Abstract
Purpose
To analyze the choroidal morphological changes in central serous chorioretinopathy (CSC) using ultra-widefield (UWF)-optical coherence tomography (OCT).
Methods
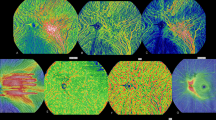
This single-center, case–control study included 65 CSC eyes (52 males; age, 55.6 ± 13.0 years) and 65 healthy eyes (50 males; age, 57.1 ± 17.9 years). UWF-OCT (viewing angle, 200°) with real-shape correction was used to create an automated choroidal thickness (CT) map. The CT map had three sub-areas: the central (0–30°), middle (30–60°), and peripheral areas (60–100°), and was divided by vertical and horizontal lines. Differences in the CT and the CT change rate (CTCR) from the central to peripheral areas were examined between the CSC and control groups after adjusting for subjects’ demographic and clinical factors. Furthermore, we assessed the vortex veins dilation patterns (VVDP) in the macula and examined the CT and the CTCR differences between CSC patients and controls for each VVDP.
Results
CSC patients had greater CT than those of the controls in all sectors (CSC vs. controls, the peripheral area: supratemporal 284.4 ± 71.2 μm vs. 220.4 ± 71.2 μm, infratemporal 263.3 ± 69.2 μm vs. 195.3 ± 52.3 μm, supranasal 251.9 ± 70.3 μm vs. 189.5 ± 58.1 μm, infranasal 193.6 ± 71.2 μm vs. 146.3 ± 48.9 μm, P < 0.0001 for all sectors). The CTCR was apparently larger in CSC eyes than controls only for the upper-dominant type of VVDP (CSC patients vs. controls, supratemporal 32.1 ± 9.9% vs. 4.6 ± 23.1%, infratemporal 44.0 ± 11.2% vs. 25.6 ± 16.8%, supranasal 42.6 ± 9.8% vs. 22.2 ± 19.4%, infranasal 57.6 ± 41.2% vs. 41.2 ± 13.9%, P < 0.0001 for all sectors).
Conclusions
CSC has a thicker choroid, even in the peripheral areas, and the macular choroidal thickening was more severe in the upper-dominant type of VVDP. VVDP may affect the location of excessive fluid.



Similar content being viewed by others
References
Shiragami C, Takasago Y, Osaka R et al (2018) Clinical features of central serous chorioretinopathy with type 1 choroidal neovascularization. Am J Ophthalmol 193:80–86. https://doi.org/10.1016/j.ajo.2018.06.009
Spaide RF, Campeas L, Haas A et al (1996) Central serous chorioretinopathy in younger and older adults. Ophthalmology 103:2070–9. https://doi.org/10.1016/s0161-6420(96)30386-2
Spaide RF, Hall L, Haas A et al (1996) Indocyanine green videoangiography of older patients with central serous chorioretinopathy. Retina 16:203–213. https://doi.org/10.1097/00006982-199616030-00004
Spaide RF, Koizumi H, Pozzoni MC (2008) Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol 146:496–500. https://doi.org/10.1016/j.ajo.2008.05.032
Srinivasan VJ, Adler DC, Chen Y et al (2008) Ultrahigh-speed optical coherence tomography for three-dimensional and en face imaging of the retina and optic nerve head. Invest Ophthalmol Vis Sci 49:5103–5110. https://doi.org/10.1167/iovs.08-2127
Shiihara H, Sonoda S, Terasaki H et al (2020) Quantitative analyses of diameter and running pattern of choroidal vessels in central serous chorioretinopathy by en face images. Sci Rep 10:9591. https://doi.org/10.1038/s41598-020-66858-1
Sonoda S, Sakamoto T, Kuroiwa N et al (2016) Structural changes of inner and outer choroid in central serous chorioretinopathy determined by optical coherence tomography. PLoS One 11:e0157190. https://doi.org/10.1097/IAE.0000000000003452
Hiroe T, Kishi S (2018) Dilatation of asymmetric vortex vein in central serous chorioretinopathy. Ophthalmol Retina 2:152–161. https://doi.org/10.1016/j.oret.2017.05.013
Imamura Y, Fujiwara T, Margolis R et al (2009) Enhanced depth imaging optical coherence tomography of the choroid in central serous chorioretinopathy. Retina 29:1469–1473. https://doi.org/10.1097/IAE.0b013e3181be0a83
Jirarattanasopa P, Ooto S, Tsujikawa A et al (2012) Assessment of macular choroidal thickness by optical coherence tomography and angiographic changes in central serous chorioretinopathy. Ophthalmology 119:1666–1678. https://doi.org/10.1016/j.ophtha.2012.02.021
Spaide RF, Gemmy Cheung CM, Matsumoto H et al (2022) Venous overload choroidopathy: a hypothetical framework for central serous chorioretinopathy and allied disorders. Prog Retin Eye Res 86:100973. https://doi.org/10.1016/j.preteyeres.2021.100973
Jeong S, Kang W, Noh D et al (2022) Choroidal vascular alterations evaluated by ultra-widefield indocyanine green angiography in central serous chorioretinopathy. Graefes Arch Clin Exp Ophthalmol 260(6):1887–1898. https://doi.org/10.1007/s00417-021-05461-0
Bacci T, Oh DJ, Singer M et al (2022) Ultra-widefield indocyanine green angiography reveals patterns of choroidal venous insufficiency influencing pachychoroid disease. Invest Ophthalmol Vis Sci 63(1):17. https://doi.org/10.1167/iovs.63.1.17
Jung JJ, Yu DJG, Ito K et al (2020) Quantitative assessment of asymmetric choroidal outflow in pachychoroid eyes on ultra-widefield indocyanine green angiography. Invest Ophthalmol Vis Sci 61:50. https://doi.org/10.1167/iovs.61.8.50
