those strategies; first in normal healthy mice. The reasoning for the latter is that exercise training and CaMKII also interact in the heart, as the inotropic effects of exercise training are at least partly modulated by an exercise training-induced increase in CaMKII activity (Kemi et al. 2007). This complicates the combination scenario as CaMKII seems to act as a two edged sword. In fact, CaMKII contributes to decompensate pathologic hypertrophy to heart failure, mainly by its action on the RyR2 to increase SR Ca2+ leak (Sag et al. 2009; Ling et al. 2009). Thus, the possibility arises that chronic CaMKII inhibition and exercise training may oppose each other, though it remains to be studied.
As such, this is the first study to introduce the combination of chronic CaMKII inhibition by daily KN-93 injections and aerobic interval exercise training. The main finding was that chronic CaMKII inhibition blunted several aspects of the response patterns of cardiomyocyte contractility, and intracellular Ca2+ handling to exercise training, but it did not fully prevent such adaptations. Moreover, CaMKII inhibition also enhanced exercise training-induced improvements on VO2max and aerobic exercise capacity, whereas it did not affect either of them in sedentary mice.
Mechanisms of exercise training-induced adaptation
The present study provides several mechanistic clues as to the response to exercise training. First, it shows that while CaMKII activation contributes to the cardiac improvements after exercise training (Kemi et al. 2007), other mechanisms must also contribute, as CaMKII inhibition only partly blunted the exercise response. Whether those mechanisms naturally co-exist or occur to compensate for the loss of CaMKII activation remains unknown.
Second, the finding that VO2max and exercise capacity responded more to exercise training in the presence of the chronic CaMKII inhibition compared to the absence thereof indicates that CaMKII also may negatively regulate exercise adaptation in peripheral organs. While this requires further investigation, it is plausible all the while it is ubiquitous and exists in most, if not all, cellular systems (Hudmon and Schulman 2002; Chin 2004).
Third, the opposite effects of exercise training on VO2max and exercise capacity on the one side, and cardiac inotropy and hypertrophy on the other side in the face of CaMKII inhibition highlights that other organs are important in determining VO2max (Bassett and Howley 2000; Coffey and Hawley 2007). In particular, chronic exercise training elicits resistance to muscle fatigue through metabolic responses including mitochondrial biogenesis, increased oxidative capacity, and alterations in gene and protein expression that ultimately leads to phenotype changes that support endurance-type activity (Rose et al. 2007; Benziane et al. 2008; Chin 2004; Coffey and Hawley 2007; Bassett and Howley 2000). The exact mechanism of this rather surprising observation is not known; however, the interaction between CaMKII and calcineurin is a possible candidate. CaMKII modulation of calcineurin signaling is released by CaMKII inhibition. Calcineruin modulates exercise-induced skeletal muscle phenotypes and enhances exercise capacity through increase in mitochondrial oxidative function and energy substrate storage in skeletal muscles (Wang et al. 2011; Jiang et al. 2010). This should be elucidated in future studies.
Cardiac contractile capacity, Ca2+ handling, and CaMKII
Both in vivo and cellular fractional shortening were unaffected by KN-93-induced inhibition of CaMKII in sedentary mice, whereas the expected training-induced increase in both whole-heart and cellular fractional shortening was blunted by the chronic KN-93 treatment. However, chronic CaMKII inhibition did reduce the rate of diastolic cellular relaxation in sedentary mice, which was explained by slower intracellular Ca2+ removal (longer time to 50% Ca2+ transient decay) and higher systolic Ca2+ levels. Exercise training normalized Ca2+ removal times, and in contrast to fractional shortening, the effect was not blunted by CaMKII inhibition. These results are in accordance with Kemi et al. (2007), who found that acute pre-incubation, with AIP (comparable CaMKII inhibitor) in isolated cardiomyocytes also blunted the exercise training-induced improvements in cellular contractility. Together, these results suggest that CaMKII at least partly modulates the exercise training-induced improvements in cardiac contractility, excitation–contraction coupling, and intracellular Ca2+ handling (Kemi et al. 2007; Stolen et al. 2009). The accumulated evidence also suggests that this modulation occurs via targeting of several loci of excitation–contraction coupling and Ca2+ handling (Stolen et al. 2009). Indeed, fractional shortening is dependent on both SR Ca2+ release and myofilaments Ca2+ sensitivity, where the latter may explain the dissociation between fractional shortening and the intracellular Ca2+ transient amplitude in the present study, as shown directly by others after exercise training (de Waard et al. 2007; Diffee et al. 2001). However, in our experiments we used unloaded myocytes where tension development and basal sarcomere length were not considered.
