Abstract
Purpose
Work disability (WD) as a medico-legal concept refers to disability benefits (DB) that are granted due to diseases that permanently reduce work ability. We studied whether an occupational healthcare instrument for the prediction of sickness absence (SA) risk—a health risk appraisal (HRA)—also predicts permanent WD.
Methods
HRA results were combined with registry data on DB of 22,023 employees from different industry sectors. We analysed how the HRA risk categories predict DB and considered occupational group, gender, age, and prior SA as confounding variables. Cumulative incidence function illustrates the difference between the HRA risk categories, and the Fine–Gray model estimates the predictors of WD during 6-year follow-up.
Results
The most common primary reasons for permanent WD were musculoskeletal (39%) and mental disorders (21%). Self-reported health problems in the HRA, labelled as “WD risk factors”, predicted DB when controlling for age and prior SA. Hazard ratios were 10.9 or over with the lower limit of the 95% confidence interval 3.3 or over among those with two simultaneous WD risk factors. 14% of the females and 17% of the males with three or more simultaneous WD risk factors had received a DB, whereas the respective figures among those without findings were 1.9% and 0.3%.
Conclusions
Self-reported health problems in the HRA, especially multiple simultaneous WD risk factors, predict permanent WD among both genders across occupational groups. Screening WD risk with a self-administered questionnaire is a potential means for identifying high-risk employees for targeting occupational healthcare actions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The cost of work disability benefits (DB) has become a significant burden to public finances globally (Aumayr-Pintar et al. 2016). Across the OECD countries, public spending on DB is around 2–6% of the gross domestic product (GDP) of the working-age population, depending on the country (OECD 2010). In 2014, about 7% of the Finnish working-age population was on a DB, and the average age of the onset of a permanent DB was 52 (Laaksonen et al. 2016b).
Permanent work disability (WD) is a medico-legal concept (De Boer et al. 2008), which in Finland is defined as having been granted a DB. The benefits programme of the Social Insurance Institution of Finland (Kela) provides coverage for lost income due to medically certified sickness up to 1 year. Thereafter, the DB scheme, operated by pension insurance companies, covers lost income for those eligible. Work ability is assessed on the basis of the employee’s remaining ability to earn an income from work that can reasonably be expected on the basis of their education, previous work history, age, housing conditions, and other social factors. A DB is granted if, based on the attending physician’s statement, the employee’s ability to work is permanently reduced and the expert panel agrees that the decrease in functional capacity and work ability is due to illness or injury. Thus, a granted DB serves a proxy for permanent WD in the present study.
Most Finnish employees use occupational healthcare services (OHS) for all primary healthcare needs. Finnish OHS covers approximately 90% of the total workforce (Lappalainen et al. 2016; Kela-Social Insurance Institution 2019), and carry out preventive and curative health care (Kela-Social Insurance Institution of Finland 2018). One of the primary tasks of OHS in Finland includes protection of employees’ work ability, for which purpose early identification of WD risk would be desirable and, therefore, instruments to tap risks are developed in OHS. Work ability and disability are complex and multifactorial phenomena, determined by personal, socio-demographical, lifestyle- and health-related factors as well as organisational determinants, healthcare management, and legislation. In most countries with disability pension schemes, permanent WD is usually due to a chronic disease (De Boer et al. 2008), which reduces functional capacity and work ability (OECD 2010). The key employee-related predictors of WD reported in observational studies can be divided into demographic factors (e.g., age, gender and educational status) (Laaksonen et al. 2016a; Polvinen et al. 2016; Samuelsson et al. 2012), health status (Karpansalo et al. 2004), and work (e.g., type of occupation) (Haukenes et al. 2011; Borg et al. 2001; Leinonen et al. 2011; Polvinen et al. 2014). Previous studies also suggest that both short-term (Alexanderson et al. 2012; Karlsson et al. 2008; Kivimäki et al. 2004; Virtanen et al. 2006), and long-term (Airaksinen et al. 2018; Gjesdal et al. 2004; Lund et al. 2008) sickness absences (SA) predict new sick leaves and permanent WD.
Some screening questionnaires, such as the World Health Organization’s Health and Work Performance Questionnaire (WHO-HPQ) (Kessler et al. 2003), the Work Ability Index (WAI) (Ilmarinen et al. 1997; Jääskeläinen et al. 2016; Kinnunen and Nätti 2018), and the 12-item Short Form Health Survey (SF-12) (Laaksonen et al. 2011; Roelen et al. 2015), to name a few, are used by researchers, but have not been implemented in broader clinical use. They are laborious to fill out, and more importantly, they are detached from the OHS processes such as occupational health surveillance. Only the WAI has evidence for the capability of predicting permanent WD (Kinnunen and Nätti 2018). Moreover, most of the previous studies have been performed among public sector employees (Airaksinen et al. 2018; Kinnunen and Nätti 2018; Laaksonen et al. 2011), or in specific industries or occupational groups (Kant et al. 2009; Niessen et al. 2012; Roelen et al. 2015; Schouten et al. 2015; Stange et al. 2016). There are different pension act legislations in the public and private sector in Finland, for which reason generalization based on public sector studies to the entire working life should be done with caution. Also, working cultures vary by sector and industry, which is reflected in much higher SA rates in the public sector than in the private sector (Seppänen 2010).