Izumi T, Maruko I, Kawano T et al (2022) Morphological differences of choroid in central serous chorioretinopathy determined by ultra-widefield optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 260:295–301. https://doi.org/10.1007/s00417-021-05380-0
Nishihara S, Maruko I, Izumi T et al (2022) Peripheral choroidal thickness determined by widefield optical coherence tomography in eyes with central serous chorioretinopathy. Retina 42(8):1450–1454. https://doi.org/10.1097/IAE.0000000000003478
Ishikura M, Muraoka Y, Nishigori N et al (2022) Wide field choroidal thickness of eyes with central serous chorioretinopathy examined by swept-source optical coherence tomography. Ophthalmol Retina 42(8):1450–1454. https://doi.org/10.1097/IAE.0000000000003478
Matsumoto H, Kishi S, Mukai R et al (2019) Remodeling of macular vortex veins in pachychoroid neovasculopathy. Sci Rep 9:14689. https://doi.org/10.1038/s41598-019-51268-9
Pang CE, Freund KB (2015) Pachychoroid neovasculopathy. Retina 35:1–9. https://doi.org/10.1097/IAE.0000000000000331
Wei WB, Xu L, Jonas JB et al (2013) Subfoveal choroidal thickness: the Beijing Eye Study. Ophthalmology 120:175–180. https://doi.org/10.1016/j.ophtha.2012.07.048
Barteselli G, Chhablani J, El-Emam S et al (2012) Choroidal volume variations with age, axial length, and sex in healthy subjects: a three-dimensional analysis. Ophthalmology 119:2572–2578. https://doi.org/10.1016/j.ophtha.2012.06.065
Hirata M, Tsujikawa A, Matsumoto A et al (2011) Macular choroidal thickness and volume in normal subjects measured by swept-source optical coherence tomography. Invest Ophthalmol Vis Sci 52:4971–4978. https://doi.org/10.1167/iovs.11-7729
Cheung CMG, Lee WK, Koizumi H et al (2019) Pachychoroid disease. Eye (Lond) 33(1):14–33. https://doi.org/10.1038/s41433-018-0158-4
Matsumoto K, Suehira N, Tomatsu N (2015) Tomographic imaging apparatus and photographing method. United States Patent 9149181 B2. https://ppubs.uspto.gov/pubwebapp/ Accessed 23 Oct 202
Touhami S, Philippakis E, Mrejen S et al (2020) Topographic variations of choroidal thickness in healthy eyes on swept-source optical coherence tomography. Invest Ophthalmol Vis Sci 61:38. https://doi.org/10.1167/iovs.61.3.38
Imanaga N, Terao N, Nakamine S et al (2021) Scleral thickness in central serous chorioretinopathy. Ophthalmol Retina 5:285–291. https://doi.org/10.1016/j.oret.2020.07.011
Imanaga N, Terao N, Sawaguchi S et al (2022) Clinical factors related to loculation of fluid in central serous chorioretinopathy. Am J Ophthalmol 235:197–203. https://doi.org/10.1016/j.ajo.2021.09.009
Spaide RF, Fisher YL, Ngo WK et al (2022) Regional scleral thickness as a risk factor for central serous chorioretinopathy. Retina 42(7):1231–1237. https://doi.org/10.1097/IAE.0000000000003485
Kuroda Y, Ooto S, Yamashiro K et al (2016) Increased choroidal vascularity in central serous chorioretinopathy quantified using swept-source optical coherence tomography. Am J Ophthalmol 169:199–207. https://doi.org/10.1016/j.ajo.2016.06.043
Spaide RF, Ryan EH Jr (2015) Loculation of fluid in the posterior choroid in eyes with central serous chorioretinopathy. Am J Ophthalmol 160:1211–1216. https://doi.org/10.1016/j.ajo.2015.08.018
Hayreh SS, Baines JA (1973) Occlusion of the vortex veins. An experimental study. Br J Ophthalmol 57:217–238. https://doi.org/10.1136/bjo.57.4.217
Kinoshita T, Mitamura Y, Shinomiya K et al (2017) Diurnal variations in luminal and stromal areas of choroid in normal eyes. Br J Ophthalmol 101(3):360–364. https://doi.org/10.1136/bjophthalmol-2016-308594
Acknowledgements
We are grateful to the orthoptists Masatoshi Tomita, Kikuko Toyodome, and the staff at the Kagoshima University Hospital for their support in the data collection process. We would like to thank Editage (www.editage.com) for English language editing.
Funding
This study was supported by JSPS KAKENHI (grant number 21H03095).
Author information
Authors and Affiliations
Contributions
Conception of design and conduct: RF, SS, HT, HS, NM, JH, TS, acquisition of the data: RF, NM, JH, management of data: RF, SS, NM, analysis of data: RF, SS, HS, JH, interpretation of the results: RF, SS, HT, HS, NM, JH, TS, preparation of articles: RF, HT, TS, and review and approval of the manuscript: RF, SS, HT, HS, NM, JH, TS.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the ethics committee of Kagoshima University, Kagoshima, Japan (No.16012). All the procedures were conducted in accordance with the tenets of the Declaration of Helsinki.
Conflict of interest
No conflicting relationships exist for any author.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Funatsu, R., Sonoda, S., Terasaki, H. et al. Choroidal morphologic features in central serous chorioretinopathy using ultra-widefield optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 261, 971–979 (2023). https://doi.org/10.1007/s00417-022-05905-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05905-1