Current results together with the previous studies (Anderson 2005; Anderson et al. 1998; Couchonnal and Anderson 2008; Erickson and Anderson 2008; Kemi et al. 2007; Khoo et al. 2006; Maier and Bers 2002; Maier et al. 2007; Sag et al. 2009; Vila-Petroff et al. 2007; Zhang et al. 2005) suggest that CaMKII is a versatile kinase that may shift cardiac function into different and also opposite phenotypes. In healthy mice, it appears that a controlled increase in the CaMKII activity increases cardiac contraction (Kemi et al. 2007); that CaMKII inhibition reduces cardiac contraction, and that these effects mainly occur because CaMKII inhibition reduces SR Ca2+ uptake via SERCA2a. Therefore, it is also possible that the depression of cardiomyocyte contractile parameters by chronic CaMKII inhibition observed here might have progressed to a global dysfunction and a failure if CaMKII inhibition was continued. As such, maintained CaMKII seems to be important for normal cardiomyocyte function in healthy mice. In contrast, the cardiac dysfunction that also has been linked to increased CaMKII activity (Ai et al. 2005; Couchonnal and Anderson 2008; Maier et al. 2007; Zhang and Brown 2004) has mainly been attributed to hypersensitization of the RyR2 to luminal Ca2+ with subsequent diastolic SR Ca2+ leak and a shift of Ca2+ out of the cell; a scenario that may lead to contractile dysfunction and increased propensity for arrhythmic events (Sag et al. 2009; Ai et al. 2005; Grimm and Brown 2010; Khoo et al. 2006; Ling et al. 2009; Stolen et al. 2009; Wu et al. 2002), in which CaMKII inhibition or reduction would become particularly beneficial (Kemi et al. 2007; Laurita and Rosenbaum 2008; Li et al. 2006; Vila-Petroff et al. 2007; Yang et al. 2006; Zhang et al. 2005). In a recent modulation study, Hashambhoy et al. (2010) report that inhibition of CaMKII phosphorylation of the L-type Ca2+ channel rather than the RyR2 is more effective in modulating diastolic RyR2 flux. Thus, a pharmacological approach of CaMKII inhibition in the heart should also target the L-type Ca2+ channel in order to prevent or treat cardiac dysfunction and disease. Whether this will be feasible remains to be investigated. KN-93 inhibits CaMKII by competing for the calmodulin binding site, and has been widely used to implicate roles of CaMKII in Ca2+ handling (Sumi et al. 1991). KN-93 is not heart-specific and is known to have other actions than CaMKII inhibition (Anderson et al. 1998; Gao et al. 2006). Previous studies have observed that KN-93 might inhibit L-type Ca2+ current independent of CaMKII (Anderson et al. 1998; Gao et al. 2006). This negative effect of KN-93 on intracellular Ca2+ levels are balanced by inhibition of voltage-dependent potassium currents which enhance Ca2+ entry via L-type Ca2+ channel (Anderson et al. 1998; Rezazadeh et al. 2006; Ledoux et al. 1999). The lack of organ specificity of KN-93 is a limitation of this study, and interpretations should be considered with caution. We did, however, control for non-cardiac side effects of chronic KN-93 injections by the pathological examinations of the vital organs after euthanasia in mice.