In the present study, we used a health risk appraisal (HRA), which was able to identify blue-collar employees in the construction industry with a high number of SA days in a previous study (Taimela et al. 2007). Especially multimorbidity, i.e., the presence of more than one simultaneous risk factor predicted SA days (Taimela et al. 2007). The HRA presents the results as different risk categories primarily based on self-reported symptoms and health behaviours. The online HRA is widely used in Finland and the Netherlands as a part of preventive occupational health services (OHS) by different providers to recognize employees at risk for SA and to target interventions for those in need. Previous randomised trial also showed that the targeted interventions put in place for employees with high risk of SA, based on the HRA results, were effective in reducing SA days (Taimela et al. 2008a, 2010) and reduced the use of healthcare resources (Taimela et al. 2008b). The predictive ability of the HRA on permanent WD has not been studied before.
We assessed whether the HRA, which is used as an occupational health-care instrument for the prediction of SA, also predicts permanent WD and if so, whether the WD risk increases by the number of self-reported health problems. We hypothesized that the HRA has an independent predictive effect on granted DB as a proxy measure of WD and that the higher the number of risk factors, the higher the WD risk.
Methods
Study design, ethics, and setting
The study design was an analysis of prospectively collected register data. We obtained the questionnaire data and the SA data from one OHS provider’s registers. The DB data were obtained from the Finnish Centre for Pensions (ETK), which combines DBs under different pension act legislations into one that is linked to an employee’s career, not to a particular employer, and the coverage of the register is practically 100%. We then combined the data registers using a unique identified, the Finnish social security code. Data privacy was strictly followed.
The Tampere University Research Ethics Board approved the study (ETL code R16074), and it was conducted in accordance with the Declaration of Helsinki.
The study setting was preventive OHS within the framework of the DB legislation in Finland.
Participants
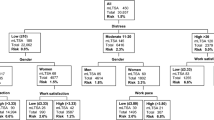
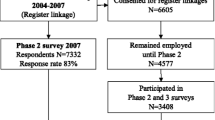
The cohort was formed of employees from different companies who acquired their OHS from one nationwide provider, which offers services to a variety of sectors and company sizes. The participants were 19–68 years old Finnish residents, who had completed the HRA (N = 22,023) during 2012–2015. We included only the first response. The data on DBs from the national register of ETK covered years 2012–2017. We had access to the complete information on all DB events including their primary and secondary diagnoses based on the International Classification of Diseases, 10th Revision. Figure 1 shows the participants’ exclusion and inclusion criteria.
Inclusion criteria were a completed HRA. An invitation to the HRA had been sent to 33,990 employees during 2012–2015, of which 11,475 had not responded (response rate 66%). We excluded the participants if DB had been previously granted (N = 415) or data concerning occupational group were missing (N = 79).
Measurements
Explanatory variables
The primary exposure variable of interest in the statistical models was the classified result of the HRA. The result categories in declining priority order are (1) work disability risk, (2) health risk, (3) some symptoms, (4) lifestyle issues, and (5) no findings (Table 1). The first category, labelled as “WD risk”, includes the following self-reported health problems: musculoskeletal problems, depressive symptoms, sleep problems, constant stress and feeling of exhaustion, and doubts about work ability. Within the category “WD risk”, the results were further subdivided by the number of risk factors (one, two, three or more). We combined the “lifestyle issues” and “no findings” categories as the reference class and included the result of the HRA (six categories) as a covariate in the statistical models.
Gender, age, occupational group and the accumulated SA days during the 12 months preceding the HRA were treated as confounding variables. Age was categorized into five classes: ≤ 30, 30–40, 40–50, 50–60, and > 60 years. Occupational group was defined as blue-collar workers, clerical employees, and professionals/managers. The number of SA days 12 months prior to the questionnaire was included as a continuous variable.
Work disability
The outcome variable was a granted DB as a proxy measure of permanent WD, and it was operationalized dichotomously as a granted DB: yes/no. The mean follow-up time was 3.5 years (SD 1.1, range from 3 days to 5.9 years, median 3.3 years) from the date of the survey response.