Physiological hypertrophy
Echocardiography measurements observed a trend for decreased LV mass in sedentary KN-93 treated mice, which was normalized by exercise-induced hypertrophy, and cardiomyocyte length and width increased significantly less in KN-93-treated mice compared to sham-treated mice. These results are somewhat similar to the observations of Zhang et al. (2005), with myocardial infarction as the physiological stressor, who reported that cardiomyocyte transverse cross-sectional area and heart weight were comparably smaller after genetic inhibition of CaMKII than in control cardiomyocytes. Furthermore, Ramirez et al. (1997) reported that pre-treatment with KN-93 blocked hypertrophic responses to the hypertrophy developed by pressure overload or endothelin-1 (Zhang et al. 2004; Zhu et al. 2000). Our observation suggests that CaMKII may also modulate cardiomyocyte growth in response to exercise training (physiological hypertrophy) and not only in response to the pathologic conditions.
Conclusion
This study indicates the importance of maintaining normal CaMKII activity in cardiomyocytes of healthy individuals, also because it positively modulates inotropic/lusitropic responses to exercise training. However, targeting CaMKII by selective inhibitors has recently been suggested to correct cardiac dysfunction and prevent decompensation and progression of heart disease; a clinical scenario that also is targeted by exercise training. This study indicates that a combination strategy of CaMKII inhibition and exercise training may be feasible for the purpose of attenuating heart disease, although this does present a complex scenario that may also reduce some of the beneficial effects of exercise training, especially if CaMKII inhibitors cannot be closely tuned into localized subcellular targets that mainly cause the cardiac dysfunction.
Limitations
The small molecule inhibitor KN-93 has potential non-specific effects other than CaMKII inhibition which were not controlled for; this is a limitation of the present study. The pathological examinations were done to rule out effects on the results from any of the other vital organs due to KN-93 or DMSO injections.
References
Adams V, Linke A, Krankel N, Erbs S, Gielen S, Mobius-Winkler S, Gummert JF, Mohr FW, Schuler G, Hambrecht R (2005) Impact of regular physical activity on the NAD(P)H oxidase and angiotensin receptor system in patients with coronary artery disease. Circulation 111(5):555–562. doi:10.1161/01.CIR.0000154560.88933.7E
Ai X, Curran JW, Shannon TR, Bers DM, Pogwizd SM (2005) Ca2+/calmodulin-dependent protein kinase modulates cardiac ryanodine receptor phosphorylation and sarcoplasmic reticulum Ca2+ leak in heart failure. Circ Res 97(12):1314–1322. doi:10.1161/01.RES.0000194329.41863.89
Anderson ME (2005) Calmodulin kinase signaling in heart: an intriguing candidate target for therapy of myocardial dysfunction and arrhythmias. Pharmacol Ther 106(1):39–55. doi:10.1016/j.pharmthera.2004.11.002
Anderson ME, Braun AP, Wu Y, Lu T, Schulman H, Sung RJ (1998) KN-93, an inhibitor of multifunctional Ca++/calmodulin-dependent protein kinase, decreases early after depolarizations in rabbit heart. J Pharmacol Exp Ther 287(3):996–1006