DBs in our study consist of four categories as follows: (1) full and (2) partial disability pension, or (3) full and (4) partial rehabilitation subsidy. A DB is granted if the remaining maximum capacity to work is 40% (2/5), as in the case of a full-time benefit; or 60% (3/5), as in the case of a partial benefit. The duration of the DB can be until further notice or for a temporary period. The common requirement in all categories of DB is the permanent nature of reduction of work ability.
Statistical methods
It has been suggested that gender should not be treated as a covariate and that the analyses should be carried out separately by gender (Messing et al. 2003). Indeed, there were complex interactions in our study between gender and occupational groups (data not shown), and we performed all analyses stratified by gender.
We present descriptive statistics to describe the eligibility categories and the most common health issues that lead to DBs. We compared the demographic characteristics of the participants and non-participants using t test and Chi-squared test. We used the cumulative incidence function (CIF) to illustrate the difference between the HRA risk categories (Kim 2007), and the Fine–Gray proportional hazards model to estimate how HRA categories, age and occupational group affected the probability of events, i.e. a granted DB, prior to a follow-up (Fine and Gray 1999). The Fine–Gray model provides hazard ratio (HR) estimates to describe the relative effect of covariates, which are then also associated with the probability of a DB occurring over time. Model 1 included only the HRA categories; and Model 2, the fully adjusted model, also included age, occupational group and earlier SA.
The statistical analyses were performed using the cmprsk library and R 3.4.4 software.
Results
The mean age of the participants was 45.5 years (SD 11.1; range 19.1–68.0), 59% (N = 12933) were female, 31% (N = 6807) were blue-collar workers, 55% (N = 12072) were clerical employees, and 14% (N = 3144) belonged to the professional or manager category. The non-respondents were slightly younger (average age 44.2 years, SD 12.3; t = − 9.0; p < 0.0001) than the respondents on the average. Also, males were less likely to respond than females with response rates 60% and 71%, respectively (Chi square 425.5; p < 0.0001). The response rates were almost identical among blue-collar workers (65%), clerical employees (67%) and experts/managers (66%), (Chi square 14.3; p = 0.0007).
A total of 379 participants in the cohort were granted a DB on the average 2 years (range from 3 days to 5.7 years) after the HRA. The overall annual incidence of a DB was 0.29%: 0.33% among the females and 0.23% among the males (p = 0.23). In the Fine–Gray model, which included gender as the explanatory variable and age, occupational group, and SA days before questionnaire as confounders, the HR for gender was 1.2 (0.9–1.5; males as the reference).
Of those who had received a DB, 149 (39%) participants had a primary diagnosis of a musculoskeletal disorder and 80 (21%) participants had a primary diagnosis of a mental or behavioural disorder (Table 2). Fifteen participants had both musculoskeletal and mental or behavioural diagnoses simultaneously (4% of all DBs).
Figure 2 presents the cumulative incidence of the DBs during the 6-year follow-up period in the HRA categories. The HRA “work disability risk” category predicted DB and there was a dose–response relationship between the number of WD risk factors and the probability of ending up on DB. Of the females with three or more WD risk factors, 14% received a DB at 6 years, while the respective figure among the males was 17%. The respective figures for those in the HRA “no symptoms” category was 1.9% for females and 0.3% for males.
In the fully adjusted Fine–Gray model, the HRA WD risk categories, age, occupational group, and SA before the HRA questionnaire predicted the probability of DB for both genders in an additive manner (Table 3). In the unadjusted model (Model 1), the HR for the probability of a DB was 36.2 (8.8–148.4) for the females and 47.7 (14.4–158.1) for the males in the HRA WD risk groups with three and more risk factors. When all covariates were included (Model 2), HR decreased among both genders, and was 17.3 (4.2–71.7) for the females, and 18.2 (5.4–60.8) for the males (Table 3). The same was also seen in the HRA WD risk categories with one and two risk factors. In the fully adjusted model, HR by age was the highest in the 50- to 60-year age group, among both genders [12.9 (4.8–35.2) for females, and 26.4 (3.6–192.8) for males]. By occupational group, blue-collar workers had the highest HRs [3.6 (1.7–7.9) for females and 2.4 (1.2–4.9) for males]. The higher the number of SA days prior to the survey, the higher the HR among both genders.
Discussion
Self-reported health problems in the HRA—musculoskeletal problems, depressive symptoms, sleep problems, constant stress and feeling of exhaustion, and doubts about work ability—predicted WD in both genders, in all occupational groups. Of note, the larger the number of these problems, labelled as “WD risk factors”, the higher was the risk for WD. In Finland, the two largest categories of the causes of permanent WD are musculoskeletal disorders and mental and behavioural disorders (Social Insurance Institution of Finland 2019; Official Statistics 2018). Also, problems with sleep (Haaramo et al. 2012), constant stress (Juvani et al. 2018), exhaustion (Ahola et al. 2009), and attitudes towards work ability (Kinnunen and Nätti 2018) have predicted SA and/or WD in earlier studies. It seems that using a questionnaire for self-rating of relevant symptoms is a valid way to identify individuals at risk of WD, as the HRs were relatively high in our study. Age, occupational group and earlier SA also predicted future DB in an additive manner. By age, the risk of DB was the highest in the 50- to 60-year age group, among both genders.