Bassett DR Jr, Howley ET (2000) Limiting factors for maximum oxygen uptake and determinants of endurance performance. Med Sci Sports Exerc 32(1):70–84
Benziane B, Burton TJ, Scanlan B, Galuska D, Canny BJ, Chibalin AV, Zierath JR, Stepto NK (2008) Divergent cell signaling after short-term intensified endurance training in human skeletal muscle. Am J Physiol Endocrinol Metab 295(6):E1427–E1438. doi:10.1152/ajpendo.90428.2008
Chin ER (2004) The role of calcium and calcium/calmodulin-dependent kinases in skeletal muscle plasticity and mitochondrial biogenesis. Proc Nutr Soc 63(2):279–286. pii:10.1079/PNS2004335S0029665104000370
Coffey VG, Hawley JA (2007) The molecular bases of training adaptation. Sports Med 37(9):737–763
Couchonnal LF, Anderson ME (2008) The role of calmodulin kinase II in myocardial physiology and disease. Physiology 23:151–159. doi:10.1152/physiol.00043.2007
de Waard MC, van der Velden J, Bito V, Ozdemir S, Biesmans L, Boontje NM, Dekkers DHW, Schoonderwoerd K, Schuurbiers HCH, de Crom R, Stienen GJM, Sipido KR, Lamers JMJ, Duncker DJ (2007) Early exercise training normalizes myofilament function and attenuates left ventricular pump dysfunction in mice with a large myocardial infarction. Circ Res 100(7):1079–1088. doi:10.1161/01.Res.0000262655.16373.37
Diffee GM, Seversen EA, Titus MM (2001) Exercise training increases the Ca2+ sensitivity of tension in rat cardiac myocytes. J Appl Physiol 91:309–315
Erbs S, Hollriegel R, Linke A, Beck EB, Adams V, Gielen S, Mobius-Winkler S, Sandri M, Krankel N, Hambrecht R, Schuler G (2010) Exercise training in patients with advanced chronic heart failure (NYHA IIIb) promotes restoration of peripheral vasomotor function, induction of endogenous regeneration, and improvement of left ventricular function. Circ Heart Fail 3(4):486–494. doi:10.1161/CIRCHEARTFAILURE.109.868992
Erickson JR, Anderson ME (2008) CaMKII and its role in cardiac arrhythmia. J Cardiovasc Electrophysiol 19(12):1332–1336. doi:10.1111/j.1540-8167.2008.01295.x
Gao L, Blair LAC, Marshall J (2006) CaMKII-independent effects of KN93 and its inactive analog KN92: reversible inhibition of L-type calcium channels. Biochem Biophys Res Commun 345:1606–1610
Grimm M, Brown JH (2010) Beta-adrenergic receptor signaling in the heart: role of CaMKII. J Mol Cell Cardiol 48(2):322–330. doi:10.1016/j.yjmcc.2009.10.016
Guatimosim S, Sobie EA, Cruz JDS, Martin LA, Lederer WJ (2001) Molecular identification of a TTX-sensitive Ca2+ current. Am J Physiol Cell Physiol 280:1327–1339
Hambrecht R, Wolf A, Gielen S, Linke A, Hofer J, Erbs S, Schoene N, Schuler G (2000) Effect of exercise on coronary endothelial function in patients with coronary artery disease. N Engl J Med 342(7):454–460. doi:10.1056/NEJM200002173420702
Hashambhoy YL, Greenstein JL, Winslow RL (2010) Role of CaMKII in RyR leak, EC coupling and action potential duration: a computational model. J Mol Cell Cardiol. doi:10.1016/j.yjmcc.2010.1007.1011
Hoydal MA, Wisloff U, Kemi OJ, Ellingsen O (2007) Running speed and maximal oxygen uptake in rats and mice: practical implications for exercise training. Eur J Cardiovasc Prev Rehabil 14(6):753–760. doi:10.1097/HJR.0b013e3281eacef1
Hudmon A, Schulman H (2002) Structure-function of the multifunctional Ca2+/calmodulin-dependent protein kinase II. Biochem J 364:593–611
Jiang LQ, Garcia-Roves PM, de Castro Barbosa T, Zierath JR (2010) Constitutively active calcineurin in skeletal muscle increases endurance performance and mitochondrial respiratory capacity. Am J Physiol Endocrinol Metab 298(1):E8–E16. doi:10.1152/ajpendo.00403.2009
Kemi OJ, Loennechen JP, Wisloff U, Ellingsen O (2002) Intensity-controlled treadmill running in mice: cardiac and skeletal muscle hypertrophy. J Appl Physiol 93(4):1301–1309. doi:10.1152/japplphysiol.00231.2002
Kemi OJ, Haram PM, Loennechen JP, Osnes JB, Skomedal T, Wisloff U, Ellingsen O (2005) Moderate vs. high exercise intensity: differential effects on aerobic fitness, cardiomyocyte contractility, and endothelial function. Cardiovasc Res 67 (1):161–172. doi:10.1016/j.cardiores.2005.03.010
Kemi OJ, Ellingsen O, Ceci M, Grimaldi S, Smith GL, Condorelli G, Wisloff U (2007) Aerobic interval training enhances cardiomyocyte contractility and Ca2+ cycling by phosphorylation of CaMKII and Thr-17 of phospholamban. J Mol Cell Cardiol 43(3):354–361. doi:10.1016/j.yjmcc.2007.06.013
Khoo MS, Li J, Singh MV, Yang Y, Kannankeril P, Wu Y, Grueter CE, Guan X, Oddis CV, Zhang R, Mendes L, Ni G, Madu EC, Yang J, Bass M, Gomez RJ, Wadzinski BE, Olson EN, Colbran RJ, Anderson ME (2006) Death, cardiac dysfunction, and arrhythmias are increased by calmodulin kinase II in calcineurin cardiomyopathy. Circulation 114(13):1352–1359. doi:10.1161/CIRCULATIONAHA.106.644583
Laurita KR, Rosenbaum DS (2008) Mechanisms and potential therapeutic targets for ventricular arrhythmias associated with impaired cardiac calcium cycling. J Mol Cell Cardiol 44(1):31–43. doi:10.1016/j.yjmcc.2007.10.012
Ledoux J, Chartier D, Leblanc N (1999) Inhibitors of calmodulin-dependent protein kinase are nonspecific blockers of voltage-dependent K+ channels in vascular myocytes. J Pharmacol Exp Ther 290(3):1165–1174
Li J, Marionneau C, Zhang R, Shah V, Hell JW, Nerbonne JM, Anderson ME (2006) Calmodulin kinase II inhibition shortens action potential duration by upregulation of K+ currents. Circ Res 99(10):1092–1099. doi:10.1161/01.RES.0000249369.71709.5c
Ling H, Zhang T, Pereira L, Means CK, Cheng H, Gu Y, Dalton ND, Peteron KL, Chen J, Bers D, Brown JH (2009) Requirement for Ca2+/calmodulin-dependent kinase II in the transition from pressure overload-induced cardiac hypertrophy to heart failure in mice. J Clin Invest 119:1230–1240
MacDonnell SM, Weisser-Thomas J, Kubo H, Hanscome M, Liu Q, Jaleel N, Berretta R, Chen X, Brown JH, Sabri AK, Molkentin JD, Houser SR (2009) CaMKII negatively regulates calcineurin-NFAT signaling in cardiac myocytes. Circ Res 105(4):316–325. doi:10.1161/CIRCRESAHA.109.194035
Maier LS, Bers DM (2002) Calcium, calmodulin, and calcium-calmodulin kinase II: heartbeat to heartbeat and beyond. J Mol Cell Cardiol 34(8):919–939. pii:S0022282802920389
Maier LS, Bers DM (2007) Role of Ca2+/calmodulin-dependent protein kinase (CaMK) in excitation–contraction coupling in the heart. Cardiovasc Res 73:631–640
Maier LS, Bers DM, Brown JH (2007) Calmodulin and Ca2+/calmodulin kinases in the heart—physiology and pathophysiology. Cardiovasc Res 73(4):629–630. doi:10.1016/j.cardiores.2007.01.005