Reporting health problems in the HRA had a strong, independent predictive value for future DB. Earlier studies have provided evidence that self-reports in a questionnaire predict DB (Bethge et al. 2017). The Work Ability Index (WAI) (Ilmarinen 2009) has been used in countries such as Finland and other Scandinavian countries, the Netherlands, and Germany (Bethge et al. 2017; Jääskeläinen et al. 2016). Two longitudinal studies have reported that the risk of a granted DB was higher among employees with poorer WAI scores [HR 7.8; 95% CI 2.6–23.4 (Bethge et al., 2017), and HR 5.0; 95% CI 4.4–5.6 (Jääskeläinen et al. 2016)]. Our results provide further support for earlier studies that perceived health and symptoms predict WD. Of note, the HRs in our study were exceptionally high among those reporting multiple “WD risk factors”, i.e., health problems. Age has been a predictor of a future DB in previous studies (Gjesdal et al. 2004; Karlsson et al. 2008). By age, the risk of WD was the highest in the 50- to 60-year age group in our study population. This might be because of a “healthy worker survivor effect” (Osmotherly and Attia 2006), which means that only the healthiest and strongest remain in working life, and those who became unfit during their employment tend to leave working life earlier (Osmotherly and Attia 2006). This effect was notable in our study, in which the over-60 age group had a lower rate of DBs than the 50- to 60-year age group. The HRs for DBs were highest among the blue-collar employees in the present study. This is in line with a previous study, in which the data were drawn from seven independent studies in Finland, France, the UK and the USA, and which reported an association with a low occupational grade and increased risks of health-related exit from work (Carr et al. 2018). A Finnish cohort study found that higher occupational classes are two times more likely to continue working beyond retirement age than lower occupational classes, while another cohort study found that hospitalization was slightly more associated with increased DB in the lower occupational classes. These studies indicate that lower occupational classes have poorer health. In our study, the gender difference was not statistically significant in terms of the annual incidence of granted DB. The findings of previous studies in this respect are contradictory. A previous prospective study found no overall gender difference in DB rates (Gjesdal et al. 2004), whereas other studies have found gender differences. A Finnish register-based retrospective study found a gender difference between different SA trajectories, which led to DB (Laaksonen et al. 2016a), although the associations with socio-demographic variables were weak. A Swedish twin cohort found that females are at a higher risk of DB (HR 1.31; 1.26–1.37) than males (HR 1.00; reference). In the present study, we found that earlier SA days predicted future DB, which is in line with previous studies (Kivimäki et al. 2004; Laaksonen et al. 2016a; Lund et al. 2008; Øyeflaten et al. 2014; Salonen et al. 2018).
The key strength of our study is its prospectively collected, extensive, registry-based data from various industries. We were also able to control potential confounders such as age, gender and occupational group. The archival data of DBs at the ETK were comprehensive and virtually no data were lost to follow-up (Finnish Centre for Pensions 2018). We combined all four DB categories as one as the proxy measure for WD: this way, no data were lost and virtually all the DB recipients had had at least 1 year of sickness allowance before the granted DB. Another strength is that we used the HRA, which can identify employees with a high number of SA days (Taimela et al. 2007). The follow-up continued at least 2 years after the completed HRA. Sickness allowance is paid for a maximum of 1 year after the onset of WD in Finland and the DB decision is typically made shortly after the sickness allowance period. Thus, the 2-year follow-up period was long enough to detect all new potential DB receivers.
We chose to use the Fine–Gray model to estimate the effect of the covariates on the rate at which WD occurs. Although the model was perhaps not able to deal with all the complexity associated with our data, among computationally feasible approaches, it is more appropriate than, e.g., the Kaplan–Meier survival analysis that tends to overestimate cumulative incidence of health-related events (Lacny et al. 2018). Besides, it was easier to add variables to Fine–Gray model than for example in Kaplan–Meier. Moreover, we prefer talking about cumulative hazards to “survival at work” conceptually. However, interpretation of the HR estimates from the Fine–Gray model is not straightforward. We recommend interpreting the covariates as having an effect on the incidence of WD (i.e., on the CIF). However, the magnitude of the relative effect of the covariate on the subdistribution hazard function is different from the magnitude of the effect of the covariate on the CIF. Yet one can conclude that if a variable increases the subdistribution hazard function, it will also increase the incidence of the event. However, one cannot infer that the exact magnitudes of these two effects are the same (Austin and Fine 2017).
We did not have access to the statutory accident insurance data, so WD resulting from accidents at work, occupational diseases, and traffic accidents are not included in our study. Moreover, our results can only cautiously be generalized to the entire working-age population, because people outside working life were not involved in our study. Another limitation of study is the potential selection bias due to differences between respondents and non-respondents. “Healthy worker effect” might be present if employees with worse health level had not responded or they are less likely to hire (Chowdhury et al. 2017). Similar bias would potentially result from a “healthy worker survival effect”, which means that only healthiest and strongest will remain in the working life (Nordström et al. 2016). All this might underestimate the associations. It may also be possible that the healthiest employees might not respond to the HRA, which would have an opposite effect on our estimates.
Some DB criteria are comparable between countries, such as requirements for a health condition in relation to work and the permanence of the condition (De Boer et al. 2008). However, the implementation of the legislation varies between countries (OECD 2010) and, therefore, our results must be interpreted with caution in the international context. However, we assume that the phenomenon itself—severe self-rated health problems predict WD—manifests in different medico-legal contexts.
The outcome of interest was rare in the entire population in our study, which is visible in the wide confidence limits for the different risk categories for both genders. However, permanent WD is very costly for society (OECD 2010), and the underlying diseases and disorders are a burden to disabled individuals in addition to their lost income. Hence, it is important to identify predictors of SA and WD and to determine how to prevent WD. Practical tools are needed to identify the risk factors for WD and to target interventions for those in need. The HRA used in the present study seems to function in OHS as a practical tool to recognize employees at increased risk for SA and DB early for the purpose of targeting OHS actions to those who need special support in maintaining their work ability. The aggregated results may also be utilised in promoting sustainable working conditions.
Our results indicate high HRs for permanent WD among employees belonging to in the HRA work disability risk category and provide further support that in addition to prior absence from work, physically demanding work and age, self-reported health problems play an independent role in identifying employees who are at an increased risk of WD. Further research is needed to assess the effectiveness and cost-effectiveness of targeted health surveillance among the risk groups.
Data sharing statement
No additional data are available due to data privacy reasons.
References
Ahola K, Gould R, Virtanen M, Honkonen T, Aromaa A, Lönnqvist J (2009) Occupational burnout as a predictor of disability pension: a population-based cohort study. Occup Environ Med 66(5):284–290. https://doi.org/10.1136/oem.2008.038935
Airaksinen J, Jokela M, Virtanen M, Oksanen T, Koskenvuo M, Pentti J, Vahtera J, Kivimäki M (2018) Prediction of long-term absence due to sickness in employees: development and validation of a multifactorial risk score in two cohort studies. Scand J Work Environ Health 44(3):274–282. https://doi.org/10.5271/sjweh.3713
Alexanderson K, Kivimäki M, Ferrie JE, Westerlund H, Vahtera J, Singh-Manoux A, Melchior M, Zins M, Goldberg M, Head J (2012) Diagnosis-specific sick leave as a long-term predictor of disability pension: a 13-year follow-up of the GAZEL cohort study. J Epidemiol Commun Health 66(2):155–159
Aumayr-Pintar C, Moulaï K, Ajzen M (2016) European Foundation for the improvement of living and working conditions. In: Developments in working life in Europe: EurWORK annual review 2015. Publications Office of the European Union (Luxembourg), Luxembourg. http://hdl.handle.net/2078.1/176825. Accessed Mar 2018
Austin PC, Fine JP (2017) Practical recommendations for reporting Fine-Gray model analyses for competing risk data. Stat Med 36(27):4391–4400. https://doi.org/10.1002/sim.7501
Bethge M, Spanier K, Peters E, Michel E, Radoschewski M (2017) Self-reported work ability predicts rehabilitation measures, disability pensions, other welfare benefits, and work participation: longitudinal findings from a sample of german employees. J Occup Rehabil 28(3):495–503. https://doi.org/10.1007/s10926-017-9733-y