Mezzani A, Corra U, Giannuzzi P (2008) Central adaptations to exercise training in patients with chronic heart failure. Heart Fail Rev 13(1):13–20. doi:10.1007/s10741-007-9053-y
Mitra R, Morad M (1981) A uniform enzymatic method for dissociation of myocytes from hearts and stomachs of vertebrates. Pflugers Arch 391:85–100
Ramirez MT, Zhao X, Schulman H, Brown JH (1997) The nuclear deltaB isoform of Ca2+/Calmodulin-dependent protein kinase II regulated atrial natriuretic factor gene expression in ventricular myocytes. J Biol Chem 272:31203–31208
Rezazadeh S, Claydon TW, Fedida D (2006) KN-93 (2-[N-(2-hydroxyethyl)]-N-(4-methoxybenzenesulfonyl)]amino-N-(4-chlorocinn amyl)-N-methylbenzylamine), a calcium/calmodulin-dependent protein kinase II inhibitor, is a direct extracellular blocker of voltage-gated potassium channels. J Pharmacol Exp Ther 317(1):292–299. doi:10.1124/jpet.105.097618
Rose AJ, Frosig C, Kiens B, Wojtaszewski JF, Richter EA (2007) Effect of endurance exercise training on Ca2+ calmodulin-dependent protein kinase II expression and signalling in skeletal muscle of humans. J Physiol 583(Pt 2):785–795. doi:10.1113/jphysiol.2007.138529
Sag CM, Wadsack DP, Khabbazzadeh S, Abesser M, Grefe C, Neumann K, Opiela MK, Backs J, Olson EN, Brown JH, Neef S, Maier SK, Maier LS (2009) Calcium/calmodulin-dependent protein kinase II contributes to cardiac arrhythmogenesis in heart failure. Circ Heart Fail 2(6):664–675. doi:10.1161/CIRCHEARTFAILURE.109.865279
Stolen TO, Hoydal MA, Kemi OJ, Catalucci D, Ceci M, Aasum E, Larsen T, Rolim N, Condorelli G, Smith GL, Wisloff U (2009) Interval training normalizes cardiomyocyte function, diastolic Ca2+ control, and SR Ca2+ release synchronicity in a mouse model of diabetic cardiomyopathy. Circ Res 105(6):527–536. doi:10.1161/CIRCRESAHA.109.199810
Sumi MKK, Ishikawa T, Ishii A, Hagiwara M, Nagatsu T, Hidaka H (1991) The newly synthesized selective Ca2+/calmodulin dependent protein kinase II inhibitor KN-93 reduces dopamine contents in PC12h cells. Biochem Biophys Res Commun 181:968–975
Taylor CR, Maloiy GM, Weibel ER, Langman VA, Kamau JM, Seeherman HJ, Heglund NC (1981) Design of the mammalian respiratory system. III Scaling maximum aerobic capacity to body mass: wild and domestic mammals. Respir Physiol 44 (1):25–37
Tjonna AE, Lee SJ, Rognmo O, Stolen TO, Bye A, Haram PM, Loennechen JP, Al-Share QY, Skogvoll E, Slordahl SA, Kemi OJ, Najjar SM, Wisloff U (2008) Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: a pilot study. Circulation 118(4):346–354. doi:10.1161/CIRCULATIONAHA.108.772822
van Oort RJ, McCauley MD, Dixit SS, Pereira L, Yang Y, Respress JL, Wang Q, De Almeida AC, Skapura DG, Anderson ME, Bers DM, Wehrens XH (2010) Ryanodine receptor phosphorylation by calcium/calmodulin-dependent protein kinase II promotes life-threatening ventricular arrhythmias in mice with heart failure. Circulation 122(25):2669–2679. doi:10.1161/CIRCULATIONAHA.110.982298
Vila-Petroff M, Salas MA, Said M, Valverde CA, Sapia L, Portiansky E, Hajjar RJ, Kranias EG, Mundina-Weilenmann C, Mattiazzi A (2007) CaMKII inhibition protects against necrosis and apoptosis in irreversible ischemia-reperfusion injury. Cardiovasc Res 73(4):689–698. doi:10.1016/j.cardiores.2006.12.003