Borg K, Hensing G, Alexandersson K (2001) Predictive factors for disability pension—an 11-year follow up of young persons on sick leave due to neck, shoulder, or back diagnoses. Scand J Public Health 29(2):104–112. https://doi.org/10.1080/14034940152393363
Carr E, Fleischmann M, Goldberg M, Kuh D, Murray ET, Stafford M, Stansfeld S, Vahtera J, Xue B, Zaninotto P, Zins M, Zaninotto P (2018) Occupational and educational inequalities in exit from employment at older ages: evidence from seven prospective cohorts. Occup Environ Med 75(5):369–377
Chowdhury R, Shah D, Payal AR (2017) Healthy worker effect phenomenon: revisited with emphasis on statistical methods—a review. Indian J Occup Environ Med 21(1):2
De Boer WEL, Donceel P, Brage S, Rus M, Willems JHBM (2008) Medico-legal reasoning in disability assessment: a focus group and validation study. BMC Public Health 8(1):335. https://doi.org/10.1186/1471-2458-8-335
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94(446):496–509. https://doi.org/10.1080/01621459.1999.10474144
Finnish Centre for Pensions (2018) Disability pension if your working ability has been reduced (homepage on the Internet). Published 2017. https://www.tyoelake.fi/en/different-pensions/disability-pension-if-your-working-ability-has-been-reduced/. Accessed 4 Oct 2018
Gjesdal S, Ringdal PR, Haug K, Mæland JG (2004) Predictors of disability pension in long-term sickness absence: results from a population-based and prospective study in Norway 1994–1999. Eur J Public Health 14(4):398–405. https://doi.org/10.1093/eurpub/14.4.398
Haaramo P, Rahkonen O, Lahelma Eero, Lahelma E, Lallukka T (2012) The joint association of sleep duration and insomnia symptoms with disability retirement—a longitudinal, register-linked study. Scand J Work Environ Health 38(5):427–435. https://doi.org/10.5271/sjweh.3269
Haukenes I, Mykletun A, Knudsen AK, Hansen H, Mæland JG (2011) Disability pension by occupational class—the impact of work-related factors: the Hordaland Health Study Cohort. BioMed Central Ltd., England. https://doi.org/10.1186/1471-2458-11-406
Ilmarinen J (2009) Work ability—a comprehensive concept for occupational health research and prevention. Scand J Work Environ Health 35(1):1–5
Ilmarinen J, Tuomi K, Klockars M (1997) Changes in the work ability of active employees over an 11-year period. Scand J Work Environ Health 23:49–57
Jääskeläinen A, Kausto J, Seitsamo J, Ojajärvi A, Nygård C, Arjas E, Leino-Arjas P (2016) Work ability index and perceived work ability as predictors of disability pension: a prospective study among Finnish municipal employees. Scand J Work Environ Health 42(6):490–499. https://doi.org/10.5271/sjweh.3598
Juvani A, la Oksanen T, Virtanen M, Salo P, Pentti J, Kivimäki M, Vahtera J (2018) Clustering of job strain, effort-reward imbalance, and organizational injustice and the risk of work disability: a cohort study. Scand J Work Environ Health. https://doi.org/10.5271/sjweh.3736
Kant I, Jansen N, van Amelswoort L, Swaen G, van Leusden R, Berkouwer A (2009) Screening questionnaire Balansmeter proved successful in predicting future long-term sickness absence in office workers. J Clin Epidemiol 62(4):40–414.e2. https://doi.org/10.1016/j.jclinepi.2008.07.003
Karlsson NE, Carstensen JM, Gjesdal S, Alexanderson KAE (2008) Risk factors for disability pension in a population-based cohort of men and women on long-term sick leave in Sweden. Eur JPublic Health 18(3):224–231. https://doi.org/10.1093/eurpub/ckm128
Karpansalo M, Manninen P, Kauhanen J, Lakka TA, Salonen JT (2004) Perceived health as a predictor of early retirement. Scand J Work Environ Health 30(4):287–292
Kela-The Social Insurance Institution of Finland (2018) Kelan sairausvakuutustilasto, FPA-statistik sjukförsäkring 2017. Official Statistics in Finland (homepage on the Internet). Published in Finnish and Swedish (Health insurance statistics 2018). http://urn.fi/URN:NBN:fi-fe2018091735890. Accessed 1 Jan 2019
Kela-The Social Insurance Institution of Finland (2019) Kelan työterveyshuoltotilasto, FPA-statistik, foretaghälsovård 2017. Official Statistics in Finland (homepage on internet). Published in Finnish and Swedish (Occupational health statistics 2017). http://urn.fi/URN:NBN:fi-fe2019061720794
Kessler R, Barber C, Beck A, Berglund P, Cleary P, McKenas D, Pronk N, Simon G, Stang P, Ustun TB, Wang P (2003) The world health organization health and work performance questionnaire (HPQ). J Occup Environ Med 45(2):156–174. https://doi.org/10.1097/01.jom.0000052967.43131.51
Kim HT (2007) Cumulative incidence in competing risks data and competing risks regression analysis. Clin Cancer Res 13(2):559–565. https://doi.org/10.1158/1078-0432.CCR-06-1210
Kinnunen U, Nätti J (2018) Work ability score and future work ability as predictors of register-based disability pension and long-term sickness absence: a three-year follow-up study. Scand J Public Health 46(3):321–330
Kivimäki M, Forma P, Wikström J, Halmeenmäki T, Pentti J, Elovainio M, Vahtera J (2004) Sickness absence as a risk marker of future disability pension: the 10-town study. J Epidemiol Commun Health (1979) 58(8):710–711. https://doi.org/10.1136/jech.2003.015842
Laaksonen M, Kääriä S, Leino-Arjas P, Lahelma E (2011) Different domains of health functioning as predictors of sickness absence—a prospective cohort study. Scand J Work Environ Health 37(3):213–218. https://doi.org/10.5271/sjweh.3131
Laaksonen M, Blomgren J, Gould R (2016a) Sickness allowance trajectories preceding disability retirement: a register-based retrospective study. Eur J Public Health 26(6):1050–1055. https://doi.org/10.1093/eurpub/ckw081
Laaksonen M, Rantala J, Järnefelt N, Kannisto J (2016b) Työkyvyttömyyden vuoksi menetetty työura (homepage on the Internet). Eläketurvakeskus 2016. Originally published in Finnish, summary in English (Working lives reduced by disability pension). http://urn.fi/URN:978-951-691-247-2. Accessed 4 Oct 2018
Lacny S, Wilson T, Clement F, Roberts DJ, Faris P, Ghali WA, Marshall DA (2018) Kaplan–Meier survival analysis overestimates cumulative incidence of health-related events in competing risk settings: a meta-analysis. J Clin Epidemiol 93:25–35. https://doi.org/10.1016/j.jclinepi.2017.10.006
Lappalainen K, Aminoff M, Hakulinen H, Hirvonen M, Räsänen K, Sauni R, Stengård J (2016) Työterveyshuolto suomessa vuonna 2015: Ja kehitystrendi 2000–2015. Tietoa Työstä 2016. Originally published in Finnish (Occupational health care in Finland 2015: and the development trend 2000–2015) (homepage on the Internet). https://www.julkari.fi/handle/10024/131293. Accessed May 2018
Leinonen T, Pietiläinen O, Laaksonen M, Rahkonen O, Lahelma E, Martikainen P (2011) Occupational social class and disability retirement among municipal employees—the contribution of health behaviors and working conditions. Scand J Work Environ Health 37(6):464–472. https://doi.org/10.5271/sjweh.3182
Lund T, Kivimäki M, Labriola M, Villadsen E, Christensen KB (2008) Using administrative sickness absence data as a marker of future disability pension: the prospective DREAM study of Danish private sector employees. Occup Environ Med 65(1):28–31. https://doi.org/10.1136/oem.2006.031393
Messing K, Punnett L, Bond M, Alexanderson K, Pyle J, Zahm S, Wegman D, Stock S, de Grosbois S (2003) Be the fairest of them all: challenges and recommendations for the treatment of gender in occupational health research. Am J Ind Med 43(6):618. http://kipublications.ki.se/Default.aspx?queryparsed=id:19271499
Niessen MAJ, Kraaijenhagen RA, Dijkgraaf MGW, van Pelt D, van Kalken CK, Peek N (2012) Impact of a web-based worksite health promotion program on absenteeism. J Occup Environ Med/Am Coll Occup Environ Med 54(4):404–408. https://doi.org/10.1097/JOM.0b013e31824d2e43
Nordström K, Hemmingsson T, Ekberg K, Johansson G (2016) Sickness absence in workplaces. Int J Occup Med Environ Health 29(2):315. http://urn.kb.se/resolve?urn=urn:nbn:se:su:diva-126184
OECD, Organisation for Economic Co-operation and Development (2010) Sickness, disability and work: breaking the barriers: a synthesis of findings across OECD countries. OECD Publishing, Paris. https://doi.org/10.1787/9789264088856-en. https://doi.org/10.1787/9789264088856-en
Official Statistics, Finland (2018) Recipients of disability pension (homepage on the internet). https://findikaattori.fi/fi/76. Accessed Oct 2018
Osmotherly P, Attia J (2006) The healthy worker survivor effect in a study of neck muscle performance measures in call-centre operators. Work 26(4):399–406
Øyeflaten I, Lie SA, Ihlebæk CM, Eriksen HR (2014) Prognostic factors for return to work, sickness benefits, and transitions between these states: a 4-year follow-up after work-related rehabilitation. J Occup Rehabil 24(2):199–212
Polvinen A, Laaksonen M, Gould R, Lahelma E, Martikainen P (2014) The contribution of major diagnostic causes to socioeconomic differences in disability retirement. Scand J Work Environ Health 40(4):353–360. https://doi.org/10.5271/sjweh.3411
Polvinen A, Laaksonen M, Gould R, Lahelma E, Leinonen T, Martikainen P (2016) Socioeconomic differences in cause-specific disability retirement in Finland, 1988 to 2009. J Occup Environ Med 58(8):840–845. https://doi.org/10.1097/JOM.0000000000000808
Roelen CAM, Heymans MW, Twisk JWR, Laaksonen M, Pallesen S, Mageroy N, Moen B, Bjorvatn B (2015) Health measures in prediction models for high sickness absence: single-item self-rated health versus multi-item SF-12. Eur J Public Health 25(4):668–672. https://doi.org/10.1093/eurpub/cku192