Wang JX, Jiao JQ, Li Q, Long B, Wang K, Liu JP, Li YR, Li PF (2011) miR-499 regulates mitochondrial dynamics by targeting calcineurin and dynamin-related protein-1. Nat Med 17(1):71–78. doi:10.1038/nm.2282
Wisloff U, Helgerud J, Kemi OJ, Ellingsen O (2001) Intensity-controlled treadmill running in rats: VO(2 max) and cardiac hypertrophy. Am J Physiol Heart Circ Physiol 280(3):H1301–H1310
Wisloff U, Loennechen JP, Currie S, Smith GL, Ellingsen O (2002) Aerobic exercise reduces cardiomyocyte hypertrophy and increases contractility, Ca2+ sensitivity and SERCA-2 in rat after myocardial infarction. Cardiovasc Res 54(1):162–174. pii:S000863630100565X
Wisloff U, Stoylen A, Loennechen JP, Bruvold M, Rognmo O, Haram PM, Tjonna AE, Helgerud J, Slordahl SA, Lee SJ, Videm V, Bye A, Smith GL, Najjar SM, Ellingsen O, Skjaerpe T (2007) Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation 115(24):3086–3094. doi:10.1161/CIRCULATIONAHA.106.675041
Wu Y, Temple J, Zhang R, Dzhura I, Zhang W, Trimble R, Roden DM, Passier R, Olson EN, Colbran RJ, Anderson ME (2002) Calmodulin kinase II and arrhythmias in a mouse model of cardiac hypertrophy. Circulation 106(10):1288–1293
Yang Y, Zhu WZ, Joiner ML, Zhang R, Oddis CV, Hou Y, Yang J, Price EE, Gleaves L, Eren M, Ni G, Vaughan DE, Xiao RP, Anderson ME (2006) Calmodulin kinase II inhibition protects against myocardial cell apoptosis in vivo. Am J Physiol Heart Circ Physiol 291(6):H3065–H3075. doi:10.1152/ajpheart.00353.2006
Zhang T, Brown JH (2004) Role of Ca2+/calmodulin-dependent protein kinase II in cardiac hypertrophy and heart failure. Cardiovasc Res 63(3):476–486. doi:10.1016/j.cardiores.2004.04.026
Zhang T, Miyamoto S, Brown JH (2004) Cardiomyocyte calcium and calcium/calmodulin-dependent protein kinase II: friends or foes? Recent Prog Horm Res 59:141–168
Zhang R, Khoo MS, Wu Y, Yang Y, Grueter CE, Ni G, Price EE Jr, Thiel W, Guatimosim S, Song LS, Madu EC, Shah AN, Vishnivetskaya TA, Atkinson JB, Gurevich VV, Salama G, Lederer WJ, Colbran RJ, Anderson ME (2005) Calmodulin kinase II inhibition protects against structural heart disease. Nat Med 11(4):409–417. doi:10.1038/nm1215
Zhu WZ, Zou Y, Shiojima I, Kudoh S, Aikawa R, Hayashi D, Mizukami M, Toko H, Shibasaki F, Yazaki Y, Nagai R, Komuro I (2000) Ca2+/Calmodulin-dependent Kinase II and Calcineurin play critical roles in endothelin-1-induced cardiomyocyte hypertrophy. J Biol Chem 275(19):15239–15245
Acknowledgments
We thank Trine Skoglund for excellent laboratory assistance. The study was supported by grants from the K.G. Jebsen Foundation; the Blix Foundation for the Promotion of Medical Science (GK), and the Norwegian Research Council Funding for Outstanding Young Investigators (UW), and the British Heart Foundation (OJK).
Conflict of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Keith Phillip George.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Kaurstad, G., Alves, M.N., Kemi, O.J. et al. Chronic CaMKII inhibition blunts the cardiac contractile response to exercise training. Eur J Appl Physiol 112, 579–588 (2012). https://doi.org/10.1007/s00421-011-1994-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-011-1994-0