Salonen L, Blomgren J, Laaksonen M, Niemelä M (2018) Sickness absence as a predictor of disability retirement in different occupational classes: a register-based study of a working-age cohort in Finland in 2007–2014. BMJ Open 8(5):e020491. https://doi.org/10.1136/bmjopen-2017-020491
Samuelsson Å, Alexanderson K, Ropponen A, Lichtenstein P, Svedberg P (2012) Incidence of disability pension and associations with socio-demographic factors in a Swedish twin cohort. Soc Psychiatry Psychiatr Epidemiol 47(12):1999–2009. https://doi.org/10.1007/s00127-012-0498-5
Schouten LS, Joling CI, van der Gulden Joost WJ, Heymans MW, Bültmann U, Roelen CA (2015) Screening manual and office workers for risk of long-term sickness absence: Cut-off points for the work ability index. Scand J Work Environ Health 41:36–42
Seppänen T (2010) Absence from work—Finland (homepage on the Internet). Published 20 Jul 2010. https://www.eurofound.europa.eu/publications/report/2010/absence-from-work-finland. Accessed 26 Mar 2019
Social Insurance Institution of Finland (2019) Statistics on the pensions provided by Kela (homepage on internet). https://www.kela.fi/web/en/485. Accessed 10 Sep 2019
Stange B, McInerney J, Golden A, Benade W, Neill B, Mayer A, Witter R, Tenney L, Stinson K, Cragle D, Newman LS (2016) Integrated approach to health screening of former department of energy workers detects both occupational and non-occupational illness. Am J Ind Med 59(3):200–211. https://doi.org/10.1002/ajim.22554
Taimela S, Läärä E, Malmivaara A, Tiekso J, Sintonen H, Justén S, Aro T (2007) Self-reported health problems and sickness absence in different age groups predominantly engaged in physical work. Occup Environ Med 64(11):739–746. https://doi.org/10.1136/oem.2006.027789
Taimela S, Malmivaara A, Justén S, Läärä E, Sintonen H, Tiekso J, Aro T (2008a) The effectiveness of two occupational health intervention programmes in reducing sickness absence among employees at risk. Two randomised controlled trials. Occup Environ Med 65(4):236–241. https://doi.org/10.1136/oem.2007.032706
Taimela S, Justén S, Aronen P, Sintonen H, Läärä E, Malmivaara A, Tiekso J, Aro T (2008b) An occupational health intervention programme for workers at high risk for sickness absence. Cost effectiveness analysis based on a randomised controlled trial. Occup Environ Med 65(4):242–248. https://doi.org/10.1136/oem.2007.033167
Taimela S, Aronen P, Malmivaara A, Sintonen H, Tiekso J, Aro T (2010) Effectiveness of a targeted occupational health intervention in workers with high risk of sickness absence: baseline characteristics and adherence as effect modifying factors in a randomized controlled trial. J Occup Rehabil 20(1):14–20. https://doi.org/10.1007/s10926-009-9221-0
Virtanen M, Kivimäki M, Vahtera J, Elovainio M, Sund R, Virtanen P, Ferrie JE (2006) Sickness absence as a risk factor for job termination, unemployment, and disability pension among temporary and permanent employees. Occup Environ Med 63(3):212–217. https://doi.org/10.1136/oem.2005.020297
Acknowledgements
Open access funding provided by University of Helsinki including Helsinki University Central Hospital.
Funding
This work was supported by Terveystalo, Evalua International, Tampere University, and Finnish Work Environment Fund.
Author information
Authors and Affiliations
Contributions
MP, JU, HA, and ST participated in planning the study. MK and TN conducted the statistical analyses. MP and ST interpreted the results. MP and ST wrote the first draft of the manuscript and all authors commented on and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Conflict of interest
Author Minna Pihlajamäki has received a Finnish Work Environment Fund scholarship. Author Heikki Arola is employed by Terveystalo. Author Simo Taimela is employed by Evalua International. Authors Jukka Uitti, Mikko Korhonen, and Tapio Nummi are employed by the Tampere University. There are no other competing interests to declare.
Patient consent
This study used solely secondary data retrieved from registers.
Ethical approval
The Tampere University Research Ethics Board approved the study (ETL code R16074).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Pihlajamäki, M., Uitti, J., Arola, H. et al. Self-reported health problems in a health risk appraisal predict permanent work disability: a prospective cohort study of 22,023 employees from different sectors in Finland with up to 6-year follow-up. Int Arch Occup Environ Health 93, 445–456 (2020). https://doi.org/10.1007/s00420-019-01497-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-019-01497-2